Double pseudoaneurysm, recurrent subvalvular aortic membrane and small left ventricular outflow tract in the same patient: who dares?
Introduction
Left ventricular outflow tract (LVOT) pseudoaneurysm is an uncommon complication following aortic valve replacement (AVR). Its diagnosis is difficult since it does not present specific symptoms (1). However, they are an important source of life threatening complications such as fistula formation, rupture or thrombosis of the pseudoaneurysm and compression of adjacent structures (2,3).
Case presentation
A 37-year-old woman with severe growth retardation who underwent surgery at 7 years of age due to congenital aortic stenosis, performing valvulotomy of the aortic valve and resection of a subvalvular aortic membrane. Sixteen years later she required a new intervention by performing resection of a new subaortic ridge and AVR with implantation of a mechanical aortic prosthesis. After this surgery, the patient remained asymptomatic despite peak trans-prosthetic gradients of 44 mmHg.
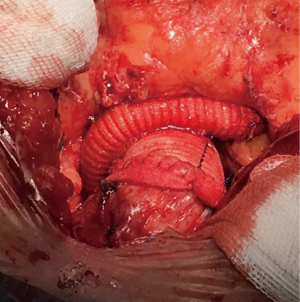
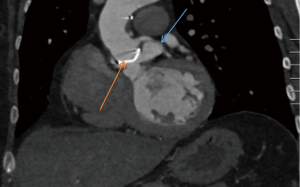
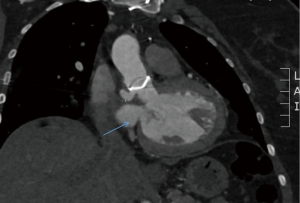
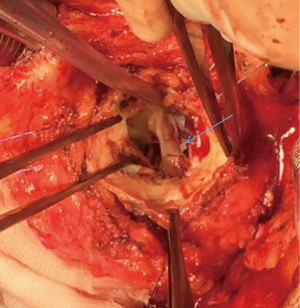
In the last 6 months, the patient suffered functional deterioration with NYHA grade II for dyspnea, so a new echocardiogram was performed. This showed the recurrence of the subaortic membrane with increased transvalvular gradients. Thoracic computed tomography (CT) scan was performed for a better visualization. CT demonstrated the presence of a subaortic membrane and two subvalvular pseudoaneurysms. One of them was related to the left coronary sinus and the other one to the noncoronary sinus. Diameters were 20.1 mm × 10.6 mm (Figures 1,2) and 10.3 mm × 8 mm respectively (Figures 3,4). In this same CT, a LVOT hypoplasia with a minimum diameter of 11 mm was observed. With this data, the patient underwent surgery for the extraction of the prosthesis to allow the resection of the subaortic membrane and both pseudoaneurysms (Figure 5). In addition, LVOT was enlarged and the aortic valve and aortic root were replaced by a mechanical prosthesis and a 26 mm Dacron graft. The rigidity of the tissues forced to perform coronary artery ostia reimplantation according to Cabrol’s technique using an 8-mm Dacron graft and a termino-terminal anastomosis (Figure 6). The extracorporeal circulation and aortic cross-clamp times were 236 and 195 minutes respectively, using intermittent anterograde and retrograde cold crystalloid cardioplegia.

The postoperative evolution was good and the patient was discharged on the seventh day. The only complication was a complete atrioventricular block requiring implantation of a definitive pacemaker. The control echocardiogram showed a mean transvalvular gradient of 9 mmHg and a LVOT diameter of 16 mm.
Discussion
Echocardiography has several limitations on this entity. In addition, vague symptoms commonly associated with this late complication make the diagnosis really difficult. However, high rate of life-threating situations related to this entity have been described, which make early intervention essential (4).
The most frequent place for pseudoaneurysm after AVR is the aortic cannulation location and the suture line of the aortotomy (3,5). Our patient had an infrequent site of both pseudoaneurysms, which were related to the aortic annulus, below the implanted prosthesis. This location has been associated with aortic wall weakness but also with problems in suture technique (4,6). In order to be able to resect both pseudoaneurysms it was necessary to remove the previously implanted prosthesis. In addition, LVOT enlargement and valvular replacement with a larger prosthesis were achieved. Given the dense adhesions, aortic root replacement was performed using the technique described by Cabrol. This technique involves the re-implantation of the coronary ostia using a small Dacron graft (7).
Conclusions
We publish here for the first time a clinical case of a 37-year-old woman with recurrent subvalvular aortic membrane, two subvalvular pseudoaneurysms and small LVOT. Surgical resection of the pseudoaneurysms, aortic root replacement using the Cabrol technique, enlargement of the LVOT and excision of the membrane was successfully performed.
Although less invasive techniques have emerged in recent years allowing the closure of postoperative pseudoaneurysms, surgery remains the technique of choice in these patients, allowing complete resection with moderate postoperative risk (8-10). Despite the problems described with the Cabrol technique, it is a good solution in this type of patients in whom the direct re-implantation of the coronary arteries is hampered by the stiffness of the tissues (11,12).
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
References
- Shariff MA, Martingano D, Khan U, et al. Left Ventricular Out ow Tract Pseudoaneurysm after Aortic Valve Replacement. AORTA (Stamford) 2015;3:167-71. [Crossref] [PubMed]
- Mohammadi S, Bonnet N, Leprince P, et al. Reoperation for false aneurysm of the ascending aorta after its prosthetic replacement: surgical strategy. Ann Thorac Surg 2005;79:147-52; discussion 152. [Crossref] [PubMed]
- Malvindi PG, van Putte BP, Heijmen RH, et al. Reoperations for aortic false aneurysms after cardiac surgery. Ann Thorac Surg 2010;90:1437-43. [Crossref] [PubMed]
- Tsai IC, Hsieh SR, Chern MS, et al. Pseudoaneurysm in the left ventricular outflow tract after prosthetic aortic valve implantation: evaluation upon multidetector-row computed tomography. Tex Heart Inst J 2009;36:428-32. [PubMed]
- Sullivan KL, Steiner RM, Smullens SN, et al. Pseudoaneurysm of the ascending aorta following cardiac surgery. Chest 1988;93:138-43. [Crossref] [PubMed]
- Yeo TC, Malouf JF, Oh JK, et al. Clinical profile and outcome in 52 patients with cardiac pseudoaneurysm. Ann Intern Med 1998;128:299-305. [Crossref] [PubMed]
- Cabrol C, Pavie A, Gandjbakhch I, et al. Complete replacement of the ascending aorta with reimplantation of the coronary arteries: new surgical approach. J Thorac Cardiovasc Surg 1981;81:309-15. [PubMed]
- Romaguera R, Slack MC, Waksman R, et al. IMAGE CARDIO MED: Percutaneous closure of a left ventricular outflow tract pseudoaneurysm causing extrinsic left coronary artery compression by transseptal approach. Circulation 2010;121:e20-2. [Crossref] [PubMed]
- Jiménez Valero S, García E, González Pinto A, et al. Percutaneous closure of pseudoaneurysm of the mitral-aortic intervalvular fibrosa. Rev Esp Cardiol 2005;58:1473-5. [PubMed]
- Katada Y, Ito J, Shibayama K, et al. Transapical Transcatheter Closure of the Pseudoaneurysm in the Left Ventricular Outflow Tract After Aortic Valve Replacement. JACC Cardiovasc Interv 2016;9:e181-3. [Crossref] [PubMed]
- Tanaka A, Afaq S, Atay S, et al. Redo aortic root replacement reutilizing 22-year patent modified Cabrol grafts. Eur J Cardiothorac Surg 2017;51:794-6. [PubMed]
- Knight J, Baumüller S, Kurtcuoglu V, et al. Long-term follow-up, computed tomography, and computational fluid dynamics of the Cabrol procedure. J Thorac Cardiovasc Surg 2010;139:1602-8. [Crossref] [PubMed]