Surgical outcome of esophageal tuberculosis secondary to mediastinal lymphadenitis in adults: experience from single center in China
Introduction
Dysphagia is a common complaint, which refers to difficulty in eating as a result of disruption in the swallowing process. It can range from mild to serious forms leading to complications like malnutrition, weight loss and dehydration. Any condition involved the esophagus can manifest as dysphagia. Esophageal tuberculosis (ET) is an extremely rare entity, even in countries where tuberculosis is highly prevalent (1). Typically, it is caused by direct extension of contiguous structures, such as mediastinal lymph nodes, lung or spine. Primary ET is even rarer (2). Clinically, differential diagnosis of ET from esophageal carcinoma is so difficult (3) that some cases may be misdiagnosed and result in unessential esophagectomy, which easily occurred especially in China with the highest mortality of esophageal carcinoma around the world (4). Early and accurate diagnosis of tuberculosis not only facilitates prompt treatment but also prevents complications. However, the gold standard of the diagnosis of tuberculosis is the isolation of tuberculous mycobacterium or the detection by polymerase chain reaction (5). Histological or bacteriological examination often fails to establish a reliable diagnosis. Although endoscopic ultrasonography (EUS) and fine-needle aspiration (FNA) can improve the accuracy of diagnosis, the positive rate of tubercle bacilli cultured or caseous necrosis presented is even lower. As a result, tentative antituberculous treatment is usually applied for the suspicious patients. This is the main cause of the multidrug-resistant tuberculosis worldwide and should be avoided as much as possible (6). Most of reports on ET pertain to individual nonsurgical treatment cases. The purpose of this study is to highlight the importance of video-assisted thoracoscopic surgery (VATS) or traditional thoracotomy surgery in the diagnosis and treatment of ET secondary to mediastinal tuberculosis lymphadenitis and associated complications.
Patients and methods
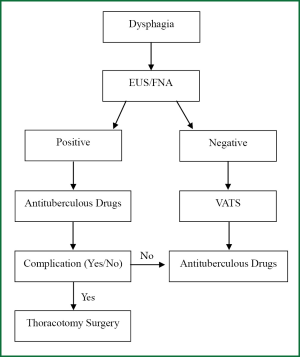
Six patients were identified in our department between June 2006 and June 2011. Clinical data were reviewed, including symptoms, physical and laboratory examination. All patients were performed with radiological imaging, esophagoscopy, EUS and/or FNA. Surgical procedures were carried out when patients could not definitely diagnosed or associated with complications after antituberculous treatment. Confirmative diagnosis of tuberculosis was defined by isolation of tuberculous mycobacterium and staining of acid-fast bacilli with Ziehl-Neelsen method from surgical biopsy specimens. Antituberculous regimens were applied according to the results of drug-sensitive test (Figure 1).
Results
Clinical features
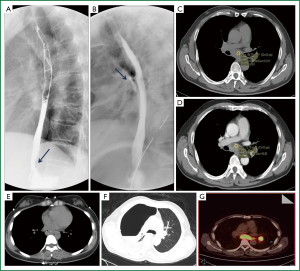
We reviewed 2,019 cases admitted in our department due to dysphagia as main presentation between June 2006 and June 2011, which included 1,679 patients with esophageal carcinoma, 334 with benign esophageal conditions, and only 6 (0.30%) with ET secondary to mediastinal tuberculosis lymphadenitis. These 6 patients aged from 28 to 71 years, including 4 females and 2 males. All of them presented with progressive dysphagia for solids with duration ranged from 2 weeks to 2 months. Weight loss was presented in 4 patients, retrosternal pain in one, epigastric pain in one, and fever with cough in one. One suspicious tuberculosis patient (No 5) complained dyspnea after one-month antituberculous drug treatment. None of them had a history of contact with tuberculosis. One had diabetes mellitus, one had cirrhosis induced by hepatitis B and coronary heart disease, one had hepatitis A and cholecystolithiasis, and the other three had normal medical history. The result of tuberculin skin test, performed with purified protein derivative (PPD) was positive only in one case. Outcome of laboratory testing revealed that erythrocyte sedimentation rate (ESR) ranged from 4 to 55 mm/h, live function were normal, HIV screening were negative, and repeated sputum acid-fast bacilli stain were negative (Table 1). Physical examination did not found pathological sign in all cases.
Full Table
Views of esophagoscopy
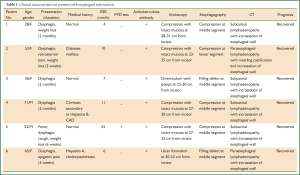
Involvement of esophagus were observed at middle (n=5) and lower segment (n=1). Esophagoscopy demonstrated that diverticulum with polyps in one patient, ulcer formation in one, and extraneous compression with intact mucosa in four (Figure 2A,B,C).
EUS was applied in all patients. The main features were round or oval shaped swollen lymph nodes around the esophagus with hypoechoic center, ambiguous border between the mass and esophagus due to infiltration of the inflammatory mediastinal lymph nodes that resulted in interruption of esophageal adventitia (Figure 2D,E). Endoscopic biopsy was performed in the ulcerative mass, histopathology described granulomatous inflammation without caseous necrosis, and acid-fast bacilli were not found in Ziehl-Neelsen stain. Two patients mimicking submucosal tumor underwent EUS-FNA, but the cytological results were negative.
Radiological findings
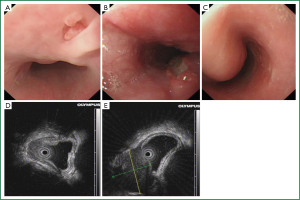
Preoperative chest radiograph of all patients showed normal manifestation. Barium or gastrografin esophagographies demonstrated extrinsic compression in 4 cases including 3 at subcarinal level and one at lower segment (Figure 3A), and filling defect in 2 cases. Contrast leakage into mediastinum could be seen in one patient (No 5) after one-month antituberculous treatment (Figure 3B).
Thoracic computed tomography (CT) revealed subcarinal or paraesophageal lymphadenopathy with incrassation of esophageal wall, some indicated heterogeneous density with mottling calcification, majority of them with peripheral thin rim enhancement with hypodensity in the central area (Figure 3C,D,E). A rare imaging of CT pertaining to patient No 5 who underwent tuberculostatic drug treatment for one month, which demonstrated pneumothorax, pleural effusion, and atelectasis in the right chest (Figure 3F). The patient also obtained an 18F-fluorodeoxyglucose (18F-FDG) positron emission tomography (PET)/CT scan showing focal hot uptaking lesions in subcarinal area and hilus of the left lung with max standardized uptake value (SUV) up to 16.5 (Figure 3G).
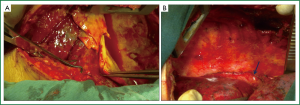
Surgical management
All patients underwent general anesthesia with double lumen endotracheal tube, and single lung ventilation were carried out during operations. The patients were placed in left lateral position. Right VATS were performed in five patients who couldn’t be distinguished from other conditions. For the VATS procedure, a camera port was placed in the 7th intercostal space on the mid-axillary line with incision 1 cm long. Two other utility incisions, each approximately 2 cm long, were made in the 4th intercostal space on the anterior axillary line and in the 6th or 7th intercostal space on the subscapular line. Rib spreading was not used, and all surgical procedures were done under complete VATS. The enlarged lymph nodes were excised while the margin between esophagus and the mass was not unclear, otherwise enucleation and drainage only performed. The patient diagnosed with esophagopleural fistula underwent a traditional right posterolateral thoracotomy through the fifth intercostal space. Yellow pyoid effusion covered all surface of the right lung and parietal pleura was found during operation (Figure 4A). After debridement, a fistula positioned at the right anterior of esophageal wall beneath arch of azygous vein was detected. We repaired the fistula by mattress suture with 3-0 vicryl, and interposed a pedicled diaphragm muscle flap on it (Figure 4B). Air inflation into esophagus were implemented in all operations in order to confirm no existence of fistula.
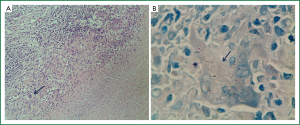
Histopathological and microbiological findings
Surgical specimens were performed for histopathological and microbiological examinations. Typical epithelioid cell granuloma with central caseous necrosis and marginally surrounded by Langhans’ giant cells be identified from microscope in all specimens (Figure 5A). Acid-fast bacilli were found in the caseating tissue by Ziehl-Neelsen stain, and some appeared within the Langhans’ gaint cells (Figure 5B). Mycobacterium tuberculosis was isolated from culture medium, and sensitivity test revealed that multidrugs resistant mycobacterium tuberculosis was cultured from the specimen of patient No 5.
Postoperative management and follow up
While tuberculosis was confirmed, following treatment with sensitive tuberculostatic drugs. Postoperative management of patient No 5 might be special, rinsing the right pleural cavity with isoniazid, metronidazole and iodophors for one week until the drainage was clear and no new fistula occurred which confirmed by esophagography, and meanwhile intravenous dripped with isoniazid, etimicin, amoxicillin and levofloxacin according to the result of sensitivity test. Nasogastric or nasoduodenal feeding tube was imperative that could allow for delivery of nutrition and administration of medications. After surgery, dysphagia of the patients eliminated immediately, and discharged without clinical symptoms. Follow-up was available for all patients. Six months after the therapy initiation, CT and esophagoscopy showed the esophageal lesions and mediastinal lymph nodes enlargement had completely resolved. All patients are healthy without any complaints and still have no recurrence after followed up for 12 to 45 months.
Discussion
ET is an extremely rare condition, accounting for 0.15% of patients who died of tuberculosis. Another study reported that only 12 (0.55%) patients with esophageal tuberculosis identified in 2,176 patients with persistent dysphagia (1). The prevalent rate of 0.30% in present report was approximate to the previous researches. ET can be categorized into two types including secondary and primary, the latter one is much more scarce. The leading mechanisms consist of stratified epithelial lining overlaying with saliva, high motility due to peristalsis of esophagus, and antireflux effect attribute to upright posture and intact lower esophageal sphincter (7). The extrinsic compression of mediastinal or hilar lymph nodes considered as the most frequent cause of secondary esophageal tuberculosis. The middle third segment is the prefer site of esophageal involvement, because of its proximity to the bifurcation of the trachea (1,8).
Clinical symptoms are often highly variable. Dysphagia is the primary complaint followed with weight loss, retrosternal pain, odynphagia, and epigastric pain (9). All patients in this report presented with dysphagia. Difficulties in differential diagnosis often occur due to ET mimicking the symptoms of carcinoma, especially in China where esophageal cancer widely prevailed.
Radiological examinations are frequently essential. Esophagography almost always presents segmental stenosis with filling defect, but it defects specific manifestation. Thoracic contrast enhanced CT typically reveals mediastinal or hilar lymphadenopathy contiguous to esophagus with appearance of thin rim enhancement with hypodensity in the central area (10). There is hardly any report about delineation of PET/CT imaging of ET. 18F-FDG-PET scanning of the present case indicated focal hot uptake lesions locating in the subcarinal and hilar areas with the max SUV up to 16.5, mimicking the imaging of esophageal carcinoma accompanying lymph nodes metastasis. The role of PET in the diagnosis of ET has not been clearly studied. Although FDG uptake is often consistent with increased metabolic activity, which not specific and may present in both inflammatory lesions and malignant tumors. The high uptake of FDG may be attributed to incremental intracellular glycolysis of inflammatory cells in the tuberculosis granuloma. Suspicions should be made when differentiating between benign and malignant conditions, because of the false positive of PET (11,12).
Esophagoscopy plays a crucial role in the definitive diagnosis of ET. Esophageal ulcer is the most common macroscopic finding (13), but only two in six patients of this study present ulceration and the others as submucosal tumor. We consider this may correlate to the duration of disease, involved segment of esophagus, and pathological stage of the adjacent tuberculosis lymph nodes. Although we confirm diagnosis mainly by the endoscopic biopsy, the specific view of granuloma with caseating necrosis seen uncommonly. This may relate to the low density of tuberculous granuloma in the involved esophageal mucosa. The requirement of multiple and deep biopsy specimens was highlighted, precipitating the utility of EUS/FNA in the diagnosis of ET. Relatively specific features were found from EUS, including masses with homogeneous or heterogeneous hypoechoic infiltrated the esophagus, incrassation of esophageal wall, and disruption of esophageal adventitia (14). The safety and efficacy of FNA is not well known, in spite of few reports advocate the utility in the investigation of mediastinal tuberculosis lymphadenitis (15). However complication such as mediastinal-esophageal fistula reported, and low positive rate also existed (16).
Histopathological and microbiological findings are the bases of definite diagnosis. However clinically positive rate is low, resulting in the majority of suspicious patients tentatively treated with antituberculous drugs. This is the main cause of the multidrug-resistant tuberculosis worldwide and should be avoided as much as possible. VATS is extensively applied in the diagnosis and treatment of thoracic diseases in recent years. We successfully diagnosed the present cases and alleviated the dysphagia through VATS by excision and excavation of the swollen mediastinal lymph nodes. The positive rate improved significantly might due to the increased quantity of specimens and reserved their integrity (17). Some surgical maneuvers should take care, attempt to completely dissect the lymph nodes from the infiltrated esophagus must be avoided if the border of them unclear, which may induce injury the lamina muscularis result in esophageal perforation. Air inflated into esophagus through a gastric tube to confirm no fistula occurred.
Esophagomediastinal and esophagobronchial fistula are the most commonly reported complications of ET. Most likely these correlate to inflammatory reaction and erosion of tuberculous lymph nodes resulting in pressure necrosis and eventually perforation occurred (18). However, patient No 5 represents the perforation of esophagus to the right pleural cavity. To our knowledge, it may be the first case of this rare complication. The high mortality of esophageal perforation usually mandates the consideration of surgical management. The preferred operative strategies include debridement of inviable tissue, closure of the esophageal defect, interposition of muscle flap, drainage and rinsing. Nutrition maintained through nasoduodenal or jejunostomy tube is imperative for the recovery of patients (19).
Conclusions
ET is easily misdiagnosed due to mimicking presentation like other conditions. Application of VATS can improve rate of definitive diagnosis and resolve the dysphagia promptly. Traditional thoracotomy operation is reserved for treatment complications like esophagomediastinal or esophagobronchial fistula.
Acknowledgements
This work was funded by the Priority Academic Program Development of Jiangsu Higher Education Institutions [JX10231801].
Disclosure: The authors declare no conflict of interest.
References
- Jain SK, Jain S, Jain M, et al. Esophageal tuberculosis: is it so rare? Report of 12 cases and review of the literature. Am J Gastroenterol 2002;97:287-91. [PubMed]
- Wort SJ, Puleston JM, Hill PD, et al. Primary tuberculosis of the oesophagus. Lancet 1997;349:1072. [PubMed]
- Musoğlu A, Ozütemiz O, Tekin F, et al. Esophageal tuberculosis mimicking esophageal carcinoma. Turk J Gastroenterol 2005;16:105-7. [PubMed]
- Guo P, Li K. Trends in esophageal cancer mortality in China during 1987-2009: age, period and birth cohort analyzes. Cancer Epidemiol 2012;36:99-105. [PubMed]
- Fujiwara T, Yoshida Y, Yamada S, et al. A case of primary esophageal tuberculosis diagnosed by identification of Mycobacteria in paraffin-embedded esophageal biopsy specimens by polymerase chain reaction. J Gastroenterol 2003;38:74-8. [PubMed]
- Dooley KE, Obuku EA, Durakovic N, et al. World Health Organization group 5 drugs for the treatment of drug-resistant tuberculosis: unclear efficacy or untapped potential? J Infect Dis 2013;207:1352-8. [PubMed]
- Grubbs BC, Baldwin DR, Trenkner SW, et al. Distal esophageal perforation caused by tuberculosis. J Thorac Cardiovasc Surg 2001;121:1003-4. [PubMed]
- Gomes J, Antunes A, Carvalho A, et al. Dysphagia as a manifestation of esophageal tuberculosis: a report of two cases. J Med Case Rep 2011;5:447. [PubMed]
- Newman RM, Fleshner PR, Lajam FE, et al. Esophageal tuberculosis: a rare presentation with hematemesis. Am J Gastroenterol 1991;86:751-5. [PubMed]
- Nagi B, Lal A, Kochhar R, et al. Imaging of esophageal tuberculosis: a review of 23 cases. Acta Radiol 2003;44:329-33. [PubMed]
- Aragon-Ching JB, Akin EA. Positron emission tomography findings in clinical mimics of lymphoma. Ann N Y Acad Sci 2011;1228:19-28. [PubMed]
- Netherland NA, Peter S. Education and Imaging. Gastrointestinal: positron emission tomography (PET) in intestinal tuberculosis: masquerading hot spots. J Gastroenterol Hepatol 2009;24:1798-9. [PubMed]
- Abid S, Jafri W, Hamid S, et al. Endoscopic features of esophageal tuberculosis. Gastrointest Endosc 2003;57:759-62. [PubMed]
- Han XM, Yang JM, Xu LH, et al. Endoscopic ultrasonography in esophageal tuberculosis. Endoscopy 2008;40:701-2. [PubMed]
- Fritscher-Ravens A, Ghanbari A, Topalidis T, et al. Granulomatous mediastinal adenopathy: can endoscopic ultrasound-guided fine-needle aspiration differentiate between tuberculosis and sarcoidosis? Endoscopy 2011;43:955-61. [PubMed]
- von Bartheld MB, van Kralingen KW, Veenendaal RA, et al. Mediastinal-esophageal fistulae after EUS-FNA of tuberculosis of the mediastinum. Gastrointest Endosc 2010;71:210-2. [PubMed]
- Welzel TM, Kawan T, Bohle W, et al. An unusual cause of dysphagia: esophageal tuberculosis. J Gastrointestin Liver Dis 2010;19:321-4. [PubMed]
- Devarbhavi HC, Alvares JF, Radhikadevi M. Esophageal tuberculosis associated with esophagotracheal or esophagomediastinal fistula: report of 10 cases. Gastrointest Endosc 2003;57:588-92. [PubMed]
- Shen KR, Allen MS, Cassivi SD, et al. Surgical management of acquired nonmalignant tracheoesophageal and bronchoesophageal fistulae. Ann Thorac Surg 2010;90:914-8; discussion 919. [PubMed]