Blunt chest trauma: is there a place for rib stabilization?
Rib fractures are a frequent occurrence in trauma victims, seen in up to 39% of patients following blunt chest trauma and present in 10% of all trauma admissions (1). While most cases are treated non-operatively, the presence of substantial chest wall trauma is associated with considerable morbidity and mortality. Patients with a “flail chest” pattern of injury, defined as two fractures per rib in three (or more) consecutive ribs, often struggle with hypoxemic respiratory failure related to inefficient ventilatory mechanics, underlying pulmonary contusion and subsequent pneumonia. In these individuals, mortality rates (even in the modern era) can reach 9–16% (2-4). For patients who survive, difficulties with chronic chest wall pain, deformity, longstanding disability and poor quality of life are common (5,6). Despite these well documented outcomes, treatment options for these patients remain poorly defined. A recent study utilizing the National Trauma Data Bank reported that fewer than 1% of patients with significant rib fractures underwent surgical stabilization, and that only 8% were treated with offered adequate pain control (4).
Can treatment protocols of early surgical stabilization, proactive pain control, and aggressive pulmonary toilet improve outcomes in this patient population? The answer seems to be “yes” (7), although the literature remains sparse in this field. In this brief article, we will review the indications for surgical intervention and the basic techniques and associated treatments involved in flail chest and significant rib injury.
Indications for surgery
The benefits of surgical stabilization have been best characterized for those patients with a flail segment. Three randomized clinical trials, as well as other cohort studies, demonstrate a reduced need for mechanical ventilation, less pneumonia, less pain, and reduced ICU stay in this population when early surgical intervention was performed (8-14). Three recent meta-analyses confirm these findings, and suggest a mortality benefit as well (15-17). The verdict has not been unanimous, though; at least two recent retrospective studies have failed to show a benefit to surgical stabilization in patients with flail segment (18,19). Others have demonstrated flaws in these dissenting studies, however, regarding methodology, timing of intervention, confounding injuries, and patient selection (7). It is likely, though, that optimal non-operative management (aggressive analgesia, pulmonary toilet, and ventilator strategies) may mitigate some of the benefits of early surgical intervention.
Indications for surgical intervention are listed in Table 1. Traditional contraindications to surgical stabilization have included the presence of a pulmonary contusion (22) and severe traumatic brain injury (TBI), although the nuances of the influence of lung and brain injury, over a broad spectrum, on the benefits of rib fixation have not been well studied.

Full table
Data for rib stabilization in non-flail segment patients is lacking. Two recent cohort studies (12,23) have demonstrated a benefit in these selected patients, although further study dedicated to this question is needed. Clearly, though, several of the indications described for surgical intervention may be present in non-flail segment patients.
Fracture assessment, non-operative treatment and timing of surgical intervention
Routine computed tomography (CT) of the chest has been found to be significantly more sensitive in detecting rib fractures compared with plain chest X-ray, although controversy exists as to the clinical significance. For example, Chapman et al. (24) noted that plain films missed about 75% of fractures diagnosed by CT; this led to changes in clinical management in 35% of patients. Other studies have found similar results (25,26). In contrast, several investigators noted that while CT is more sensitive, the additional information rarely was clinically significant (27,28). Finally, the use of three dimensional reconstruction in the diagnosis of rib fractures has limited utility compared to 2-D approaches, although this may change as technology advances (29).
Several scoring systems (30-32) have been devised to aid the clinician in assessing the severity of rib injury, typically incorporating the number, pattern and laterality of fractures, and the presence of other significant factors such as presence of a flail segment or pulmonary contusion. Higher scores are associated with poor outcomes, such as mortality, duration of mechanical ventilation, likelihood of pneumonia, etc. While useful in describing the severity of the fracture pattern present, there are limited data regarding the utility of these scoring systems in predicting the need or outcome of surgical intervention.
Optimizing pain control, pulmonary toilet, and ventilation strategies are incredibly important in this patient population, regardless of incorporation of surgical intervention in their treatment (7). Controversies exist regarding the best analgesic regimen; comparison studies fail to show clear benefit of regional techniques over other methods (33,34), although more work is needed in this area. Additionally, other injuries and clinical conditions (e.g., spinal injury or coagulopathy) must be taken into account when designing an analgesic regimen. Most experts agree, though, that a standardized protocol for pain control in blunt trauma patients is beneficial (7). In an analogous fashion, use of aggressive pulmonary toilet (chest physiotherapy, nasotracheal suctioning, mini-tracheostomy placement, etc.) and ventilator strategies (non-invasive ventilation, protective ventilation strategies, etc.) are crucial in the recovery of blunt chest trauma patients.
The timing of surgical stabilization following blunt chest trauma is felt to be important, with many investigators favoring early intervention within a few days of the primary injury (9,13,14,20,21,35-37). Rib fixation early in the patient’s hospital course avoids factors such as inflammation, severe hematoma, and early callous formation which can complicate operative reduction of the fractures. Of course, the timing of surgery must be made in the context of the patients overall clinical condition, and occasionally must be delayed while other injuries and conditions are stabilized.
Operative caveats
There are a number of caveats to surgical rib stabilization that should be understood prior to actively engaging in the treatment of these patients, and are well described in several excellent papers on the subject (35,36,38). Some described items are controversial, and require further study.
Mode of Fixation
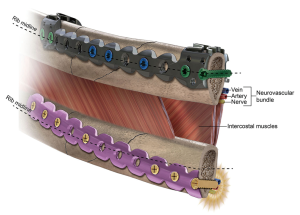
There are a number of hardware options for rib fixation currently offered, all of which have advantages and drawbacks. The dominant method currently used employs a plating system designed for placement on the outer cortex of the rib, secured with bicortical screws (Figures 1,2) (39). At least two centimeters of exposed rib on either side of the fracture are required to ensure adequate fixation. The majority of studies regarding rib fixation have used this technique, citing advantages of ease of use and adaptability to a variety of clinical situations. The external plates have been modified by one manufacturer with a “U”-shaped extension to fit over the cephalad aspect of the rib (Figure 3), allowing for uniform screw placement through the midportion of the rib; however, these require additional dissection for placement (40).


Recently, one company has developed an intramedullary strut, or splint, which allows for single point fixation per fracture (Figure 4) (41). This feature is theoretically attractive when a minimally invasive approach is contemplated, or difficult to expose fracture sites (e.g., posterior, subscapular) are addressed. Preliminary data suggest adequate healing using splints, although much more research is needed (42). Concerns have been raised in the literature by some investigators that the single point of fixation may allow distraction (separation of the bone) at the fracture site (7).

Bioabsorbable plating hardware has been available for many years, and is used primarily in areas of low load stress (e.g., face, cranium) to assist in bone healing. Absorbable plates amenable for rib fixation are also now available; made from poly-L-lactide, they are engineered to dissolve within 18–24 months (43). They may be cut to specific lengths, are malleable, and can be combined to provide additional length or rigidity (Figure 5). When used as indicated by the manufacturer, these plates are a bit less rigid, and allow for a bit more movement at the fracture site; as such, they may be poorly suited for reconstruction at areas of high load stress (44). However, the lack of complete rigidity at the fracture site may be advantageous through the concept of “stress shielding”, which postulates that some load stress is needed at the fracture to stimulate optimal bone regrowth. This load stress is often missing in completely rigid fixation associated with plate stabilization, but present to some degree with bioabsorbable or intramedullary splint repairs (45).

Surgical approach
Surgical rib stabilization has traditionally been accomplished through an open approach, and all significant series in the literature have used this method. The exact placement of incision(s) depends on the fracture pattern, the mode of fixation, and the other injuries present. A muscle-sparing approach is preferred.
A recent case report broached the subject of stabilization through a thoracoscopic approach (46), using a standard plating system modified to align with the inner cortex of the fractured ribs. This method allows access to virtually all rib segments typically addressed with surgical fixation, through minimally invasive incisions. While feasibility was demonstrated, widespread application of this approach will require availability of commercially available instrumentation.
Should all fractures be addressed?
This question can be framed in a variety of ways—for example: should both sides of a flail segment be stabilized, or just one side, converting the flail chest to simple fractures? Is stabilization of every other fracture as efficacious as fixation of every fracture? Can certain ribs be routinely excluded from consideration of repair? Selective fixation is faster, simpler, less expensive, and often less invasive. The question of selective versus complete rib stabilization has not been addressed in a scientific fashion, and expert opinion is divided on the subject (7,38,47,48). Most agree, though, that certain ribs can be excluded from stabilization efforts. Ribs 1 and 2 contribute minimally to respiratory function, and exposure to allow fixation at the chest apex can be challenging. In a similar vein, free floating ribs very low within the chest usually do not mandate repair.
Is surgical intervention cost-effective?
Several investigators have found early surgical rib stabilization in patients with blunt chest trauma to be more cost effective than non-operative treatment alone (13,17,49). The higher cost of the surgical intervention is more than offset by the decreased costs of subsequent care—less pneumonia, less respiratory failure, shorter ICU stay, etc. Further work in this area is needed.
Who will perform surgical rib stabilization?
Currently, a variety of surgical subspecialties participate in rib stabilization of blunt chest trauma patients—trauma (or acute care) surgeons, orthopedic trauma surgeons, and thoracic surgeons. Each subspecialty brings specific expertise to the care of these patients, and each is critical in a high functioning trauma unit. The trauma/acute care surgeons often are the attending of record, and have the best overall knowledge of the management of the poly-trauma patient. The orthopedic surgeons are perhaps most familiar with the hardware and instrumentation crucial to fracture fixation. Finally, the thoracic surgeons clearly are best acquainted with the anatomy of the chest wall, and are best equipped to deal with other intrathoracic pathology. However, the reality is that thoracic surgeons often delegate the care of these patients to others. It is incumbent for thoracic surgeons to maintain an active interest in this area of our specialty, lest it slip away to other able subspecialists; it is difficult to argue against the notion that the care of the chest trauma patient is optimized when dedicated thoracic surgeons are involved.
Acknowledgements
The author wishes to thank Fredric M. Pieracci, M.D., for assistance in preparing this manuscript.
Footnote
Conflicts of Interest: The author has no conflicts of interest to declare.
References
- Lafferty PM, Anavian J, Will RE, et al. Operative treatment of chest wall injuries: indications, technique, and outcomes. J Bone Joint Surg Am 2011;93:97-110. [Crossref] [PubMed]
- Athanassiadi K, Theakos N, Kalantzi N, et al. Prognostic factors in flail-chest patients. Eur J Cardiothorac Surg 2010;38:466-71. [Crossref] [PubMed]
- Cannon RM, Smith JW, Franklin GA, et al. Flail chest injury: are we making any progress? Am Surg 2012;78:398-402. [PubMed]
- Dehghan N, de Mestral C, McKee MD, et al. Flail chest injuries: a review of outcomes and treatment practices from the National Trauma Data Bank. J Trauma Acute Care Surg 2014;76:462-8. [Crossref] [PubMed]
- Fabricant L, Ham B, Mullins R, et al. Prolonged pain and disability are common after rib fractures. Am J Surg 2013;205:511-5; discussion 515-6. [Crossref] [PubMed]
- Marasco S, Lee G, Summerhayes R, et al. Quality of life after major trauma with multiple rib fractures. Injury 2015;46:61-5. [Crossref] [PubMed]
- Pieracci FM, Majercik S, Ali-Osman F, et al. Consensus statement: Surgical stabilization of rib fractures rib fracture colloquium clinical practice guidelines. Injury 2017;48:307-21. [Crossref] [PubMed]
- Doben AR, Eriksson EA, Denlinger CE, et al. Surgical rib fixation for flail chest deformity improves liberation from mechanical ventilation. J Crit Care 2014;29:139-43. [Crossref] [PubMed]
- Granetzny A, Abd El-Aal M, Emam E, et al. Surgical versus conservative treatment of flail chest. Evaluation of the pulmonary status. Interact Cardiovasc Thorac Surg 2005;4:583-7. [Crossref] [PubMed]
- Majercik S, Wilson E, Gardner S, et al. In-hospital outcomes and costs of surgical stabilization versus nonoperative management of severe rib fractures. J Trauma Acute Care Surg 2015;79:533-8; discussion 538-9. [Crossref] [PubMed]
- Marasco SF, Davies AR, Cooper J, et al. Prospective randomized controlled trial of operative rib fixation in traumatic flail chest. J Am Coll Surg 2013;216:924-32. [Crossref] [PubMed]
- Pieracci FM, Lin Y, Rodil M, et al. A prospective, controlled clinical evaluation of surgical stabilization of severe rib fractures. J Trauma Acute Care Surg 2016;80:187-94. [Crossref] [PubMed]
- Tanaka H, Yukioka T, Yamaguti Y, et al. Surgical stabilization of internal pneumatic stabilization? A prospective randomized study of management of severe flail chest patients. J Trauma 2002;52:727-32; discussion 732. [Crossref] [PubMed]
- Wada T, Yasunaga H, Inokuchi R, et al. Effectiveness of surgical rib fixation on prolonged mechanical ventilation in patients with traumatic rib fractures: A propensity score-matched analysis. J Crit Care 2015;30:1227-31. [Crossref] [PubMed]
- Leinicke JA, Elmore L, Freeman BD, et al. Operative management of rib fractures in the setting of flail chest: a systematic review and meta-analysis. Ann Surg 2013;258:914-21. [Crossref] [PubMed]
- Slobogean GP, MacPherson CA, Sun T, et al. Surgical fixation vs nonoperative management of flail chest: a meta-analysis. J Am Coll Surg 2013;216:302-11.e1. [Crossref] [PubMed]
- Swart E, Laratta J, Slobogean G, et al. Operative Treatment of Rib Fractures in Flail Chest Injuries: A Meta-analysis and Cost-Effectiveness Analysis. J Orthop Trauma 2017;31:64-70. [Crossref] [PubMed]
- DeFreest L, Tafen M, Bhakta A, et al. Open reduction and internal fixation of rib fractures in polytrauma patients with flail chest. Am J Surg 2016;211:761-7. [Crossref] [PubMed]
- Farquhar J, Almahrabi Y, Slobogean G, et al. No benefit to surgical fixation of flail chest injuries compared with modern comprehensive management: results of a retrospective cohort study. Can J Surg 2016;59:299-303. [Crossref] [PubMed]
- Althausen PL, Shannon S, Watts C, et al. Early surgical stabilization of flail chest with locked plate fixation. J Orthop Trauma 2011;25:641-7. [Crossref] [PubMed]
- Pieracci FM, Rodil M, Stovall RT, et al. Surgical stabilization of severe rib fractures. J Trauma Acute Care Surg 2015;78:883-7. [Crossref] [PubMed]
- Voggenreiter G, Neudeck F, Aufmkolk M, et al. Operative chest wall stabilization in flail chest--outcomes of patients with or without pulmonary contusion. J Am Coll Surg 1998;187:130-8. [Crossref] [PubMed]
- Majercik S, Cannon Q, Granger SR, et al. Long-term patient outcomes after surgical stabilization of rib fractures. Am J Surg 2014;208:88-92. [Crossref] [PubMed]
- Chapman BC, Overbey DM, Tesfalidet F, et al. Clinical Utility of Chest Computed Tomography in Patients with Rib Fractures CT Chest and Rib Fractures. Arch Trauma Res 2016;5:e37070. [Crossref] [PubMed]
- Brink M, Deunk J, Dekker HM, et al. Added value of routine chest MDCT after blunt trauma: evaluation of additional findings and impact on patient management. AJR Am J Roentgenol 2008;190:1591-8. [Crossref] [PubMed]
- Traub M, Stevenson M, McEvoy S, et al. The use of chest computed tomography versus chest X-ray in patients with major blunt trauma. Injury 2007;38:43-7. [Crossref] [PubMed]
- Kea B, Gamarallage R, Vairamuthu H, et al. What is the clinical significance of chest CT when the chest x-ray result is normal in patients with blunt trauma? Am J Emerg Med 2013;31:1268-73. [Crossref] [PubMed]
- Livingston DH, Shogan B, John P, et al. CT diagnosis of Rib fractures and the prediction of acute respiratory failure. J Trauma 2008;64:905-11. [Crossref] [PubMed]
- Pulley BR, Taylor BC, Fowler TT, et al. Utility of three-dimensional computed tomography for the surgical management of rib fractures. J Trauma Acute Care Surg 2015;78:530-4. [Crossref] [PubMed]
- Chapman BC, Herbert B, Rodil M, et al. RibScore: A novel radiographic score based on fracture pattern that predicts pneumonia, respiratory failure, and tracheostomy. J Trauma Acute Care Surg 2016;80:95-101. [Crossref] [PubMed]
- Chen J, Jeremitsky E, Philp F, et al. A chest trauma scoring system to predict outcomes. Surgery 2014;156:988-93. [Crossref] [PubMed]
- Pressley CM, Fry WR, Philp AS, et al. Predicting outcome of patients with chest wall injury. Am J Surg 2012;204:910-3; discussion 913-4. [Crossref] [PubMed]
- Duch P, Møller MH. Epidural analgesia in patients with traumatic rib fractures: a systematic review of randomised controlled trials. Acta Anaesthesiol Scand 2015;59:698-709. [Crossref] [PubMed]
- Yeh DD, Kutcher ME, Knudson MM, et al. Epidural analgesia for blunt thoracic injury--which patients benefit most? Injury 2012;43:1667-71. [Crossref] [PubMed]
- Gasparri MG, Tisol WB, Haasler GB. Rib stabilization: lessons learned. Eur J Trauma Emerg Surg 2010;36:435-40. [Crossref] [PubMed]
- Sarani B, Schulte L, Diaz JJ. Pitfalls associated with open reduction and internal fixation of fractured ribs. Injury 2015;46:2335-40. [Crossref] [PubMed]
- Nirula R, Diaz JJ Jr, Trunkey DD, et al. Rib fracture repair: indications, technical issues, and future directions. World J Surg 2009;33:14-22. [Crossref] [PubMed]
- Mayberry J. Surgical stabilization of severe rib fractures: Several caveats. J Trauma Acute Care Surg 2015;79:515. [Crossref] [PubMed]
- Available online: http://sites.synthes.com/intl/matrixrib/resources/Pages/features.aspx
- Available online: https://acuteinnovations.wefoster-platform.co/wp-content/uploads/2017/01/RBL7005B_U-Plus-brochure1.pdf
- Available online: https://emea.depuysynthes.com/hcp/cmf/products/qs/matrixrib-fixation-system
- Marasco S, Quayle M, Summerhayes R, et al. An assessment of outcomes with intramedullary fixation of fractured ribs. J Cardiothorac Surg 2016;11:126. [Crossref] [PubMed]
- Available online: http://acuteinnovations.com/Products/BioBridge
- Marasco SF, Sutalo ID, Bui AV. Mode of failure of rib fixation with absorbable plates: a clinical and numerical modeling study. J Trauma 2010;68:1225-33. [Crossref] [PubMed]
- Becker G, Calvis A, Hazlett L, et al. Bioabsorbable polymeric fracture fixation devices aim to reduce stress shielding in bone. In 2014 40th Annual Northeast Bioengineering Conference (NEBEC), 2014.
- Pieracci FM, Johnson JL, Stovall RT, et al. Completely thoracoscopic, intra-pleural reduction and fixation of severe rib fractures. Trauma Case Reports 2015;1:39-43. [Crossref]
- Nickerson TP, Thiels CA, Kim BD, et al. Outcomes of Complete Versus Partial Surgical Stabilization of Flail Chest. World J Surg 2016;40:236-41. [Crossref] [PubMed]
- Marasco S, Liew S, Edwards E, et al. Analysis of bone healing in flail chest injury: do we need to fix both fractures per rib? J Trauma Acute Care Surg 2014;77:452-8. [Crossref] [PubMed]
- Bhatnagar A, Mayberry J, Nirula R. Rib fracture fixation for flail chest: what is the benefit? J Am Coll Surg 2012;215:201-5. [Crossref] [PubMed]


