Gender differences in cardiovascular risk factors in patients with coronary artery disease and those with type 2 diabetes
The incidence of cardiovascular disease is known to be higher in men than in women of similar age, and this gender difference is more prominent at a younger age (1) and is partly explained by protective effects of sex hormones (2). On the other hand, female patients with coronary artery disease have been reported to be more likely to have a worse cardiovascular risk factor profile (3,4).
The EUROASPIRE IV is a cross-sectional survey on hospitalized patients with coronary artery disease (n=7,998; ages of 18–80 years) including centers from 24 European countries. De Smedt et al. analyzed the data of this survey and demonstrated that prevalence of multiple cardiovascular risk factors (3 or more from 5 risk factors including smoking, obesity, high blood pressure, high LDL cholesterol and diabetes) was significantly higher in female patients than in male patients (4). In the former study by the authors’ group (EUROASPIRE III study), the prevalence of each of the risk factors including obesity, high blood pressure, high LDL cholesterol and diabetes was shown to be higher in female patients with coronary artery disease than in male patients (3). Interestingly, the gender difference in the prevalence of multiple cardiovascular risk factors was more prominent in elderly patients (≥70 years) and patients with a lower level of education (4), although it was not shown whether and how the relation of each risk factor to gender was influenced by age or education. There was no significant three-way (gender, age and education) interaction with multiple risk factors. In overall subjects, women were 3.1 years older than men, and this possibly influences the relationship of gender with cardiovascular risk factors, although age as well as education was adjusted in the analysis. It was not shown whether and how mean age differs in men and women of the younger group (<70 years) or older (≥70 years) group. In addition to the gender difference in risk factors, a gender difference was found in the control (target achievement) of cardiovascular risk factors: Regarding LDL cholesterol, glycemic status, adiposity and physical activity as targets, the proportion of subjects who achieved each target was lower in female patients than in male patients, and interactions by age and education were observed in LDL cholesterol and adiposity, respectively, as targets. However, in lifestyle changes and risk factor awareness, no significant gender differences were found except for less women having had a weight measurement since hospital discharge and worse awareness rate among women regarding their waist if centrally obese. Therefore, the gender differences in target achievement for LDL cholesterol, blood pressure and hemoglobin A1c are unlikely to be due to differences in lifestyle changes and risk factor awareness. The difference between the individual value of each risk factor and its target should be greater in female patients than in male patients. Therefore, there is a possibility that the status of each risk factor is associated with its target achievement, although the method for evaluation of target achievement was not described in the article. The gender gap in the opportunity for education is becoming smaller, and thus the authors speculated that this explains a smaller gender difference in younger patients than in elderly patients and that the gender difference will decrease in the future. As possible reasons for the gender difference in accumulation of risk factors, the authors gave some explanations including later diagnosis of coronary artery disease and consequent greater clustering of risk factors, less opportunity for optimal treatment, lower magnitude of lifestyle changes, less professional activities, and higher prevalences of anxiety and depression in women than in men (4). The high risk factor burden hypothesis and healthy survivor effects were also raised as possible reasons for the gender difference in cardiovascular risk factors in patients with coronary artery disease (4).
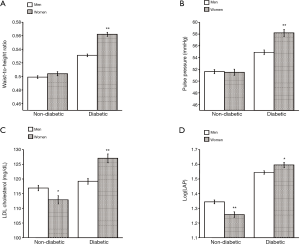
Regarding patients with diabetes mellitus, it has also been shown that female patients have a higher cardiovascular risk than do male patients (5), and this may be in part explained by a more adverse cardiometabolic profile including visceral obesity, hypertension and dyslipidemia in women with diabetes (6-9). In a previous study, I demonstrated that female subjects with diabetes (n=569; mean age, 53.8±7.4 years) had a more adverse cardiometabolic profile than did age-matched male subjects with diabetes (n=1,138) (9). Waist-to-height ratio (WHtR), pulse pressure, LDL cholesterol, and log-transformed lipid accumulation product (LAP) were compared between men and women with and without diabetes who were 35 to 70 years old (Figure 1). In the non-diabetic group, LDL cholesterol and log-transformed LAP were higher in men than in women, while WHtR and pulse pressure were comparable in men and women. On the other hand, in the diabetic group, WHtR, pulse pressure, LDL cholesterol and log-transformed LAP were all higher in women than in men. Pulse pressure reflects arterial stiffness, which is a potent cardiovascular risk factor (10). Obesity is a major risk factor for type 2 diabetes, and dyslipidemia is known to be closely associated with diabetes. LAP, an index calculated by using levels of serum triglycerides and waist circumference, has been reported to be a good discriminator for diabetes (11). Therefore, female patients with diabetes had a more adverse profile of cardiovascular risk factors than did male patients, whereas women without diabetes had a better profile of risk factors than did men. Regarding the gender difference in cardiovascular risk factors, the above findings on diabetes agree with those of the previous studies on coronary artery disease (3,4). In the above study on diabetes, the subjects were 70 years old or younger and their ages were matched in men and women in the diabetic and non-diabetic groups (9), and thus the gender difference is not related to age. Information on education level of subjects was unfortunately not available, but all of the subjects were workers, and results for their annual health checkups at the workplaces were analyzed in the above study on diabetes (9). Therefore, it is unlikely that there is a great difference in education levels in male and female subjects with diabetes in the study. The ability to convert androgen to estrogen was reported to be impaired in women with type 2 diabetes, and this impairment is likely to be caused by attenuation of ovarian aromatase activity (12). Thus, protective actions of estrogen on cardiovascular health, including suppression of obesity and dyslipidemia, may be decreased in female patients with diabetes compared with those in non-diabetic women. However, the reason for a more adverse cardiovascular profile in female patients with diabetes than in male patients remains unknown. Type 2 diabetes has been shown to be more common in men than in women in many studies (5). Men develop diabetes at a lower body mass index and are more insulin-resistant (13). In a cross-sectional study of non-diabetic and diabetic men and women, advantages of women such as a better profile of risk factors and less insulin resistance than those in men were diminished in a diabetic state, and the interactions of gender and diabetes for diastolic blood pressure, tissue plasminogen, white blood cell count and coagulation factor VIII were attenuated after adjustment for waist circumference and HOMA-IR (14). Thus, it was thought that the greater adverse influence of diabetes on cardiovascular risk factors was, to some degree, explained by the greater increases in adiposity and insulin resistance associated with diabetes in women than in men. Therefore, the gender difference in cardiovascular risk factors in patients with diabetes may be at least partly explained by a higher risk factor burden (15): women who develop diabetes are more prone to have disadvantages in their backgrounds, such as obesity and insulin resistance, that deteriorate glucose tolerance. In addition, gender differences regarding diagnosis and therapy for diabetes, including later diagnosis, less diagnostic and therapeutic supports, and less attainment of therapeutic goals in women, have been suggested as reasons for gender differences in diabetic complications (16).
A more adverse profile of cardiovascular risk factors in women than in men is found both in patients with coronary artery disease and patients with diabetes. Common reasons are speculated for these gender differences. Sufficient medical care including lifestyle modification and medication therapy for correcting cardiovascular risk factors is needed in order to prevent cardiovascular complications in women with diabetes and to reduce recurrent events in female patients with coronary artery disease.
Acknowledgements
None.
Footnote
Conflicts of Interest: The author has no conflicts of interest to declare.
References
- Kannel WB, Hjortland MC, McNamara PM, et al. Menopause and risk of cardiovascular disease: the Framingham study. Ann Intern Med 1976;85:447-52. [Crossref] [PubMed]
- Vitale C, Fini M, Speziale G, et al. Gender differences in the cardiovascular effects of sex hormones. Fundam Clin Pharmacol 2010;24:675-85. [Crossref] [PubMed]
- Dallongevillle J, De Bacquer D, Heidrich J, et al. Gender differences in the implementation of cardiovascular prevention measures after an acute coronary event. Heart 2010;96:1744-9. [Crossref] [PubMed]
- De Smedt D, De Bacquer D, De Sutter J, et al. The gender gap in risk factor control: Effects of age and education on the control of cardiovascular risk factors in male and female coronary patients. The EUROASPIRE IV study by the European Society of Cardiology. Int J Cardiol 2016;209:284-90. [Crossref] [PubMed]
- Emerging Risk Factors Collaboration, Sarwar N, Gao P, et al. Diabetes mellitus, fasting blood glucose concentration, and risk of vascular disease: a collaborative meta-analysis of 102 prospective studies. Lancet 2010;375:2215-22. [Crossref] [PubMed]
- Walden CE, Knopp RH, Wahl PW, et al. Sex differences in the effect of diabetes mellitus on lipoprotein triglyceride and cholesterol concentrations. N Engl J Med 1984;311:953-9. [Crossref] [PubMed]
- Howard BV, Cowan LD, Go O, et al. Adverse effects of diabetes on multiple cardiovascular disease risk factors in women. The Strong Heart Study. Diabetes Care 1998;21:1258-65. [Crossref] [PubMed]
- Hypertension in Diabetes Study (HDS). I. Prevalence of hypertension in newly presenting type 2 diabetic patients and the association with risk factors for cardiovascular and diabetic complications. J Hypertens 1993;11:309-17. [Crossref] [PubMed]
- Wakabayashi I. Gender-related differences in cardiometabolic risk profile of Japanese patients with diabetes. J Womens Health (Larchmt) 2014;23:1046-53. [Crossref] [PubMed]
- Safar ME. Systolic blood pressure, pulse pressure and arterial stiffness as cardiovascular risk factors. Curr Opin Nephrol Hypertens 2001;10:257-61. [Crossref] [PubMed]
- Kahn HS. The lipid accumulation product is better than BMI for identifying diabetes: a population-based comparison. Diabetes Care 2006;29:151-3. [Crossref] [PubMed]
- Stamataki KE, Spina J, Rangou DB, et al. Ovarian function in women with non-insulin dependent diabetes mellitus. Clin Endocrinol (Oxf) 1996;45:615-21. [Crossref] [PubMed]
- Sattar N. Gender aspects in type 2 diabetes mellitus and cardiometabolic risk. Best Pract Res Clin Endocrinol Metab 2013;27:501-7. [Crossref] [PubMed]
- Wannamethee SG, Papacosta O, Lawlor DA, et al. Do women exhibit greater differences in established and novel risk factors between diabetes and non-diabetes than men? The British Regional Heart Study and British Women's Heart Health Study. Diabetologia 2012;55:80-7. [Crossref] [PubMed]
- Andreotti F, Marchese N. Women and coronary disease. Heart 2008;94:108-16. [Crossref] [PubMed]
- Seghieri G, Policardo L, Anichini R, et al. The effect of sex and gender on diabetic complications. Curr Diabetes Rev 2016. [Epub ahead of print]. [PubMed]


