A case of video-assisted thoracoscopic resection of malignant transformation of pulmonary recurrent respiratory papillomatosis
Introduction
Recurrent respiratory papillomatosis (RRP) is a disease caused by infection with the human papillomavirus (HPV) characterized by multiple recurring papillomas throughout the respiratory tract (1). Extra laryngeal involvement is rare, with tracheal or proximal bronchial lesions appearing in only 5% of cases and pulmonary involvement in 3% of cases (2,3). The risk of malignant transformation is approximately 3–7% in adults, and is associated mainly with HPV serotypes 6 and 11 (4,5). Treatment for RRP consists of repeated local treatments with laser therapy and/or surgical debulking as well as possible adjunctive medical therapy with cidofovir, an inhibitor of viral DNA polymerase (1,6). We describe a case of unmonitored juvenile onset RRP with subsequent pulmonary involvement and malignant transformation to squamous cell carcinoma (SCC), treated with a thoracoscopic lobectomy and mediastinal lymph node dissection.
Case presentation
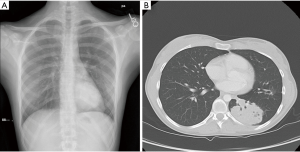
The patient is an 18-year-old woman with a history of juvenile onset RRP requiring multiple local resections in her upper airway as a child. She had received multiple HPV vaccinations from 2008–2012 and at the time of presentation to a thoracic surgeon she had not undergone any intervention for approximately 10 years. She presented after undergoing a chest X-ray after mild chest wall trauma, which demonstrated a new left lower lobe mass (Figure 1A). At that time she was asymptomatic, with no chest pain, cough, hemoptysis or shortness of breath. A subsequent chest CT demonstrated a 5.6 cm × 5.0 cm × 7.1 cm soft tissues mass in the left lower lobe (Figure 1B). A percutaneous biopsy of the mass showed squamous neoplasm with papillomatosis features. A PET scan showed a large hypermetabolic mass as well as a prominent left precarinal lymph node with mild hypermetabolic activity. After discussions with our multidisciplinary tumor board and the patient, it was decided to pursue surgical resection of this mass with concurrent mediastinal lymph node dissection.
Perioperative bronchoscopy was negative for upper airway masses. A video assisted thoracoscopic left lower lobectomy was performed with mediastinal lymph node dissection. The patient tolerated the procedure well and was discharged from the hospital on postoperative day 2. Final surgical pathology revealed a 10 cm × 9 cm × 7 cm (Figure 2) focally keratinizing SCC in a background of invasive respiratory papillomatosis without pleural invasion. Surgical margins were negative; however, lymph nodes in stations 7 and 9 were positive for metastatic disease. Her pathologic stage was pT3N2, with a clinical stage of IIIA. Now one year after her surgery, she is status post four cycles of adjuvant chemotherapy with carboplatin and paclitaxel as well as 5,000 cGy adjuvant mediastinal radiation which she tolerated well and has returned to normal living. Post-operative surveillance CT showed no progression of disease at 6 months and she will undergo another surveillance CT scan in 6 months.

Discussion
Pulmonary spread of RRP is a rare phenomenon, occurring in approximately 3% of patients, and is associated with malignant degeneration with a measured rate of 16% in a systematic review of 1,666 patients (3). Specific risk factors for malignant degeneration are not yet characterized, though younger age at diagnosis and HPV-11 serotype have been identified as risk factors for overall disease severity (7). There is currently no clear consensus on the timing and form that surveillance of RRP should take. Knepper et al. recently advocated for surveillance imaging with either chest radiographs or CT scanning, with the addition of FDG PET/CT for any concerning findings found on screening images (8).
Treatment of pulmonary involvement of RRP consists of either anatomical surgical resection of known disease, or immunotherapy. Despite the inability of these therapeutic options to provide a definitive cure for pulmonary spread, routine screening of the chest clearly has a critical role in the management of RRP. Had our patient undergone surveillance imaging of any form in the 10 years preceding her operation, it is likely that the pulmonary spread of her disease would have been diagnosed prior to either its malignant degeneration or the lymphatic spread of her disease. Such screening would reduce the risk of requiring adjuvant chemo-radiation after definitive surgical resection. To this end, we advocate for all patients with RRP to undergo yearly imaging screening. Based on the current level of evidence, this screening may consist of either chest radiographs or CT scans.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
References
- Carifi M, Napolitano D, Morandi M, et al. Recurrent respiratory papillomatosis: current and future perspectives. Ther Clin Risk Manag 2015;11:731-8. [Crossref] [PubMed]
- Can NT, Tretiakova MS, Taxy JB. Natural History and Malignant Transformation in Recurrent Respiratory Papillomatosis: Human Papillomavirus (HPV), Dysplasia and an Autopsy Review. Fetal Pediatr Pathol 2015;34:80-90. [Crossref] [PubMed]
- Gélinas JF, Manoukian J, Côté A. Lung involvement in juvenile onset recurrent respiratory papillomatosis: a systematic review of the literature. Int J Pediatr Otorhinolaryngol 2008;72:433-52. [Crossref] [PubMed]
- Lee LA, Cheng AJ, Fang TJ, et al. High incidence of malignant transformation of laryngeal papilloma in Taiwan. Laryngoscope 2008;118:50-5. [Crossref] [PubMed]
- Sajan JA, Kerschner JE, Merati AL, et al. Prevalence of dysplasia in juvenile-onset recurrent respiratory papillomatosis. Arch Otolaryngol Head Neck Surg 2010;136:7-11. [Crossref] [PubMed]
- Taliercio S, Cespedes M, Born H, et al. Adult-onset recurrent respiratory papillomatosis: a review of disease pathogenesis and implications for patient counseling. JAMA Otolaryngol Head Neck Surg 2015;141:78-83. [Crossref] [PubMed]
- Karatayli-Ozgursoy S, Bishop JA, Hillel A, et al. Risk Factors for Dysplasia in Recurrent Respiratory Papillomatosis in an Adult and Pediatric Population. Ann Otol Rhinol Laryngol 2016;125:235-41. [Crossref] [PubMed]
- Knepper BR, Eklund MJ, Braithwaite KA. Malignant degeneration of pulmonary juvenile-onset recurrent respiratory papillomatosis. Pediatr Radiol 2015;45:1077-81. [Crossref] [PubMed]


