Influenza seasonality and predominant subtypes of influenza virus in Guangdong, China, 2004-2012
Introduction
Influenza is a widespread viral infectious disease causing seasonal epidemics and periodic pandemics in the worldwide (1-3). A better understanding of seasonal patterns of influenza is essential for the development of effective prevention and control strategies for influenza (4). The seasonality of human influenza in temperate regions has been well documented (5-10). In these areas both in northern and southern hemisphere, annual seasonal epidemics of influenza occur consistently during winter or early spring months (11). On the other side, temporal pattern of influenza activity varies more considerably in subtropical and tropical locales (12). In opposition to temperate regions, influenza in some tropical countries circulates year round with peaks in rainy season (13-15), whereas some others have two distinct influenza seasons in winter/spring and summer months within a year, such as Singapore and Hong Kong (16-18).
Influenza surveillance data collected in the Chinese mainland have shown two seasonal cycles of influenza (19). Influenza in northern China has a regular winter peak, which is also shown in the other countries and regions with temperate climates. Some provinces in southern China are proven to have both winter/spring and summer peaks of seasonal influenza epidemics (20). However, the influenza activity in Guangdong province tends to have neither winter peak nor bimodal mode within a year.
Guangdong province located in southern China is a subtropical region in Southeast Asia with a population over 100 million. Seasonal influenza is a critical public health issue in the province. As Influenza viruses undergo frequent antigenic changes, diverse subtypes of influenza virus circulate in the province. The incidence of influenza was estimated to be 4 to 20 per 1,000 populations in the province (21). The H1N1 influenza pandemic also attacked the province heavily in 2009 and brought nearly 10,000 laboratory-confirmed cases of H1N1 and 36 deaths (22). The Guangdong provincial Centre for Disease Control and Prevention (Guangdong CDC), a WHO Collaborating Center for Surveillance of Emerging Infectious Diseases, has been conducting systematic surveillance on surveillance for years. Guangdong CDC also publishes updated reports regarding seasonal influenza activity termly multiple times each year. Based on systematic surveillance, continuous monitoring data and evidences from clinics and laboratories indicate that Guangdong also has a potential seasonal pattern of influenza activity.
In China, annual vaccination campaigns are timed according to the Northern Hemisphere winter season (23). As the seasonality in one region may not be the case in other ones, a different and complex seasonality will complicate local annual vaccination campaign and other prevention measures. Few studies report the seasonality of influenza and its virological variants at a provincial level in Guangdong. It is necessary to study the seasonal characteristics of influenza activity in Guangdong. This paper summarizes epidemiological and virological features of influenza from 2004 through 2012 to give a comprehensive insight into the influenza activity in Guangdong province. Our study findings can help to improve evidence-based prevention and control strategies for influenza in the future.
Materials and methods
The Guangdong Influenza Surveillance Network
Our study uses surveillance data from the Guangdong Influenza Surveillance System, which is a national system conducted by Center for Disease Control and Prevention of Guangdong Province (Guangdong CDC), to measure the influenza activity in Guangdong province. Between 2004 and 2009, the Guangdong Influenza Surveillance Network comprised of 14 sentinel hospitals and 9 collaborating laboratories across 13 prefectures in Guangdong. Before 2006, the sentinel units in the network made records through the traditional “pen and paper” methods. Since 2006, the sentinels have reported surveillance data by the National Influenza Surveillance Information System. It is a web-based reporting system, which has reduced serious missing data problems and brought a great improvement in reporting timeliness and data management.
Because of H1N1 influenza pandemic in 2009, the influenza surveillance network in Guangdong had been expanded to cover all 21 prefectures. In this upgraded network, the number of sentinel hospitals and influenza laboratories was increased to 28 and 22 respectively. The type of sentinel hospitals mainly includes central hospital, comprehensive hospital and maternal and child hospital based on city-level and county-level. The Guangdong CDC and local CDC in 21 prefectures run these 22 influenza virologic laboratories. There are three categories of influenza surveillance in Guangdong: Influenza-like Illness (ILI) Outpatient Surveillance, ILI Outbreak Surveillance and Influenza Virus Surveillance.
ILI Outpatient Surveillance
According to World Health Organization criteria, ILI is defined as a fever (Body temperature ≥38 °C) with a cough and /or a sore throat, and the absence of other diagnoses. In all of 28 sentinel hospitals (before 2010,the number is 14), physicians from department of pediatrics, department of respiratory and emergency room record the number of outpatients they treated each day, as well as the number of outpatients who present with non-specific symptoms that meet a case definition of ILI. Both of these two types of records are uploaded to the National Influenza Surveillance Information System and the weekly percentages of ILI outpatients can be calculated automatically.
Influenza Virus Surveillance
For monitoring influenza virus activity, sentinel hospitals through the province were required to collect 5-15 nasopharyngeal or throat swabs each week from ILI outpatients who had not taken antiviral drugs and who had a fever (Body temperature ≥38 °C) for no longer than 3 days. Informed consent was obtained from all subjects (or children’s guardians) recruited to receive a laboratory test.
The swabs were sent to the laboratories participating in viral surveillance, which are located in province or city-level CDC, for influenza virus test and identification of virus subtypes. A total of 22 laboratories report the total number of specimens received for influenza virus testing and the number testing positive for influenza A (H1N1), A (H3N2), A (H1N1) pdm09, A (not subtyped), or influenza B each week, via the National Influenza Surveillance Information System. All isolates of influenza virus collected by laboratories in city-level CDC are required to send to provincial CDC for confirmation testing.
ILI Outbreak Surveillance
ILI Outbreak Surveillance is passive in Guangdong. If Outbreaks (15 ILI cases affected or above within 7 days in a small unit, like community, school, nursing house, etc.) occur and are detected, local CDCs are required to report to Guangdong CDC through the National Influenza Surveillance Information System in 24 hours. Field investigation is launch and at least 10 respiratory samples of affected ILI cases are required to be collected and test for influenza virus in each ILI outbreak. All epidemiological and virological information referring ILI outbreaks are uploaded to the National Influenza Surveillance Information System.
Data management and analysis
Data collection
All data used in this paper are from the National Influenza Surveillance Information System and provided by Guangdong CDC. Our study period is from January 2004 to December 2012. The units of analysis used were weekly percentage of clinic outpatients with ILI, monthly counts of influenza virus and monthly number of influenza outbreaks as well as their laboratory results. The surveillance week starts on Monday and ends on Sunday. There are 469 weekly data in total, from the 1st week in 2004 (2001-01-05 to 2001-01-11) to the 52nd week in 2012 (2012-12-24 to 2012-12-30).
Of note, ILI surveillance system in Guangdong had added its sentinel hospitals from 14 to 28 since 2010. Thus only original 14 hospitals have complete data between 2004 and 2012. For comparability and consistency, we select and aggregate ILI surveillance data of the 14 sentinel hospitals, throughout the study period, to measure the long-term trends and periodical patterns of ILI epidemic at a provincial level. The ILI data analyzed in this paper are provincial time series of weekly percentages of ILI cases, which is produced by dividing the totals number of weekly ILI case numbers by the total number of all outpatients in all 14 selected hospitals. For influenza virus surveillance, only 9 collaborating laboratories reported virological data each month between 2004 and 2008. Since 2009, extra 13 laboratories had engaged in the surveillance.
Time series analysis
We used median, minimum and maximum (peak) value with their appearing time to describe the annual level of ILI epidemic. To explore the periodicity of the provincial time series of ILI data, we applied spectral analysis and built a logistic regression model to fit and set a warning line for the time series of the weekly ILI visiting percentage in Guangdong. With a Fast Fourier transformation (FFT) (24) in our spectral analysis, the periodic components of the time series of weekly ILI percentage can be extracted. These periodic components then would be invited into the logistic regression model as potential explained variables. The model is
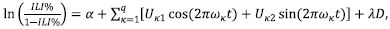
where ILI% denotes the weekly provincial ILI visiting percentage; α represents the intercept; Uk for κ=1,2,…,q, are the parameters to be estimated; ωk are the periodic parameters calculated by FFT; t denotes the corresponding number of the 469 surveillance weeks in chronological order; D is a categorical variable indicating influenza epidemic status (0= pre-pandemic, 1= in pandemic and 2= post-pandemic), and λ is vector of coefficients. We take the fitted values as a baseline of weekly ILI percentage, and set their upper endpoints of 95% confident interval in the model as the thresholds for ILI surveillance.
Peak analysis
The seasonal parameters of influenza virus circulating were estimates of peak month and epidemic duration by “Peak analysis”. Peak month was identified as the month with the maximum number of strains isolated within a calendar year. Epidemic duration was defined as the numbers of months in epidemic periods, which is defined as periods of two or more consecutive months in which each month accounted for more than 5% of the annual total number of specimens that tested positive for influenza. We also identified semi-annual patterns if two peaks occurred at least 3 months apart within the same calendar year, and monthly proportions of virus isolates between them are all less than 5%. All analyses and plots were conducted using R, an open-source programming language for statistical analysis (25).
Ethics statement
The protocol of this study was reviewed completely and approved by the ethics committee of the Guangdong CDC. Data records and collection in the process of surveillance did not reveal the patient’s personal information and privacy. There was no required written consent from patients as the study was based on aggregated and de-identified data. No information about the identity of any patients was retained.
Results
ILI epidemics
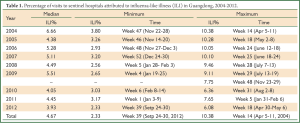
During the 9-year study period, a total of 37,571,582 outpatients had been recorded, of which 1,889,684 ILI cases had been reported from sentinel hospitals. The provincial average level of patient visiting to sentinel hospitals for ILI varied remarkably every year. From 2004 to 2008, patient visits for ILI peaked at 9-10%. Since the H1N1 influenza pandemic arrived in 2009, Guangdong had two separate ILI peaks this year. One was detected in July causing by seasonal influenza, with a peak value of 9%. The other affected by the pandemic shown in November 2009, with a peak value of 7%. After the pandemic, the ILI visiting level declined between 2010 and 2012, with peaks at 6-8%. The annual median, minimum and maximum value of ILI visiting percentage were shown in Table 1.
Full Table
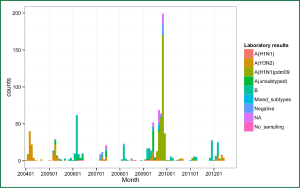
From Figure 1, the weekly ILI epidemic in Guangdong displayed strong annual periodicity. The FFT clearly identified one periodic component (1/ω =1/0.01875≈53 weeks). A unimodal model was applied and the estimated parameters were given in Table 2. The ILI visiting level had a strong annual unimodal cycle between 2004 and 2008, when the ILI activity was above the thresholds regularly from spring to summer in Guangdong. It was bimodal in 2009 because of the influenza A (H1N1) pandemic. The ILI surveillance data peaked sharply and unusually in November 2009, far beyond the thresholds. After the pandemic, the trends of weekly ILI visiting percentage came back to the unimodal periodic mode. But their peaks became weaker in the following three years from 2010 to 2012. The ILI visiting percentage delayed its peak in 2010 and spiked early in 2011. The estimated model also told that the annual average level of ILI visiting percentage has barely changes (the coefficient of D =1 is 1.05, P=0.19) in pandemic period comparing with that in pre-pandemic periods, however the ILI percentage decreased statistical significantly (the coefficient of D =2 is 0.8, P<0.001) after 2009.
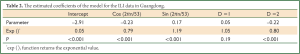
Full Table
Predominant subtypes of influenza virus
There have been several subtypes of seasonal influenza virus and an influenza pandemic virus isolated in Guangdong, including influenza A (H1N1), A (H3N2), A (H1N1) pdm09 (a novel subtype identified in influenza pandemic 2009) and influenza B. A total of 107115 respiratory specimens of ILI outpatients were collected from 2004 through 2012, 16.29% of them tested for influenza virus were positive. Of the 17454 influenza isolates reported to Guangdong CDC, 4,899 (28.07%) were influenza A (H3N2), 1,305 (7.48%) were influenza A (H1N1), 5,284 (30.27%) were influenza A (H1N1) pdm09, 988 (5.66%) were A (not subtyped) and 4,978 (28.52%) were influenza B.
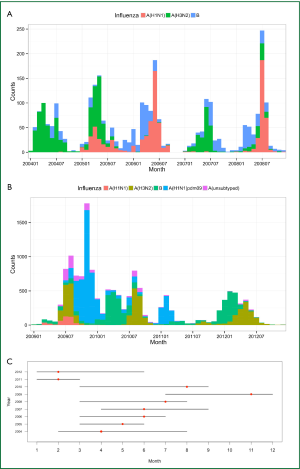
According to the bar charts showing influenza subtypes (Figure 2A,B), the proportion of influenza virus subtypes changed frequently between 2004 and 2012. Influenza A (H3N2) Predominated in 2004 and 2007, but influenza B also was identified. Influenza A (H1N1) grew in 2005 and became a major subtype both in 2006 and 2008. Influenza A (H1N1) pdm09 was identified firstly in Guangdong in May 2009 and started to predominated from July 2009 to January 2010. After the pandemic, Influenza A (H1N1) pdm09 circulated weakly in 2010 and became active again in 2011. There are two major types of influenza virus both in 2010 and 2012, when influenza B was isolated more frequently in spring and then Influenza A (H3N2) followed as a main subtype in the summer.
Influenza virus peak time and epidemic duration are presented in Figure 2C. Influenza virus peaks in 6 of 9 years came in summer months in Guangdong, from April to September. In 2011 and 2012, the peaks appeared in February. The longest epidemic duration for influenza virus isolated was 7 months (in 2004 and 2010) while the shortest one was 3 months (in 2011). Median epidemic duration was 6 months.
Outbreak reports
A total of 925 ILI outbreaks recorded in Guangdong from 2004 to 2012, in which 45,322 cases were affected. The majority of reported outbreaks (832 outbreaks, 90%) occurred in institutional settings, such as schools, colleges and kindergartens. ILI outbreaks in the province occurred mostly in spring and summer, from March to July each year of seasonal influenza epidemic. The global pandemic in 2009 brought an extra and extremely high peak of ILI outbreak reporting in fall.
Of 925 outbreaks in Guangdong, 919 (99%) had done laboratory test for influenza virus, yet 6 had not sampled. Of 919 outbreaks with laboratory test, 828 (90%) outbreaks associated with influenza had been confirmed, 48 (5%) were negative for influenza virus test, and 43 (5%) had no available information. H3N2 caused all influenza outbreaks in 2004. H3N2 and type B were two main influenza viruses causing multiple seasonal influenza outbreaks in 2005, 2007, 2010 and 2012. There was no H3N2 outbreak detected in 2006, 2008 and 2011, when type B was isolated mostly. H1N1 pdm2009 was responsible for most outbreaks in 2009 (Figure 3).
Discussion
Due to development and efforts during the last decade, Guangdong’s influenza surveillance system, monitoring ILI, influenza virus and influenza outbreak, has covered all prefectures throughout the province. Complete and reliable surveillance data for influenza can be used to estimate the activity of influenza in Guangdong. To our knowledge, this is the first study to systematically review influenza activity in Guangdong, by combining epidemiological data and laboratory results on a provincial scale.
ILI surveillance is essentially a type of syndromic surveillance (26). ILI is usually caused by influenza virus and other respiratory viruses. The ILI temporal trends normally reflect the actual influenza activity in epidemic seasons (8,9). With an exception in pandemic periods [August 2009 to June 2010 in Guangdong (22,27)], the time series of ILI visiting percentage in Guangdong showed a clear and strong seasonal pattern with a peak occurring mostly in summer each year. According to our results, ILI percentage often went down to a minimum value among cold months. It is suggested that fewer cases see doctor for ILI in winter in Guangdong. Although the seasonality continued after the 2009 H1N1 pandemic, some parameters have been changing. The provincial ILI visiting percentages declined and ran at an observable lower level, as well as the ILI peak timing became more diverse from 2010 to 2012. Further researches should determine what factors are reducing the ILI percentages in Guangdong province.
It is worth to note that ILI surveillance is sensitive and affected easily by some known and unknown factors, like other syndromic surveillances do (26). A sudden increase of ILI outside regular epidemic months may bring a signal of a novel virus coming. The ILI percentage spiked rapidly in November 2009 and in January 2011. These two peaks taking place outside regular seasons were attributed to influenza A (H1N1) pdm09, a novel influenza virus causing a global pandemic in 2009 (28). It is also observed that some minor and instant increases of ILI visiting percentage appear at early time each year, which are absent in time series of virological data. A likely reason is holiday effects. Chinese New Year, called Spring Festival, comes with 7-day public holiday usually in January or February each year, when outpatients visiting activity may be biased.
In generally, different subtypes of influenza virus can co-circulate throughout the year in Guangdong. The same virus subtype never predominated during more than two consecutive calendar years from 2004 through 2012. The displacement of one subtype with another was gradual overall. Current studies revealed that in tropical zones of the Northern and Southern Hemispheres, peak timing of influenza virus activity is more variable with several modes (12,29). In East and South East Asia, including Philippines, Singapore, Thailand, Vietnam and Hong Kong, semi-annual influenza activity was identified (30-33). In these locales, the major peak of influenza virus insolated was reported in winter, and the minor one occurred in summer. In contrast, the dynamic patterns of influenza virus activity in Guangdong had some differences and seemed to be experiencing some changes. Basing on the definition of influenza virus peak and epidemic duration in our analysis, there were no two separated peaks occurring within a year. Most annual peaks of influenza virus isolated came along with their epidemic durations between April and September, in which Guangdong’s summer is. No peak had occurred in January or December.
Vaccination is the most effective way to prevent infection and severe outcomes caused by influenza viruses. The World Health Organization (WHO) convenes technical consultations in February and September each year to recommend viruses for inclusion in influenza vaccines for the northern and southern hemispheres, respectively (34). China and many other countries in northern hemisphere with winter epidemics launch annual influenza vaccination campaign before the start of every winter season. Guangdong follows the national recommendation and initials its provincial influenza vaccination in fall. Our findings shown that the epidemic season is usually in summer. Such difference from typical winter epidemics may produce local difficulties in maintaining an efficient vaccination program.
Nevertheless, we cannot rule out some underlying semi-annual peaks of influenza activity during the 9-year study periods. Taking virus isolates in 2006 and 2008 as examples, a minor peak caused by influenza B and a major one attributed to seasonal influenza A (H1N1) could be recognized. Yet these two types of virus co-circulated actively during same epidemic durations, and their peaks overlapped each other. Because of expanded surveillance program and more collaborating laboratories taking part in, the number of influenza virus isolates increased largely. The influenza virus activity in 2010 and 2012 tended to present a bimodal seasonality more clearly, with two distinct peaks in spring and summer respectively.
Seasonal influenza outbreaks in Guangdong normally concentrated in spring and summer, which coincide partly with ILI and influenza virus activity peaks. Although widespread influenza activity typically occurs during the epidemic seasons in Guangdong, sporadic cases and outbreaks can basically occur at any time of the year. Our findings of virological surveillance show that influenza viruses were identified each month during the study periods. There was, however, no outbreak reported in some months in Guangdong. It may be explained partly by the passive surveillance system. Schools and other institutional settings are encouraged to report any likely influenza outbreaks, but it is hard to monitor in summer (in July and August) or winter holidays (in January and February). Excess outbreaks occurred in the pandemic of 2009. Due to limitation of public health resources, some of them had not been sampled or tested for influenza virus.
The exact mechanism of influenza activity remains poorly understood. Seasonal changes in virus survival and transmissibility, host susceptibility to infection and social behavior, and their interactions have been suggested to play a key role (12,35,36). Meteorological factors also can affect influenza activity directly. Some researches pointed that cold temperatures, low indoor humidity and minimal solar radiation are causally associated with a higher activity of influenza in temperate regions (37-39). On the other hand, mounting evidence revealed a link between increased influenza activity and high humidity as well as the rainy season in several tropical populations (40-42). Guangdong has the typical subtropical marine monsoon climate. Winters in Guangdong are not so cold with plentiful sunshine, while summers are long and hot. Springs and autumns are cool and humid in Guangdong. Guangdong’s rainy seasons are range from April to September. Studies in future are necessarily to explore what determinants and how they work in influenza activity of Guangdong.
This study used aggregate data to measure influenza activity and explore seasonal periodicity on a provincial scale. The overall dynamic pattern may not fit those in different parts of the province. We did not collect data by age groups, in which the features of influenza activity may be diverse. Our findings hinted that some parameters of seasonal pattern are different between pre- and post the pandemic periods. It remains to be shown whether inter-pandemic influenza follows the same pattern.
In conclusion, influenza circulates periodically every year in Guangdong. Influenza activity in Guangdong had relatively strong and clear seasonality with epidemic periods in summer for last decade. The pattern of influenza activity is developing. Annual major peaks used to be in summer, but after the pandemic they brought forward in spring apparently in recent years. The presence of local unique seasonal pattern and its changes emphasizes the need to optimize timing of influenza vaccine delivery and other public health interventions.
Acknowledgements
We thank all the staff throughout the influenza surveillance network in Guangdong for their assistance with data collection, sample acquisition and field investigation. We are also grateful to Patricia Bowles of Griffith University (Australia) for critical reading of the manuscript.
Disclosure: The authors declare no conflict of interest.
References
- Western Pacific Region Global Influenza Surveillance and Response System. Epidemiological and virological characteristics of influenza in the Western Pacific Region of the World Health Organization, 2006-2010. PLoS One 2012;7:e37568. [PubMed]
- World Health Orgnization. Influenza fact sheet. Available online: http://www.who.int/mediacentre/factsheets/2003/fs211/en/, revised March 2003.
- Simonsen L. The global impact of influenza on morbidity and mortality. Vaccine 1999;17 Suppl 1:S3-10. [PubMed]
- World Health Organization (2007). Acute respiratory infections: Influenza. Available online: http://www.who.int/vaccine_research/diseases/ari/en/index.html, accessed 15 March 2011.
- Meijer A, Paget WJ, Meerhoff TJ, et al. Epidemiological and virological assessment of influenza activity in Europe, during the 2004-2005 winter. Euro Surveill 2006;11:111-8. [PubMed]
- Paget WJ, Meerhoff TJ, Meijer A, et al. Epidemiological and virological assessment of influenza activity in Europe during the 2003-2004 season. Euro Surveill 2005;10:107-11. [PubMed]
- Brammer TL, Murray EL, Fukuda K, et al. Surveillance for influenza--United States, 1997-98, 1998-99, and 1999-00 seasons. MMWR Surveill Summ 2002;51:1-10. [PubMed]
- Arkema JM, Meijer A, Meerhoff TJ, et al. Epidemiological and virological assessment of influenza activity in Europe, during the 2006-2007 winter. Euro Surveill 21;13. pii: 18958. [PubMed]
- Meijer A, Meerhoff TJ, Meuwissen LE, et al. Epidemiological and virological assessment of influenza activity in Europe during the winter 2005-2006. Euro Surveill 2007;12:E11-2. [PubMed]
- Lipsitch M, Viboud C. Influenza seasonality: lifting the fog. Proc Natl Acad Sci U S A 2009;106:3645-6. [PubMed]
- Finkelman BS, Viboud C, Koelle K, et al. Global patterns in seasonal activity of influenza A/H3N2, A/H1N1, and B from 1997 to 2005: viral coexistence and latitudinal gradients. PLoS One 2007;2:e1296. [PubMed]
- Tamerius J, Nelson MI, Zhou SZ, et al. Global influenza seasonality: reconciling patterns across temperate and tropical regions. Environ Health Perspect 2011;119:439-45. [PubMed]
- Alonso WJ, Viboud C, Simonsen L, et al. Seasonality of influenza in Brazil: a traveling wave from the Amazon to the subtropics. Am J Epidemiol 2007;165:1434-42. [PubMed]
- Dapat C, Saito R, Kyaw Y, et al. Epidemiology of human influenza A and B viruses in Myanmar from 2005 to 2007. Intervirology 2009;52:310-20. [PubMed]
- Russell CA, Jones TC, Barr IG, et al. The global circulation of seasonal influenza A (H3N2) viruses. Science 2008;320:340-6. [PubMed]
- Lee VJ, Yap J, Ong JB, et al. Influenza excess mortality from 1950-2000 in tropical Singapore. PLoS One 2009;4:e8096. [PubMed]
- Yang L, Wong CM, Lau EH, et al. Synchrony of clinical and laboratory surveillance for influenza in Hong Kong. PLoS One 2008;3:e1399. [PubMed]
- Viboud C, Alonso WJ, Simonsen L. Influenza in tropical regions. PLoS Med 2006;3:e89. [PubMed]
- Zou J, Yang H, Cui H, et al. Geographic divisions and modeling of virological data on seasonal influenza in the Chinese mainland during the 2006-2009 monitoring years. PLoS One 2013;8:e58434. [PubMed]
- Shu YL, Fang LQ, de Vlas SJ, et al. Dual seasonal patterns for influenza, China. Emerg Infect Dis 2010;16:725-6. [PubMed]
- Guo RN, Zheng HZ, Huang LQ, et al. Epidemiologic and economic burden of influenza in the outpatient setting: a prospective study in a subtropical area of China. PLoS One 2012;7:e41403. [PubMed]
- Yang F, He J, Zhong H, et al. Temporal trends of influenza A (H1N1) virus seroprevalence following 2009 pandemic wave in Guangdong, China: three cross-sectional serology surveys. PLoS One 2012;7:e38768. [PubMed]
- Recommended composition of influenza virus vaccines for use in the 2012-2013 northern hemisphere influenza season. Wkly Epidemiol Rec 2012;87:83-95. [PubMed]
- Brockwell PJ, Davis RA. Time series: theory and methods. Springer-Verlag New York, Inc. New York, NY, USA ©1986.
- R Development Core Team. R: a language and environment for statistical computing, reference index version 2.11.1. R Foundation for Statistical Computing, Vienna, Austria, 2008.
- Henning KJ. What is syndromic surveillance? MMWR Morb Mortal Wkly Rep 24;53 Suppl:5-11. [PubMed]
- Zhang X, He J, Li L, et al. Serologic survey of the pandemic H1N1 2009 virus in Guangdong Province, China: a cross sectional study. PLoS One 2011;6:e23034. [PubMed]
- Novel Swine-Origin Influenza A. Emergence of a novel swine-origin influenza A (H1N1) virus in humans. N Engl J Med 2009;360:2605-15. [PubMed]
- Park AW, Glass K. Dynamic patterns of avian and human influenza in east and southeast Asia. Lancet Infect Dis 2007;7:543-8. [PubMed]
- Hampson AW. Epidemiological data on influenza in Asian countries. Vaccine 1999;17 Suppl 1:S19-23. [PubMed]
- Simmerman JM, Chittaganpitch M, Levy J, et al. Incidence, seasonality and mortality associated with influenza pneumonia in Thailand: 2005-2008. PLoS One 2009;4:e7776. [PubMed]
- Nguyen HT, Dharan NJ, Le MT, et al. National influenza surveillance in Vietnam, 2006-2007. Vaccine 2009;28:398-402. [PubMed]
- Chan PK, Mok HY, Lee TC, et al. Seasonal influenza activity in Hong Kong and its association with meteorological variations. J Med Virol 2009;81:1797-806. [PubMed]
- World Health Orgnization (2013). Recommended composition of influenza virus vaccines for use in the 2013-2014 northern hemisphere influenza season. Availlable online: http://www.who.int/influenza/vaccines/virus/recommendations/201302_recommendation.pdf, accessed 20 February 2013.
- Dowell SF. Seasonal variation in host susceptibility and cycles of certain infectious diseases. Emerg Infect Dis 2001;7:369-74. [PubMed]
- Dowell SF, Ho MS. Seasonality of infectious diseases and severe acute respiratory syndrome-what we don't know can hurt us. Lancet Infect Dis 2004;4:704-8. [PubMed]
- Davey ML, Reid D. Relationship of air temperature to outbreaks of influenza. Br J Prev Soc Med 1972;26:28-32. [PubMed]
- Hemmes JH, Winkler KC, Kool SM. Virus survival as a seasonal factor in influenza and polimyelitis. Nature 1960;188:430-1. [PubMed]
- Hope-Simpson RE. The role of season in the epidemiology of influenza. J Hyg (Lond) 1981;86:35-47. [PubMed]
- Chew FT, Doraisingham S, Ling AE, et al. Seasonal trends of viral respiratory tract infections in the tropics. Epidemiol Infect 1998;121:121-8. [PubMed]
- de Mello WA, de Paiva TM, Ishida MA, et al. The dilemma of influenza vaccine recommendations when applied to the tropics: the Brazilian case examined under alternative scenarios. PLoS One 2009;4:e5095. [PubMed]
- Moura FE, Perdigão AC, Siqueira MM. Seasonality of influenza in the tropics: a distinct pattern in northeastern Brazil. Am J Trop Med Hyg 2009;81:180-3. [PubMed]