Primary pleural lymphoma: a rare case and a synopsis of the literature
Introduction
A rare case of non-pyothorax associated, small B-cell non-Hodgkin’s pleural lymphoma is reported in this article. The diagnosis of pleural malignant lymphoma seems to be difficult in most cases. If possible, surgical biopsy via thoracoscopy is recommended for early diagnosis. The more modern and minimally invasive approach of video-asssisted throacoscopic surgery (VATS) allows for a quicker patient recovery and discharge.
Case presentation
A 74 year-old-woman presented to the hospital with right sided chest pain and gradually increasing dyspnea. She had no past medical history of HIV infection, tuberculosis, pyothorax or autoimmune disease, and had not been previously exposed to asbestos. She had a prior history of anaemia diagnosed in Hematology department more than 1 year ago. Due to the dizziness and fatigue caused by the anaemia, she was admitted four times to the Hematology department during the year. Except for hemoglobin decreased, other routine laboratory studies, including bone puncture, were normal. There was a little right-sided pleural effusion diagnosed by chest X-ray at that time, but she didn’t accept pleurocentesis. Without definite diagnosis, she became depression and struggled with chronic right chest wall pain and gradually increasing dyspnea. So she followed the suggestion from her previous physician to do pleura biopsy and the pleural effusion drainage in our department. On physical exam, the right lower posterior chest was dull to percussion with diminished respiration, and moist rales were audible in the inferior lobe at the end of inspiration on auscultation. There was no palpable lymphadenopathy on exam, nor was there hepato-or splenomegaly. According to the abdominal ultrasound, there were no liver and spleen enlargement.
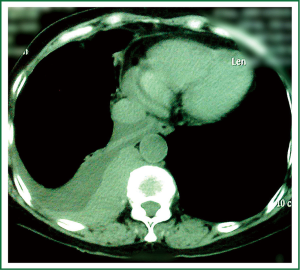
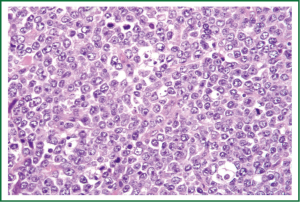
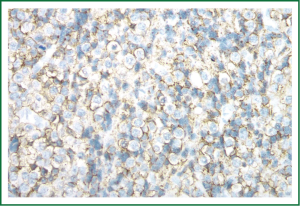
The patient’s CT demonstrated pleural effusion and irregular pleural mass in the right pleural cavity (Figure 1). The patient was scheduled for VATS to biopsy the pleural mass and drain the effusion. During the operation, disseminated white nodules were seen in a 4 cm × 4 cm area of the parietal pleura which the neoplasm involved, along with serous membrane hyperemia. Approximately 500 mL of yellow serous fluid was drained. A biopsy was taken from the nodules for pathological frozen section examination during the procedure. Though the pathological diagnosis was thought to be malignancy at the time, the diagnosis was not confirmed until a conventional pathologic exam was performed during the postoperative period. As it was malignancy pleural neoplasm with effusion, we gave up complete excision. At last, we performed mechanical pleurodesis to reduce pleural effusion. Pathological and immuno-histochemical examinations of the pleural nodule revealed that it was small B-cell lymphocytic lymphoma (SLL) (Figure 2). The neoplastic cells expressed the CD-20 antigen (Figure 3).
The pleural effusions ceased completely following surgery. The time from the first diagnosis of pleural disease until the thoracoscopic surgical intervention was one week. In the absence of any evidence of lymphoma outside the pleural space, the diagnosis of primary pleural lymphoma was made. The patient refused radiotherapy was discharged from the hospital without any other treatment, but with a plan for regular follow-up every 6 months. Our patient is still in complete remission after 12 months of follow-up.
Discussion
The patient presented with pronounced dyspnea, which was caused by a right-sided pleural effusion diagnosed as pleural lymphoma. King et al. reported that malignant lymphoma is very rare, comprising only 2.4% of primary chest wall tumors (1). Additionally, only two forms of high-grade lymphoma involve the pleura as primary neoplasms: primary effusion lymphoma (PEL) and pyothorax associated lymphoma (PAL) (2). Both have well characterized clinical and pathological features. Most cases of pleural lymphoma have been reported from Japan, and they were typically associated with persistent chronic tuberculous pyothorax or artificial pneumothorax for lung tuberculosis (3). Although any type of lymphoma can involve the pleura, diffuse large B-cell lymphoma has been reported as most frequent, followed by follicular lymphoma, with rates of approximately 60% and 20%, respectively (4). A small series of case reports have identified other types of pleural lymphoma, such as extra-nodal marginal zone B-cell lymphoma of mucosa-associated lymphoid tissue (EMZL/MALT-type) and mantle cell lymphoma (5,6). Therefore, primary pleural non-Hodgkin’s lymphoma (NHL) in an immunocompetent patient without a history of chronic pyothorax is extremely rare (7). Our case shows typical histological and immunohistological findings of SLL. The World Health Orgnization (WHO) classification recognizes it as an entity of non-Hodgkin lymphoma similar to chronic lymphocytic leukemia (CLL) (8). It is a low-grade NHL and pathologically shows that it is indolent. The large B-cell lymphoma needs to do systemic chemotherapy. But the SLL can be observed if there were no symptoms (8).
The mechanism of this rare type of lymphoma is likely a stimulation of B-lymphocytic cells in the pleural cavity, which is seen in long-standing chronic pleural disease (3). Rouviere and Miller, in 1938 and 1947, respectively, determined that normal subpleural regions are rich in lymphatic tissue (4). The chronic stimulation of B lymphocytes and the decrease in the number of circulating T lymphocytes may lead to lymphoid cell hyperplasia (7). Other postulated mechanisms for primary pleural lymphoma include antecedent autoimmune disease, such as Sjogren’s Syndrome, rheumatoid arthritis, malignant lymphoma (elsewhere in the body), chronic lymphocytic thyroiditis, thyroid lymphoma and Epstein-Barr virus (EBV) (3). Chronic pleural inflammation, either due to genetic factors or acquired immunodeficiency, leads to the unlimited proliferation of B-cell lymphocytes, and can eventually lead to the occurrence of pleural lymphoma. The location of the neoplasm in the parietal pleural and the lack of mediastinal and hilar lymph node swelling suggests that the parietal pleura is the most probable origin of the lymphoma.
The differential diagnosis of pleural effusion in a patient with primary SLL includes infection, pleural diseases and lymphatic obstruction. Primary pleural lymphomas are extremely rare and in a series reported by Burgener and Hamlin, pleural plaques were seen in less than 4% of patients (9). Primary pleural lymphoma needs to be differentiated from other pleural diseases like pleural mesothelioma, which can occur diffusely at any place in the pleura without enlarged mediastinal and hilar lymph nodes. Kawashima (9) et al. reported that the CT scan of a malignant pleural mesothelioma always shows widespread pleural involvement, reduced lung volume, adhesions between the parietal and visceral pleura, and the presence of wavy thickening and nodules. In our patient, the primary pleural lymphoma manifested as an uneven pleural neoplasm with varying degrees of mass effect causing dyspnea. The chest was partially collapsed and the two pleural layers were separated by the effusion. Additionally, the parietal pleura was involved heavily, which was entangled in many swollen mediastinal and hilar nodes. Pleural metastases often occur in lung cancer, breast cancer and aggressive thymoma, and may directly infiltrate the pleura. The site of origin of the neoplasm can easily be determined in these cases because pleural metastases are often accompanied by changes in the adjacent ribs. However, in pleural lymphoma, this change is not commonly identified and thus the diagnosis is both complex and rare.
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- King RM, Pairolero PC, Trastek VF, et al. Primary chest wall tumors: factors affecting survival. Ann Thorac Surg 1986;41:597-601. [PubMed]
- Alexandrakis MG, Passam FH, Kyriakou DS, et al. Pleural effusions in hematologic malignancies. Chest 2004;125:1546-55. [PubMed]
- Hirai S, Hamanaka Y, Mitsui N, et al. Primary malignant lymphoma arising in the pleura without preceding long-standing pyothorax. Ann Thorac Cardiovasc Surg 2004;10:297-300. [PubMed]
- Giardino A, O’Regan KN, Hargreaves J, et al. Primary pleural lymphoma without associated pyothorax. J Clin Oncol 2011;29:e413-5. [PubMed]
- Kawashima A, Libshitz HI. Malignant pleural mesothelioma: CT manifestations in 50 cases. AJR Am J Roentgenol 1990;155:965-9. [PubMed]
- Kosaka M, Koizumi T, Fukushima T, et al. Mantle cell lymphoma mainly involving thoracic lesions: two case reports. Intern Med 2011;50:1477-81. [PubMed]
- Ahmad H, Pawade J, Falk S, et al. Primary pleural lymphomas. Thorax 2003;58:908-9. [PubMed]
- Jaffe ES, Harris NL, Stein H, et al. eds. World Health Organization Classification of tumors: pathology and genetics of tumors of haematopoietic and lymphoid tissues. Lyon, France: IARC Press, 2001.
- Parnell AP, Frew I. Case report: non-Hodgkin’s lymphoma presenting as an encasing pleural mass. Br J Radiol 1995;68:926-7. [PubMed]


