Pressure-controlled versus volume-controlled ventilation during one-lung ventilation for video-assisted thoracoscopic lobectomy
Introduction
Respiratory complications especially postoperative acute lung injury (ALI) is the main cause of morbidity and mortality after thoracic surgery with one-lung ventilation (OLV) (1). In order to decrease the incidence of ALI after OLV and to prevent the respiratory complications after thoracic surgery, protective ventilation [PV; mainly including VTs of 6 mL/predicted body weight (PBW) and positive end-expiratory pressure (PEEP) of 5 cmH2O] is recommended during OLV (2,3).
For a long time, small VT was believed to be more benefit than large one. The most convincing data was from Dr. Yang (4) which showed that pressure controlled ventilation (PCV) with low VT (6 mL/kg) was associated with lower incidence of postoperative lung dysfunction than volume controlled ventilation (VCV) with large VT (10 mL/kg). In 2007, Schultz et al. (5) published recommendations on intraoperative VT and suggested utilizing lower VT (≤6 mL/kg) in patients with abnormal lungs and/or risk factors for ALI.
With further studying of small VT ventilation, some new findings came out. Blum et al. (6) showed that the incidence of postoperative ARDS was 0.2% in a general surgical population and the intraoperative risk factor included driver pressure instead of low tide volume. In thoracic surgery, the expected incidence of postoperative ALI was as high as 4.2% (7) and the independent risk factors included intraoperative ventilatory pressure index instead of VT. Fernández-Pérez et al. (8) designed a study to prove their hypothesis that higher VT would be associated with higher risk of respiratory failure secondary to ALI, but the result showed that mean first hour peak airway pressure but not VT was associated with ALI. The clinical researches above made us reconsider to utilize the ventilation mode with lower airway pressure during high risk operations especially thoracic surgeries with obligated OLV.
Song et al. (9) compared volume-controlled versus pressure-controlled ventilation-volume guaranteed mode (PCV-VG) during OLV. The result showed that in patients with normal lung function the airway pressure was lower in PCV-VG than that in VCV while the arterial oxygen tension remained the same. Lin et al. (10) also compared three different ventilation modes (VCV, PCV and PCV-VG) during OLV in elderly patients. It showed that the airway pressure and PaO2 were both improved in PCV and PCV-VG group compared to VCV.
Unfortunately neither studied presented the postoperative data and furthermore the VTs were set to 8 mL/kg which was not fulfilled the criteria of PV during OLV nowadays. No data of oxygenation index which is an important index of ALI was given in these studies. So we designed this study to investigate the difference of PCV and VCV mode on the peak inspiratory airway pressure (Ppeak), Pplat during OLV and oxygenation index intra- and post-operative.
Methods
General design
This is a single center, single blinded prospective study on two different ventilation modes during one lung ventilation for patients undergoing video-assisted thoracoscopic lobectomy. The study was approved by institutional ethics committee of Zhongshan Hospital, Fudan University (No. B2012-064) and was registered in ClinicalTrails.gov under the number NCT03061617. After written informed consents were obtained, 70 patients with primary lung cancer undergo video-assisted thoracoscopic lobectomy in Zhongshan Hospital were enrolled and randomized into two groups: VCV group (group V) or PCV group (group P).
Inclusion criteria were age between 18–75 years, ASA I–II, lateral decubitus position with at least 1 h OLV and preoperative FEV1 >50% predicted. Preoperative exclusion criteria were previous lobectomy, COPD, asthma, uncompensated cardiac disease or contraindications for epidural catheter. Intraoperative exclusion criteria were SpO2 under 90% after intratracheal suction, reconfirmation the position of double lumen tracheal tube (DLT) and recruitment maneuver of dependant lungs.
Protocol
Epidural catheters were placed at T6–7 intervertebral spaces before induction and analgesia effect was confirmed using 5 mL 1% lidocaine. Patients were induced by propofol (target-controlled infusion, Ce =2.5 µg/mL), fentanyl (2 µg/kg), remifentanil (0.2 µg/kg/min) and rocuronium (0.6 mg/kg). DLT was intubated and fiberoptic bronchoscopy was used to confirm its position. Anesthesia was maintained with propofol (Ce =3–4 µg/mL), fentanyl and rocuronium. In each patient, 10 mL 0.15% ropivacaine was used epidurally as loading dose and 5 mL was added every 1 h after induction.
The ventilation setting during two-lung ventilation is as follows: VT 8 mL/kg, f 10 breaths/min, PEEP 0 cmH2O. And the goals of hemodynamic management during our study were the same as other surgeries in our center which was within ±20% of the baseline.
In Group V, OLV was performed using VCV mode with Vt =6 mL/kg, PEEP 5 cmH2O. In Group P, OLV was performed using PCV mode with PEEP 5 cmH2O, Ppeak/Pplat adjusted to achieve Vt =6 mL/kg. In each case, respiratory rate was adjusted to maintain EtCO2 35–45 mmHg and FiO2 was increased from 50% to achieve SpO2 over 90%. Patients were extubated and transferred to PACU after surgery.
Ppeak, Pplat, respiratory rate and VT were recorded at 15 min (T1), 1 h (T2) after the beginning of OLV and at the end of OLV (T3). Arterial gas analysis were performed preoperatively with room air (T0) and at T1, T2, T3, 30 min after PACU admission (T4), post-operative day 1 (POD1) and day 2 (POD2).
Duration of surgery, intraoperative blood loss, intraoperative urine output, intraoperative fluid infusion were recorded as well as pulmonary complication, cardiovascular complication and others.
Statistical analysis
The quantitative data were expressed as mean and standard deviation. The categorical data were expressed as number of cases and percentage of the total. Student’s t-test or the Mann-Whitney test was used for quantitative data. Fischer exact test was used to compare qualitative data. A value of P<0.05 was considered significant. According to the results of Pu’s study (11), 35 subjects per group allowed detection of a 50 mmHg reduction in PaO2 (FiO2 100) during OLV with α=0.05 and a 90% power.
Results
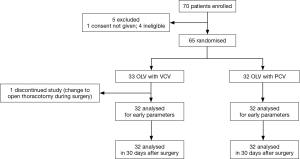
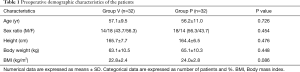
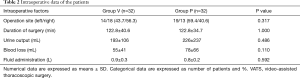
Seventy patients were enrolled in this study and sixty-four completed it (see flow chart in Figure 1). All the demographic data are shown in Table 1. All the surgery related data are presented in Table 2. There were no difference with demographic features and surgery related factors between these two groups.
Full table
Full table
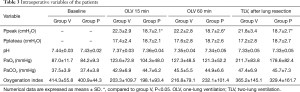
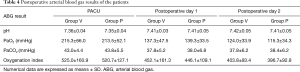
Intraoperative variables are shown in Table 3. Gas analysis results of arterial blood sample at T0, T1, T2 and T3 were presented as well as the ventilation parameters. There were no differences with arterial blood gas analysis results (i.e., pH, PaO2, PaCO2) between these two groups. Ppeak in group P was lower than that in group V at any time point during OLV. As to oxygenation index, we did not find any difference between these two groups not only during operation but also in postoperative period. We followed up arterial blood gas for two days after operations and no difference was showed up (Table 4).
Full table
Full table
After 30 days’ follow-up, no difference was found in pulmonary, cardiovascular and other complications between them. The numbers of postoperative pneumonia cases were 2 and 1 in group V and group P respectively. There was one case of respiratory failure in group V due to surgery related problem and reintubation was happened to this case (Table 5).
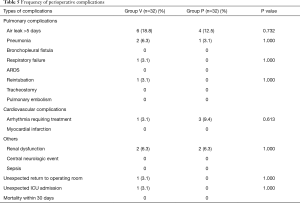
Full table
Discussion
Our results showed that during OLV in patients under video-assisted thoracoscopic lobectomy, the performance of PCV mode was superior to VCV in Ppeak during OLV but not the intra- nor post-operative oxygenation index. There was no difference with pulmonary or cardiovascular complications between these two modes.
The strategy of OLV went from large volume ventilation (same VT as two lung ventilation) to small volume ventilation with appropriate PEEP (5 cmH2O). Low VT ventilation is widely known as PV especially in ARDS (12).
High airway pressure associated with mechanical ventilation is thought to be the main risk of ventilator related lung injury (13). According to the result from Licker et al. (7), there were four independent factors for primary ALI: high intraoperative ventilatory pressure, excessive fluid infusion, pneumonectomy and preoperative alcohol abuse. Among these four factors what we anesthesiologist can intervene was to optimize the intraoperative ventilatory pressure and limit intraoperative fluid infusion. In this study we focused on the intraoperative ventilatory pressure and we wanted to figure out the difference of patients’ outcome between two commonly used ventilator modes during OLV.
PCV was always used to avoid higher airway pressure and provide better oxygenation (14). From previous studies we found that the controversy on better performance of PCV over VCV really existed. So we designed this study to figure out whether PCV had better performance on intra- and post-operative oxygenation and postoperative pulmonary complications in low risk patient during OLV.
Because the VTs in PCV are highly variable (15), we adjusted ventilation pressure to maintain the same volume during OLV so that we can balanced the volume related lung injury (volutrauma). The modified PCV ventilation we adopted here was similar with PCV-VG which was utilized in some recent papers (9,10). PCV-VG is the newest ventilation mode in anesthesia machine (16). It delivers the preset VT with the lowest possible pressure. Unfortunately in our center we did not have such new mode in our anesthesia machine, so we adjusted the pressure manually to obtain the same volume as PCV-VG did.
PCV generates a square pressure waveform with a decelerating inspiratory flow pattern which leads to a more even distribution of VT, recruitment of insufficiently ventilated lung units and oxygenation improvement (14,17,18). Additionally, the rapid alveolar inflation caused by the high initial flow rate in PCV can avoid regional overdistension and lead to better ventilation perfusion matching (19). Though there were a few studies compared PCV and VCV mode during OLV, but very few had evaluated the oxygenation index and postoperative lung complications between these two ventilation modes especially under PV strategy which is highly recommended during OLV.
It was Pplat not Ppeak which was strongly correlated with barotrauma (20). From our study there was no difference with Pplat and also no difference in pulmonary complications though the Ppeak was higher in group V. All the airway pressure were under the recommended range with Ppeak under 35 cmH2O and Pplat under 25 cmH2O (21,22).
The first study of PCV-VG (11) and following studies on OLV in thoracic surgery (9) showed that PCV-VG provided better oxygenation and lower airway pressure, but unfortunately they did not compare the postoperative complications and prognosis. Our study not only focused on the intraoperative performance of these two ventilation modes but also during postoperative period. Our result showed that PCV really had lower Ppeak as previous studies suggested but the oxygenation index of two groups were similar intraoperatively and post-operatively.
And also there were no difference with any postoperative complications between these two groups in present study. The result of our study was consistence with the recent meta-analysis on intraoperative mechanical ventilation strategies in patients undergoing one lung ventilation (23). In this meta-analysis, they suggested that PV but not pressure-controlled ventilation can decrease the incidence of PPCs (postoperative pulmonary complications). PCV and VCV had similar effect on PPCs. Our randomized controlled perspective study suggested that under the condition of low VT and proper PEEP, PVC mode did not show better performance either intraoperatively or postoperatively. Previous study showed that low VT along with low PEEP could increase the atelectasis (24) so we set the PEEP at the level of 5 cmH2O which seemed to be necessary for PV (23). Under these settings we did not find any increased incidence of atelectasis in group V compared with group P. Another recent meta-analysis (25) on comparison of pressure-controlled ventilation with volume-controlled ventilation during OLV got the conclusion that PCV had better performance on oxygenation and Ppeak. Our result showed a lower Ppeak in group P but not better oxygenation. Although previous study implied PCV was in association with better oxygenation during OLV (26), PCV per se did not show any effect on gas exchange (27,28). We set the same PEEP value in both groups and this maybe the main reason why there was no significant difference with oxygenation between two groups.
As to the patients with high risks of PPCs, elderly patients seemed to get more intraoperative benefits from both PCV and PCV-VG ventilation modes during OLV (10). But there was still no data for postoperative complications and prognosis. At the mean time their VT (8 mL/kg) was higher than we used (6 mL/kg) in this study.
The limitation of our study was that the patients enrolled were at low risk of PPCs and it was important to find out if the risk patients can benefit from suitable ventilation mode during OLV. Furthermore we did not test the inflammatory cytokines from the reactions of our body to different ventilation mode during OVL.
In conclusion, our present study showed that VCV and PCV had the same performance of PPCs under the condition of PV.
Acknowledgements
This work was supported by the research foundation from The 2nd Oriental Congress of Anesthesiology and Perioperative Medicine for the research on optimizing the intraoperative ventilation strategy in minimal invasive thoracic surgery.
Footnote
Conflicts of Interest: The authors have no conflicts of interests to declare.
Ethical Statement: The study was approved by institutional ethics committee of Zhongshan Hospital, Fudan University (No. B2012-064) and written informed consent was obtained from all patients.
References
- Licker M, Fauconnet P, Villiger Y, et al. Acute lung injury and outcomes after thoracic surgery. Curr Opin Anaesthesiol 2009;22:61-7. [Crossref] [PubMed]
- Cerfolio RJ, Pickens A, Bass C, et al. Fast-tracking pulmonary resections. J Thorac Cardiovasc Surg 2001;122:318-24. [Crossref] [PubMed]
- McKenna RJ Jr, Mahtabifard A, Pickens A, et al. Fast-tracking after video-assisted thoracoscopic surgery lobectomy, segmentectomy, and pneumonectomy. Ann Thorac Surg 2007;84:1663-7; discussion 1667-8.
- Yang M, Ahn HJ, Kim K, et al. Does a protective ventilation strategy reduce the risk of pulmonary complications after lung cancer surgery?: a randomized controlled trial. Chest 2011;139:530-7. [Crossref] [PubMed]
- Schultz MJ, Haitsma JJ, Slutsky AS, et al. What tidal volumes should be used in patients without acute lung injury? Anesthesiology 2007;106:1226-31. [Crossref] [PubMed]
- Blum JM, Stentz MJ, Dechert R, et al. Preoperative and intraoperative predictors of postoperative acute respiratory distress syndrome in a general surgical population. Anesthesiology 2013;118:19-29. [Crossref] [PubMed]
- Licker M, de Perrot M, Spiliopoulos A, et al. Risk factors for acute lung injury after thoracic surgery for lung cancer. Anesth Analg 2003;97:1558-65. [Crossref] [PubMed]
- Fernández-Pérez ER, Sprung J, Afessa B, et al. Intraoperative ventilator settings and acute lung injury after elective surgery: a nested case control study. Thorax 2009;64:121-7. [Crossref] [PubMed]
- Song SY, Jung JY, Cho MS, et al. Volume-controlled versus pressure-controlled ventilation-volume guaranteed mode during one-lung ventilation. Korean J Anesthesiol 2014;67:258-63. [Crossref] [PubMed]
- Lin F, Pan L, Qian W, et al. Comparison of three ventilatory modes during one-lung ventilation in elderly patients. Int J Clin Exp Med 2015;8:9955-60. [PubMed]
- Pu J, Liu Z, Yang L, et al. Applications of pressure control ventilation volume guaranteed during one-lung ventilation in thoracic surgery. Int J Clin Exp Med 2014;7:1094-8. [PubMed]
- Petrucci N, Iacovelli W. Lung protective ventilation strategy for the acute respiratory distress syndrome. Cochrane Database Syst Rev 2007;18:CD003844. [PubMed]
- Alam N, Park BJ, Wilton A, et al. Incidence and risk factors for lung injury after lung cancer resection. Ann Thorac Surg 2007;84:1085-91; discussion 1091. [Crossref] [PubMed]
- Nichols D, Haranath S. Pressure control ventilation. Crit Care Clin 2007;23:183-99. viii-ix. [Crossref] [PubMed]
- Della Rocca G, Coccia C. Acute lung injury in thoracic surgery. Curr Opin Anaesthesiol 2013;26:40-6. [Crossref] [PubMed]
- Keszler M. Volume-targeted ventilation. Early Hum Dev 2006;82:811-8. [Crossref] [PubMed]
- MacIntyre NR. New modes of mechanical ventilation. Clin Chest Med 1996;17:411-21. [Crossref] [PubMed]
- Al-Saady N, Bennett ED. Decelerating inspiratory flow waveform improves lung mechanics and gas exchange in patients on intermittent positive-pressure ventilation. Intensive Care Med 1985;11:68-75. [Crossref] [PubMed]
- Prella M, Feihl F, Domenighetti G. Effects of short-term pressure-controlled ventilation on gas exchange, airway pressures, and gas distribution in patients with acute lung injury/ARDS: comparison with volume-controlled ventilation. Chest 2002;122:1382-8. [Crossref] [PubMed]
- Neto AS, Hemmes SN, Barbas CS, et al. Association between driving pressure and development of postoperative pulmonary complications in patients undergoing mechanical ventilation for general anaesthesia: a meta-analysis of individual patient data. Lancet Respir Med 2016;4:272-80. [Crossref] [PubMed]
- Slinger P. Pro: low tidal volume is indicated during one-lung ventilation. Anesth Analg 2006;103:268-70. [Crossref] [PubMed]
- Boussarsar M, Thierry G, Jaber S, et al. Relationship between ventilatory settings and barotrauma in the acute respiratory distress syndrome. Intensive Care Med 2002;28:406-13. [Crossref] [PubMed]
- Liu Z, Liu X, Huang Y, et al. Intraoperative mechanical ventilation strategies in patients undergoing one-lung ventilation: a meta-analysis. Springerplus 2016;5:1251. [Crossref] [PubMed]
- Güldner A, Kiss T, Serpa Neto A, et al. Intraoperative protective mechanical ventilation for prevention of postoperative pulmonary complications: a comprehensive review of the role of tidal volume, positive end-expiratory pressure, and lung recruitment maneuvers. Anesthesiology 2015;123:692-713. [Crossref] [PubMed]
- Kim KN, Kim DW, Jeong MA, et al. Comparison of pressure-controlled ventilation with volume-controlled ventilation during one-lung ventilation: a systematic review and meta-analysis. BMC Anesthesiol 2016;16:72. [Crossref] [PubMed]
- Sentürk NM, Dilek A, Camci E, et al. Effects of positive end-expiratory pressure on ventilatory and oxygenation parameters during pressure-controlled one-lung ventilation. J Cardiothorac Vasc Anesth 2005;19:71-5. [Crossref] [PubMed]
- Esteban A, Alía I, Gordo F, et al. Prospective randomized trial comparing pressure-controlled ventilation and volume-controlled ventilation in ARDS. For the Spanish Lung Failure Collaborative Group. Chest 2000;117:1690-6. [Crossref] [PubMed]
- Kallet RH, Campbell AR, Dicker RA, et al. Work of breathing during lung-protective ventilation in patients with acute lung injury and acute respiratory distress syndrome: a comparison between volume and pressure-regulated breathing modes. Respir Care 2005;50:1623-31. [PubMed]


