Complete versus culprit only revascularization in ST-elevation myocardial infarction—a perspective on recent trials and recommendations
Introduction
There has been a recent decline in the incidence of ST-elevation myocardial infarction (STEMI) (1,2). However, multivessel (MV) coronary artery disease (CAD) is frequently encountered (45–60%) in patients undergoing primary percutaneous coronary intervention (PCI) for STEMI (3-6). In contrast to stable lesions in stable CAD, non-culprit lesions in patients with acute coronary syndrome (ACS) tend to have more diffuse CAD and less-calcified plagues (7,8). The plaques in ACS patients are also more vulnerable, with large amount of necrotic core (7) and thin-cap fibroatheromas, consistent with high-risk features. This could potentially lead to development of future major adverse cardiovascular events (9). The presence of MV-CAD is strongly associated with higher 30-day mortality, reduced myocardial reperfusion success, reinfarction, and occurrence of major adverse cardiac events (MACE) at 1-year compared with single vessel CAD (4-6).
Despite higher morbidity and mortality in patients with STEMI and coexistent MV CAD, guidelines published by the American College of Cardiology/American Heart Association (ACC/AHA) in 2013 recommended against PCI on non-culprit lesions at the time of primary PCI in patients with STEMI who are hemodynamically stable (10). The 2014 European Society of Cardiology/European Association of Cardio-Thoracic Surgery guidelines also similarly recommend systematic primary PCI of the culprit vessel and advocate for additional non-culprit vessel revascularization only in patients with cardiogenic shock, especially when the lesions are multiple, unstable, or with critical stenosis, and if persistent ischemia exists after PCI of the culprit lesion (11). However, only 25% of patients with cardiogenic shock and MV CAD receive MV PCI during STEMI (12).
The recommendations against PCI of non-culprit lesions were largely driven by results of nonrandomized observational studies with conflicting results. The rationale behind not recommending routine complete revascularization was increased in-hospital mortality, contrast-induced nephropathy (CIN), and MACEs associated with MV-PCI during the index procedure (13-17). Small randomized controlled trials (RCTs) reported potential safety and benefits of complete and staged revascularization in reducing long-term MACE (18,19). In multicenter randomized Hepacoat for Culprit or Multivessel Stenting for Acute Myocardial Infarction (HELP-AMI) study (19), with a total of 69 patients (17 patients in culprit-only PCI group and 52 patients in multivessel PCI group), the investigators found that MVPCI at the time of index procedure was not associated with increase in in-hospital adverse events and had similar overall healthcare cost as compared to culprit-only PCI (19). In the Primary Angioplasty in Patients Transferred From General Community Hospitals to Specialized PTCA Units With or Without Emergency Thrombolysis (PRAGUE-13) trial (20), the authors compared staged MV-PCI (n=106) with culprit-only PCI (n=108) in STEMI patients with MV-CAD. This study found no difference in the long term development of composite primary end-point of all-cause mortality, non-fatal MI, and stroke between the two revascularization strategies (20).
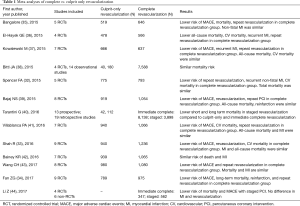
The presence of MV-CAD often poses a therapeutic dilemma for interventional cardiologists as there are multiple options in patients with MV-CAD and insufficient data regarding benefit in reducing end-point such as mortality and MI. These options are culprit artery-only primary PCI, complete revascularization (MV-PCI) at the time of index procedure, or staged revascularization (primary PCI followed by ischemia or symptom guided PCI of the non-culprit lesion within days or weeks after primary PCI). In this review, we will discuss the recently published RCTs (Table S1) designed to investigate optimal revascularization strategy in managing STEMI patients with MV-CAD and their impact on current clinical practice and guidelines.
RCTs (Table S1)

Full table
Politi et al. (18)
Out of a total of 263 consecutive patients with STEMI and MV-CAD, 214 patients were randomly assigned to culprit-only PCI (n=81), complete revascularization during the index procedure (n=65), and staged revascularization performed approximately two months after the index procedure (n=65) (18). Patients with cardiogenic shock at presentation (systolic blood pressure ≤90 mmHg despite drug therapy), left main coronary disease (≥50% diameter stenosis), previous coronary artery bypass graft (CABG) surgery, severe valvular heart disease and unsuccessful revascularization were excluded from the study. Patients were followed for a mean duration of 2.5±1.4 years (18).
The investigators found that culprit-only revascularization had a higher rate of at least one MACE (50%), compared to staged revascularization (20%) and immediate complete revascularization (23%) at a mean follow-up of 2.5 years (P<0.001). The staged and immediate complete revascularization group had a 63% (P=0.003) and a 60% lower risk of MACE (P=0.002), respectively. This result was mainly driven by a lower incidence of in-hospital death, re-PCI, and rehospitalization. Kaplan-Meier analysis showed a worse outcome in the culprit-only revascularization group (worse survival-free of MACE, survival-free of re-PCI), but no significant difference in outcomes between the staged and immediate complete revascularization groups. There were no significant differences in CIN incidence and length of hospital stay between the 3 study groups (18). This study suffered from a small sample size and utilization of unrestricted randomization instead of block randomization leading to imbalances in the treatment arms (25). It was also unclear whether patients in the culprit-only revascularization group had any non-invasive ischemia testing within 2.5 years, which could qualify these patients for staged revascularization. This could potentially explain the higher incidence of repeat revascularization and re-hospitalization in the culprit-only revascularization group (26).
PRAMI (21)
In the Preventive Angioplasty in Acute Myocardial Infarction (PRAMI) trial, a total of 465 patients were randomly assigned to culprit only revascularization (n=231) and complete revascularization during the index procedure (n=234) (21). Staged revascularization in the asymptomatic patients was discouraged. Once the infarct-related artery was treated, the patients were included in the trial if they had a PCI-amenable ≥50% stenosis in one or more non-infarct-related coronary arteries. Patients who were in cardiogenic shock, unable to provide consent, had undergone previous CABG, had a non-infarct stenosis of 50% or more in the left main stem or the ostia of both the left anterior descending and circumflex arteries, or if the only non-culprit stenosis was a chronic total occlusion were excluded. Patients were followed for a mean follow-up duration of 23 months (21).
This study reported a 65% reduction in the primary endpoint in the complete revascularization group compared to the culprit-only revascularization group. Complete revascularization group also had a significantly lower risk for repeat revascularization and composite of death from cardiac causes or non-fatal MI. The Kaplan-Meier analysis showed that the risk reduction benefit was apparent within 6 months after the procedure (21). This study, however, failed to address the question whether similar benefit could be obtained when PCI was performed as a delayed procedure (staged revascularization) (27).
DANAMI-3 PRIMULTI (22)
In The Third Danish Study of Optimal Acute Treatment of Patients with STEMI: Primary PCI in Multivessel Disease (DANAMI-3 PRIMULTI), 627 patients were randomly allocated to complete revascularization (n=314) and culprit only revascularization (n=313) (22). After successful PCI of the culprit lesion, patients with an angiographic diameter stenosis of greater than 50% in one or more non-infarct related arteries were included in the trial. Patients were excluded if they were intolerant of contrast media or of relevant anticoagulant or antithrombotic drugs, unconscious or suffered from cardiogenic shock, stent thrombosis, met indication for CABG, or had an increased bleeding risk. Complete revascularization was performed in a staged manner 2 days after the index procedure during the index hospitalization, and was guided by fractional flow reserve (FFR), if appropriate. In non-culprit lesions with a greater than 50% diameter stenosis, FFR values were calculated (FFR ≤0.8 considered significant) (22).
One-third of patients allocated to the complete revascularization group did not receive PCI as they had FFR values >0.80. The investigators found that complete revascularization was associated with a 44% reduction in the incidence of the composite primary endpoint, which was largely driven by a 69% reduction of ischemia-driven revascularization of the non-infarct related arteries. There were no significant differences in the all-cause mortality and non-fatal reinfarction rates between the 2 groups. There were also no significant differences in cardiovascular death or non-fatal MI, although complete revascularization was significantly associated with a lower need for both urgent and non-urgent PCI of the lesions in the non-culprit arteries (22). This trial failed to show an impact on hard outcomes (such as death and MI due to lack of power). The optimal timing of non-infarct related artery PCI (index admission versus staged outpatient procedure) remains a debate (28,29).
CvLPRIT (23)
The Complete versus Lesion-only Primary PCI (CvLPRIT) trial randomized 296 STEMI patients and MVCAD to culprit-only (n=146) and complete (n=150) revascularization (23). Exclusion criteria were an age <18 years, clear indication for, or contraindication to, MV primary PCI according to operator judgement, prior MI, patients with prior CABG, cardiogenic shock, ventricular septal rupture or moderate/severe mitral regurgitation, chronic kidney disease, suspected or confirmed thrombosis of a previously stented artery, and when the only significant non-infarct-related lesion is a chronic total occlusion (23).
Complete revascularization was done either during the index procedure or the index hospitalization (staged revascularization). The primary endpoint of this study was MACE, which was a composite of all-cause mortality, recurrent MI, heart failure, and ischemic-driven revascularization by PCI or CABG within 12 months. This study reported a 55% reduction of MACE in the patients undergoing complete revascularization compared to the culprit-only revascularization. The occurrence of individual components of the primary endpoint was insignificantly lower in the complete revascularization group. Sixty-four percent of patients underwent complete revascularization during the index procedure, while the others had a staged revascularization. Patients receiving complete revascularization during the index procedure had a trend towards a reduced prevalence of MACE compared to staged revascularization. There were no differences in the occurrence of adverse events, such as stroke, major bleeding (all non-CABG related), or CIN between the infarct-related revascularization and complete revascularization groups (23). The study was not powered to assess the individual components of the primary composite endpoint (30). The study did not include intravascular ultrasound or FFR for the non-infarct-related lesion characterization anatomically or physiologically, respectively.
Compare-Acute Trial (24)
The Comparison Between FFR Guided Revascularization Versus Conventional Strategy in Acute STEMI Patients With MVD (COMPARE-ACUTE) Trial enrolled 885 STEMI patients with non-infarct-related coronary stenosis of 50% or more (24). Patients were randomly assigned in a ratio of 1:2 to FFR-guided complete revascularization (n=295) and culprit-only revascularization (n=590). Exclusion criteria were left main CAD, chronic total occlusion, severe stenosis with a Thrombolysis in Myocardial Infarction (TIMI) flow grade of 2 or less in the non-infarct-related coronary artery, a suboptimal result or complication after treatment of infarct-related artery, severe valve dysfunction, and Killip class III or IV. Complete revascularization was performed in lesions with FFR ≤0.80, preferably within 72 hours (complete PCI was performed during index procedure in 83.4% patients). Primary end-point of the study was the composite of all-cause mortality, non-fatal MI, any revascularization, and cerebrovascular events (MACCE) at 12 months (24).
As the FFR measurement was performed in both groups, this study showed that approximately half of the patients had one or more non-infarct-related artery lesions with an FFR of 0.80 or less. The investigators found that complete revascularization group had significantly lower rate of MACCE compared to culprit-only revascularization group which seems to be driven mainly by the decreased need for revascularization. The other components of primary end-point (all-cause mortality, MI, and cerebrovascular event) did not differ statistically between both groups (24).
Although this study showed that FFR-guided revascularization could be safely performed in acute setting of STEMI and cost-effective, it is questionable whether the result of trial can also be applied to much sicker patient populations. In addition, there is a potential bias as the angiographic result of culprit-only revascularization group was made known to patients and cardiologist, which could contribute to higher subsequent revascularization among that group (31).
Meta-analyses
Spencer et al. (32) in their systematic review, which included five RCTs [RCT by Politi et al. (18), HELP-AMI (19), PRAMI (21), DANAMI-3 PRIMULTI (22), and CvLPRIT (23)] enrolling 1,606 patients, concluded that complete revascularization was associated with significant reduction in the risk of repeat revascularization, non-fatal MI, cardiovascular mortality compared to culprit-only revascularization. However, the investigators did not find any difference in the total mortality between the two groups (32). A separate meta-analysis which recruited nine RCTs with total 2,176 patients, agreed that complete revascularization strategy was overall better in lowering risk of MACE, repeat revascularization, cardiovascular mortality, but found no difference in mortality or recurrent MI. The investigators also compared the three revascularization strategies (culprit-only, complete revascularization at index procedure, and complete revascularization as staged procedure) and showed that complete revascularization during index procedure seemed to be more superior than two other strategies (33). However, more recent meta-analysis, conducted by Fan et al. (34), concluded the opposite: complete revascularization as staged procedure deemed better than immediate complete revascularization or culprit-only revascularization in reducing all-cause mortality (34).
Numerous other meta-analyses have been conducted and published since the RCTs (Table 1). They have discordant results, which was largely driven by the inclusion of different variety of trials to conduct the meta-analyses and by the fact that none of the RCTs were adequately powered for the hard outcomes of death and MI. Overall, MV-PCI seems to be associated with lower risk of MACE, repeat revascularization, but with a similar risks of recurrent MI and mortality compared to culprit-only revascularization (32-44).
Full table
Timing of revascularization
Timing of revascularization remains an area of intense controversy and debate. Wang et al. (43) performed a subgroup analysis in their meta-analysis, comparing outcomes in complete revascularization at the time of the index procedure (immediate complete revascularization) and staged revascularization with culprit-only revascularization. Immediate complete revascularization had a significantly lower incidence of MACE, all-cause death and/or MI, non-fatal MI, and repeat revascularization when compared to the culprit-only revascularization. Staged revascularization reduced only the incidence of MACE. This showed that immediate complete revascularization might be more superior compared to staged revascularization. This finding seems to be opposite of what was found in other meta-analyses (40,44) and the few observational studies (45,46).
Kornowski et al. (45) performed a post-hoc analysis of the Harmonizing Outcomes with Revascularization and Stents in Acute Myocardial Infarction (HORIZONS-AMI) trial. This was a RCT originally designed to compare bivalirudin versus heparin plus a glycoprotein IIb/IIIa inhibitor and paclitaxel-eluting stents versus bare-metal stents in patients undergoing primary PCI for STEMI. A total of 668 STEMI patients were identified to have undergone MV-PCI in the original trial. Two hundred and seventy-five patients underwent MV-PCI during the index procedure, whereas 393 patients underwent staged revascularization (6–50 days after primary PCI). This study showed that MV-PCI during index procedure was associated with an increased all-cause mortality [hazard ratio (HR) 4.1, 95% CI: 1.93–8.86, P<0.0001] and cardiovascular mortality (HR 3.41, 95% CI: 1.35–7.27, P=0.005) compared to the staged MV-PCI (45). Similarly, a meta-analysis by Tarantini et al. (40) revealed that staged revascularization was associated with short-and long-term survival compared with both immediate complete revascularization and culprit-only revascularization. In separate meta-analysis by Li et al. (44) which compared staged revascularization and immediate complete revascularization head-to-head, the former seemed to be a better strategy.
Iqbal et al. (46) performed an observational study which compared the 3 revascularization strategies (immediate complete revascularization, staged revascularization, and culprit-only revascularization) in 6,503 STEMI patients with MV-CAD. The primary outcome was all-cause mortality and repeat revascularization at 2 years. The investigators found that staged revascularization was associated with a lower mortality at 1 year and 2 years when compared with either immediate complete revascularization or culprit-only revascularization. This study also showed lower repeat revascularization rates at 30 days, 1 year, and 2 years when compared with culprit-only revascularization. The authors concluded that staged PCI of the non-culprit vessel (if indicated) may yield better results, and MV-PCI at time of index procedure may be considered in patients with non-culprit LAD disease (46).
Of the RCTs discussed in detail above, Politi et al. (18) was the only trial that included both staged and immediate complete revascularization and analyzed them separately. PRAMI (21) was the only trial that specifically compared MV-PCI at time of index procedure to culprit-only revascularization. DANAMI-3 PRIMULTI (22) compared only staged revascularization to culprit only-revascularization. CvLPRIT (23) and Compare-Acute Trial (24) combined both immediate and staged revascularization (mentioned as complete revascularization) at time of data analysis. The variability on how the trials were conducted leads to uncertainty and confusion on when and how complete revascularization should be performed. This warrants a larger scale RCT to confirm the present findings, as well as to determine the impact of such intervention on hard endpoints such as mortality or MI.
A large, ongoing, Complete vs. Culprit-only Revascularization to Treat Multivessel Disease After Primary PCI for STEMI (COMPLETE) trial (ClinicalTrials.gov. Identifier: NCT01740479) was designed to enroll 3,900 STEMI patients with MV-CAD randomly assigning them to receive either staged revascularization or culprit-only revascularization, on top of optimal medical therapy (including low dose aspirin and ticagrelor). This trial was started in December, 2012, and is estimated to be completed in December, 2018. The primary outcome of this study is a composite of cardiovascular death or new MI over a follow-up of approximately 4 years. The secondary outcome is a composite of cardiovascular death, new MI, ischemia-driven revascularization or hospitalization for unstable angina or heart failure. The results of this trial are expected to provide a better understanding of whether staged revascularization is better than culprit-only revascularization in STEMI patients with MV-CAD undergoing primary PCI.
2015 ACC/AHA focused update and 2016 ACC/AHA appropriate use criteria
The publication of larger scale RCTs has prompted ACC/AHA to change the recommendation for complete revascularization to class IIb in the recent 2015 ACC/AHA/SCAI Focused Update on Primary Percutaneous Intervention for Patients with ST-Elevation Myocardial Infarction (47). These guidelines specifically mention that PCI of a non-infarct artery may be considered in selected patients with STEMI and MV-CAD who are hemodynamically stable, either at the time of primary PCI or as a planned staged procedure (47).
The 2016 Appropriate Use Criteria for Coronary Revascularization in Patients with ACS also addressed the issue on how to treat MV-CAD in STEMI patients (48). Multivessel revascularization at the time of the index procedure with PCI or CABG was deemed appropriate in patient with cardiogenic shock persisting after PCI of the presumed culprit artery. Whereas revascularization of non-culprit artery during initial hospitalization (as staged procedure) was considered appropriate in MV-CAD patients with spontaneous or easily provoked symptoms of myocardial ischemia, asymptomatic patients with findings of ischemia on non-invasive testing, and asymptomatic patients with an intermediate (50–70%) stenosis and a FFR ≤0.8 (48).
Conclusions
In conclusion, it seems prudent to consider MV-PCI at the time of the index procedure in patients with cardiogenic shock, severe left ventricular dysfunction and hemodynamic instability. MV-PCI at the time of the index procedure can also be considered in patients with angiographically critical atherosclerotic plaques (high thrombus burden, ulcerated, TIMI flow <3, angiographic stenosis >95%) especially in the left anterior descending artery. MV-PCI at the index procedure may be considered in situations where it is difficult to determine the culprit lesion (for example coexistent left circumflex and right coronary artery critical lesions in patients with inferior wall ACS). In patients who are older, have chronic comorbid conditions such as diabetes or chronic kidney disease, a staged approach for non-culprit lesions may be preferred to prevent acute kidney injury. Timing of the staged procedure is debatable (same admission versus outpatient) and relies on the clinical scenario, ongoing symptoms and patient-physician preference after a risk-benefit discussion. Noninvasive or invasive testing (FFR) may be considered in the non-acute staged setting, as appropriate. Until more data are available, an individualized approach should be adopted after careful evaluation of the lesion severity, hemodynamics, underlying comorbidities, vascular access, physician comfort, and cardiac catheterization laboratory ancillary staff availability (day versus night).
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Khera S, Kolte D, Palaniswamy C, et al. ST-elevation myocardial infarction in the elderly--temporal trends in incidence, utilization of percutaneous coronary intervention and outcomes in the United States. Int J Cardiol 2013;168:3683-90. [Crossref] [PubMed]
- Khera S, Kolte D, Gupta T, et al. Temporal Trends and Sex Differences in Revascularization and Outcomes of ST-Segment Elevation Myocardial Infarction in Younger Adults in the United States. J Am Coll Cardiol 2015;66:1961-72. [Crossref] [PubMed]
- Muller DW, Topol EJ, Ellis SG, et al. Multivessel coronary artery disease: a key predictor of short-term prognosis after reperfusion therapy for acute myocardial infarction. Thrombolysis and Angioplasty in Myocardial Infarction (TAMI) Study Group. Am Heart J 1991;121:1042-9. [Crossref] [PubMed]
- Jaski BE, Cohen JD, Trausch J, et al. Outcome of urgent percutaneous transluminal coronary angioplasty in acute myocardial infarction: comparison of single-vessel versus multivessel coronary artery disease. Am Heart J 1992;124:1427-33. [Crossref] [PubMed]
- Sorajja P, Gersh BJ, Cox DA, et al. Impact of multivessel disease on reperfusion success and clinical outcomes in patients undergoing primary percutaneous coronary intervention for acute myocardial infarction. Eur Heart J 2007;28:1709-16. [Crossref] [PubMed]
- Park DW, Clare RM, Schulte PJ, et al. Extent, location, and clinical significance of non-infarct-related coronary artery disease among patients with ST-elevation myocardial infarction. JAMA 2014;312:2019-27. [Crossref] [PubMed]
- Pundziute G, Schuijf JD, Jukema JW, et al. Evaluation of plaque characteristics in acute coronary syndromes: non-invasive assessment with multi-slice computed tomography and invasive evaluation with intravascular ultrasound radiofrequency data analysis. Eur Heart J 2008;29:2373-81. [Crossref] [PubMed]
- Rodriguez-Granillo GA, McFadden EP, Valgimigli M, et al. Coronary plaque composition of nonculprit lesions, assessed by in vivo intracoronary ultrasound radio frequency data analysis, is related to clinical presentation. Am Heart J 2006;151:1020-24. [Crossref] [PubMed]
- Stone GW, Maehara A, Lansky AJ, et al. A prospective natural-history study of coronary atherosclerosis. N Engl J Med 2011;364:226-35. [Crossref] [PubMed]
- American College of Emergency Physicians. 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction: executive summary: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol 2013;61:485-510. [Crossref] [PubMed]
- Authors/Task Force members, Windecker S, Kolh P, et al. 2014 ESC/EACTS Guidelines on myocardial revascularization: The Task Force on Myocardial Revascularization of the European Society of Cardiology (ESC) and the European Association for Cardio-Thoracic Surgery (EACTS)Developed with the special contribution of the European Association of Percutaneous Cardiovascular Interventions (EAPCI). Eur Heart J 2014;35:2541-619. [Crossref] [PubMed]
- Bauer T, Zeymer U, Hochadel M, et al. Use and outcomes of multivessel percutaneous coronary intervention in patients with acute myocardial infarction complicated by cardiogenic shock (from the EHS-PCI Registry). Am J Cardiol 2012;109:941-6. [Crossref] [PubMed]
- Corpus RA, House JA, Marso SP, et al. Multivessel percutaneous coronary intervention in patients with multivessel disease and acute myocardial infarction. Am Heart J 2004;148:493-500. [Crossref] [PubMed]
- Hannan EL, Samadashvili Z, Walford G, et al. Culprit vessel percutaneous coronary intervention versus multivessel and staged percutaneous coronary intervention for ST-segment elevation myocardial infarction patients with multivessel disease. JACC Cardiovasc Interv 2010;3:22-31. [Crossref] [PubMed]
- Qarawani D, Nahir M, Abboud M, et al. Culprit only versus complete coronary revascularization during primary PCI. Int J Cardiol 2008;123:288-92. [Crossref] [PubMed]
- Rigattieri S, Biondi-Zoccai G, Silvestri P, et al. Management of multivessel coronary disease after ST elevation myocardial infarction treated by primary angioplasty. J Interv Cardiol 2008;21:1-7. [Crossref] [PubMed]
- Toma M, Buller CE, Westerhout CM, et al. Non-culprit coronary artery percutaneous coronary intervention during acute ST-segment elevation myocardial infarction: insights from the APEX-AMI trial. Eur Heart J 2010;31:1701-7. [Crossref] [PubMed]
- Politi L, Sgura F, Rossi R, et al. A randomised trial of target-vessel versus multi-vessel revascularisation in ST-elevation myocardial infarction: major adverse cardiac events during long-term follow-up. Heart 2010;96:662-7. [Crossref] [PubMed]
- Di Mario C, Mara S, Flavio A, et al. Single vs multivessel treatment during primary angioplasty: results of the multicentre randomised HEpacoat for cuLPrit or multivessel stenting for Acute Myocardial Infarction (HELP AMI) Study. Int J Cardiovasc Intervent 2004;6:128-33. [Crossref] [PubMed]
- Hlinomaz O. Multivessel coronary disease diagnosed at the time of primary PCI for STEMI: complete revascularization versus conservative strategy: the PRAGUE 13 trial. Available online: http://sbhci.org.br/wp-content/uploads/2015/05/PRAGUE-13-Trial.pdf
- Wald DS, Morris JK, Wald NJ, et al. Randomized trial of preventive angioplasty in myocardial infarction. N Engl J Med 2013;369:1115-23. [Crossref] [PubMed]
- Engstrøm T, Kelbæk H, Helqvist S, et al. Complete revascularisation versus treatment of the culprit lesion only in patients with ST-segment elevation myocardial infarction and multivessel disease (DANAMI-3—PRIMULTI): an open-label, randomised controlled trial. Lancet 2015;386:665-71. [Crossref] [PubMed]
- Gershlick AH, Khan JN, Kelly DJ, et al. Randomized trial of complete versus lesion-only revascularization in patients undergoing primary percutaneous coronary intervention for STEMI and multivessel disease: the CvLPRIT trial. J Am Coll Cardiol 2015;65:963-72. [Crossref] [PubMed]
- Smits PC, Abdel-Wahab M, Neumann FJ, et al. Fractional Flow Reserve-Guided Multivessel Angioplasty in Myocardial Infarction. N Engl J Med 2017;376:1234-44. [Crossref] [PubMed]
- Politi L, Sgura F, Rossi R, et al. Correction. Heart 2014;100:350. [Crossref]
- Dambrink JH, van’t Hof A. Multivessel revascularisation in ST-elevation myocardial infarction: too early to change the guidelines. Heart 2010;96:1511; author reply 1511-2. [Crossref] [PubMed]
- Mauri L. Nonculprit lesions--innocent or guilty by association. N Engl J Med 2013;369:1166-7. [Crossref] [PubMed]
- Di Mario C, Rosser G. Open questions for non-infarct-related arteries in STEMI. Lancet 2015;386:630-2. [Crossref] [PubMed]
- Banning AS, Gershlick AH. Complete revascularisation in patients with ST-segment elevation myocardial infarction and multivessel disease: contemporary data in context. Evid Based Med 2016;21:73-4. [Crossref] [PubMed]
- Bhatt DL. Do we really know the CvLPRIT in Myocardial infarction? or just stent all lesions? J Am Coll Cardiol 2015;65:973-5. [Crossref] [PubMed]
- Køber L. Complete Revascularization in ST-Elevation Myocardial Infarction? N Engl J Med 2017;376:1282-4. [Crossref] [PubMed]
- Spencer FA, Sekercioglu N, Prasad M, et al. Culprit vessel versus immediate complete revascularization in patients with ST-segment myocardial infarction-a systematic review. Am Heart J 2015;170:1133-9. [Crossref] [PubMed]
- Shah R, Berzingi C, Mumtaz M, et al. Meta-Analysis Comparing Complete Revascularization Versus Infarct-Related Only Strategies for Patients With ST-Segment Elevation Myocardial Infarction and Multivessel Coronary Artery Disease. Am J Cardiol 2016;118:1466-72. [Crossref] [PubMed]
- Fan ZG, Gao XF, Li XB, et al. The optimal strategy of percutaneous coronary intervention for ST-elevation myocardial infarction patients with multivessel disease: an updated meta-analysis of 9 randomized controlled trials. Minerva Cardioangiol 2017;65:148-56. [PubMed]
- Bangalore S, Toklu B, Wetterslev J. Complete versus culprit-only revascularization for ST-segment-elevation myocardial infarction and multivessel disease: a meta-analysis and trial sequential analysis of randomized trials. Circ Cardiovasc Interv 2015;8:e002142. [Crossref] [PubMed]
- El-Hayek GE, Gershlick AH, Hong MK, et al. Meta-Analysis of Randomized Controlled Trials Comparing Multivessel Versus Culprit-Only Revascularization for Patients With ST-Segment Elevation Myocardial Infarction and Multivessel Disease Undergoing Primary Percutaneous Coronary Intervention. Am J Cardiol 2015;115:1481-6. [Crossref] [PubMed]
- Kowalewski M, Schulze V, Berti S, et al. Complete revascularisation in ST-elevation myocardial infarction and multivessel disease: meta-analysis of randomised controlled trials. Heart 2015;101:1309-17. [Crossref] [PubMed]
- Bittl JA, Tamis-Holland JE, Lang CD, et al. Outcomes after multivessel or culprit-Vessel intervention for ST-elevation myocardial infarction in patients with multivessel coronary disease: a Bayesian cross-design meta-analysis. Catheter Cardiovasc Interv 2015;86 Suppl 1:S15-22. [Crossref] [PubMed]
- Bajaj NS, Kalra R, Aggarwal H, et al. Comparison of Approaches to Revascularization in Patients With Multivessel Coronary Artery Disease Presenting With ST-Segment Elevation Myocardial Infarction: Meta-analyses of Randomized Control Trials. J Am Heart Assoc 2015;4:e002540. [Crossref] [PubMed]
- Tarantini G, D'Amico G, Brener SJ, et al. Survival After Varying Revascularization Strategies in Patients With ST-Segment Elevation Myocardial Infarction and Multivessel Coronary Artery Disease: A Pairwise and Network Meta-Analysis. JACC Cardiovasc Interv 2016;9:1765-76. [Crossref] [PubMed]
- Villablanca PA, Briceno DF, Massera D, et al. Culprit-lesion only versus complete multivessel percutaneous intervention in ST-elevation myocardial infarction: A systematic review and meta-analysis of randomized trials. Int J Cardiol 2016;220:251-9. [Crossref] [PubMed]
- Bainey KR, Welsh RC, Toklu B, et al. Complete vs Culprit-Only Percutaneous Coronary Intervention in STEMI With Multivessel Disease: A Meta-analysis and Trial Sequential Analysis of Randomized Trials. Can J Cardiol 2016;32:1542-51. [Crossref] [PubMed]
- Wang CH, Zhang SY, Jin XF. Complete revascularization versus culprit-only revascularization in ST-segment elevation myocardial infarction and multivessel disease patients undergoing primary percutaneous coronary intervention: A meta-analysis and trial sequential analysis. Int J Cardiol 2017;228:844-52. [Crossref] [PubMed]
- Li Z, Zhou Y, Xu Q, et al. Staged versus One-Time Complete Revascularization with Percutaneous Coronary Intervention in STEMI Patients with Multivessel Disease: A Systematic Review and Meta-Analysis. PLoS One 2017;12:e0169406. [Crossref] [PubMed]
- Kornowski R, Mehran R, Dangas G, et al. Prognostic impact of staged versus “one-time” multivessel percutaneous intervention in acute myocardial infarction: analysis from the HORIZONS-AMI (harmonizing outcomes with revascularization and stents in acute myocardial infarction) trial. J Am Coll Cardiol 2011;58:704-11. [Crossref] [PubMed]
- Iqbal MB, Nadra IJ, Ding L, et al. Culprit Vessel Versus Multivessel Versus In-Hospital Staged Intervention for Patients With ST-Segment Elevation Myocardial Infarction and Multivessel Disease: Stratified Analyses in High-Risk Patient Groups and Anatomic Subsets of Nonculprit Disease. JACC Cardiovasc Interv 2017;10:11-23. [Crossref] [PubMed]
- Levine GN, Bates ER, Blankenship JC, et al. 2015 ACC/AHA/SCAI Focused Update on Primary Percutaneous Coronary Intervention for Patients With ST-Elevation Myocardial Infarction: An Update of the 2011 ACCF/AHA/SCAI Guideline for Percutaneous Coronary Intervention and the 2013 ACCF/AHA Guideline for the Management of ST-Elevation Myocardial Infarction. J Am Coll Cardiol 2016;67:1235-50. [Crossref] [PubMed]
- Patel MR, Calhoon JH, Dehmer GJ, et al. ACC/AATS/AHA/ASE/ASNC/SCAI/SCCT/STS 2016 Appropriate Use Criteria for Coronary Revascularization in Patients With Acute Coronary Syndromes: A Report of the American College of Cardiology Appropriate Use Criteria Task Force, American Association for Thoracic Surgery, American Heart Association, American Society of Echocardiography, American Society of Nuclear Cardiology, Society for Cardiovascular Angiography and Interventions, Society of Cardiovascular Computed Tomography, and the Society of Thoracic Surgeons. J Am Coll Cardiol 2017;69:570-91. [Crossref] [PubMed]


