Neo-adjuvant chemotherapy in early stage non-small cell lung cancer
Neo-adjuvant or preoperative chemotherapy is still considered an experimental modality of treatment mainly because it has been evaluated in only a small number of randomized trials, exploring the safety and activity of different platinum regimens. Theoretically the neo-adjuvant approach has a number of advantages: it can reduce the tumour volume and facilitate the control of micro-metastatic diffusion or prevent it; The neo-adjuvant treatment allows a careful evaluation of chemotherapy response giving critical information on tumour biology in adequate tumour samples: the compliance of chemotherapy in untreated patients is certainly better than after surgery and its dose intensity higher. On the other hand, its toxicities and a delay to surgery could be disadvantages, although up to now these issues seem to be scarcely relevant.
A meta-analysis (1) based upon seven trials involving 988 patients suggested that neo-adjuvant chemotherapy improved survival with a HR of 0.82 (95% CI: 0.69-0.97), equivalent to an absolute benefit of 6% at 5 years. They furthermore found an incremental benefit by stage: stage IA: +4%, stage IB: 6%; stage II-III: +7%, but did not observe any interaction between the kind of platinum-containing regimen or the kind of adjuvant treatment (chemo- or radiotherapy). The exploratory nature of these subgroup analyses warrants an IPD approach, which is ongoing. When the mature results of the European Intergroup trial added to the previous meta-analysis a shift of the hazard ratio observed to 0.87, with loss of the significance of the improvement in outcome.
The range of results observed with neo-adjuvant chemotherapy is illustrated by several contemporary phase III trials:
In a French trial, 355 patients with non-small-cell lung cancer (NSCLC) (stage IB, II, or IIIA, including 35% with N2 disease) were randomly assigned to surgery with or without two cycles of preoperative cisplatin-based chemotherapy (2). Responding patients were eligible for postoperative chemotherapy, as well. Neo-adjuvant chemotherapy was associated with a trend toward a longer median disease-free survival (P=0.15). At a median follow-up of 14 years, the 10-year recurrence-free survival rate was significantly increased with chemotherapy plus surgery compared to surgery alone (HR 0.78, 95% CI: 0.62-0.98) (3). There was a trend toward increased overall survival with neo-adjuvant chemotherapy compared to surgery alone (P=0.12), and the difference was statistically significant when multivariate analysis incorporated age, T stage, and N stage (HR 0.69, 95% CI: 0.64-0.90).
In the multicentre European LU22 trial, 519 patients with resectable NSCLC were randomly assigned to three cycles of platinum-based chemotherapy followed by surgery or to immediate surgery (4). At randomization, 93% of patients had clinical stage I or II disease. The chemotherapy regimen varied at different sites; the two most widely used combinations were vinorelbine plus cisplatin and gemcitabine plus cisplatin. Overall 75% of patients completed all three cycles of chemotherapy, and the objective response rate to chemotherapy was 47%. Despite the observed antitumor activity from chemotherapy, there was no improvement in PFS with neo-adjuvant treatment (HR for recurrence 0.96, 95% CI: 0.77-1.21). Similarly, there was no improvement in overall survival with preoperative chemotherapy (five-year survival 44% versus 45%, HR for death 1.02, 95% CI: 0.80-1.31). Results were not reported as a function of stage. The negative results in this trial may be attributed to the very high percentage of patients enrolled with stage I disease. This trial also underscores the difficulties in accurately staging patients preoperatively, as 59% of patients on the control arm (surgery alone) had either pathological upstaging or down-staging at the time of surgery.
In Southwest Oncology Group trial SWOG 9900, 354 patients with resectable stage IB-IIIA NSCLC were randomly assigned to three cycles of chemotherapy with paclitaxel plus carboplatin followed by surgery or immediate surgery (5). PFS was prolonged with neo-adjuvant chemotherapy compared to immediate surgery (HR 0.80, 95% CI: 0.619-1.04). Overall survival was also non-significantly longer with neo-adjuvant chemotherapy (median 62 versus 41 months, HR 0.79, 95% CI: 0.60-1.06). The trial was terminated prematurely when positive results were obtained in large trials using adjuvant chemotherapy.
Neo-adjuvant and adjuvant chemotherapy were compared to surgery alone in the three-armed NATCH trial (6). In this trial, 624 patients with IA, IB, II, or III (T3N1) NSCLC were randomly assigned to surgery alone, neo-adjuvant chemotherapy followed by surgery, or surgery followed by adjuvant chemotherapy. Chemotherapy consisted of three cycles of paclitaxel plus carboplatin. Compliance with chemotherapy was significantly higher with neo-adjuvant rather than adjuvant chemotherapy (90% versus 61% receiving three cycles of chemotherapy). Despite this, there were no significant differences in the five-year disease-free survival rates (34%, 38%, and 37% for surgery alone, neo-adjuvant chemotherapy, or adjuvant chemotherapy, respectively) or five-year overall survival rates (44%, 47%, and 46%, respectively) possibly due to the predominance of stage I patients.
A smaller European trial randomly assigned 141 patients to chemotherapy with gemcitabine plus cisplatin followed by surgery or to surgery alone (7). There was a trend toward improved overall three-year survival with the combined modality approach (P=0.053). In a subset analysis, the benefits appeared to be limited to patients with stage IIB/IIIA disease (three-year overall survival 70% versus 47%). The trial was terminated prematurely when positive results were obtained in large trials using adjuvant chemotherapy.
A common feature of these trials is that they have all been confronted with accrual problems, leading in some studies to their early closure, when the results of randomized trials showing a benefit of adjuvant chemotherapy were published.
Besides their low power and accrual, these trials have two further weaknesses in common: the survival in their control arms treated with immediate surgery is better than initially estimated, confounding the under-powering caused by the early closure of these trials; stage I (clinical or pathological) accounted for >50% of the enrolment and hence of the better than expected survival. As the accumulated evidence in the adjuvant setting has not found a statistically significant survival benefit for adjuvant chemotherapy in stage I disease, the implication of this finding in the neo-adjuvant setting might imply that a possible benefit for higher stages has been diluted by the majority of stage I cases (8).
Decisions on giving neo-adjuvant chemotherapy depend upon accurate clinical staging, while the decision to give adjuvant therapy is based upon the more accurate pathologic staging. Although 98% of patients in the NATCH trial had clinical stage I or II disease at protocol entry, 28% of those who underwent immediate surgery (with or without adjuvant chemotherapy) were reclassified as pathologic stage III based upon surgical findings.
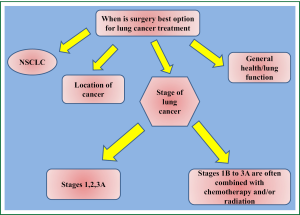
The results of these trials and the meta-analysis do not support the use of a neo-adjuvant approach in stage I, II rather than immediate surgery with postoperative adjuvant chemotherapy for patients with resectable NSCLC (9) (Figure 1).
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- Burdett S, Stewart LA, Rydzewska L. A systematic review and meta-analysis of the literature: chemotherapy and surgery versus surgery alone in non-small cell lung cancer. J Thorac Oncol 2006;1:611-21. [PubMed]
- Depierre A, Milleron B, Moro-Sibilot D, et al. Preoperative chemotherapy followed by surgery compared with primary surgery in resectable stage I (except T1N0), II, and IIIa non-small-cell lung cancer. J Clin Oncol 2002;20:247-53. [PubMed]
- Westeel V, Milleron BJ, Quoix EA, et al. Long-term results of the French randomized trial comparing neoadjuvant chemotherapy followed by surgery versus surgery alone in resectable non-small cell lung cancer. J Clin Oncol 2010;28:abstr 7003.
- Gilligan D, Nicolson M, Smith I, et al. Preoperative chemotherapy in patients with resectable non-small cell lung cancer: results of the MRC LU22/NVALT 2/EORTC 08012 multicentre randomised trial and update of systematic review. Lancet 2007;369:1929-37. [PubMed]
- Pisters KM, Vallières E, Crowley JJ, et al. Surgery with or without preoperative paclitaxel and carboplatin in early-stage non-small-cell lung cancer: Southwest Oncology Group Trial S9900, an intergroup, randomized, phase III trial. J Clin Oncol 2010;28:1843-9. [PubMed]
- Felip E, Rosell R, Maestre JA, et al. Preoperative chemotherapy plus surgery versus surgery plus adjuvant chemotherapy versus surgery alone in early-stage non-small-cell lung cancer. J Clin Oncol 2010;28:3138-45. [PubMed]
- Scagliotti GV, Pastorino U, Vansteenkiste JF, et al. A phase III randomized study of surgery alone or surgery plus preoperative gemcitabine-cisplatin in early-stage non small cell lung cancer: follow-up data of CH.E.S.T. J Clin Oncol 2008;26:abstr 7508.
- Crinò L, Weder W, van Meerbeeck J, et al. Early stage and locally advanced (non-metastatic) non-small-cell lung cancer: ESMO clinical practice guidelines for diagnosis, treatment and follow-up. Ann Oncol 2010;21:v103-15. [PubMed]
- Bradbury PA, Shepherd FA. Chemotherapy and surgery for operable NSCLC. Lancet 2007;369:1903-4. [PubMed]