Training and certification in endobronchial ultrasound-guided transbronchial needle aspiration
Introduction
Lung cancer is the most commonly diagnosed cancer worldwide and the most frequent cause of cancer death (1). Most cases are non-small cell lung cancer (NSCLC) and accurate staging of these is crucial for allocation to surgical treatment, which is curative only in cases of localized disease.
The examination of patients suspected of lung cancer is a clinical challenge. The achievement of tissue samples by invasive techniques is of utmost importance, firstly to confirm or invalidate the image based suspicion of cancer and secondly, to determine the Tumour-Node-Metastasis (TNM)-classification if lung cancer is demonstrated. The imaging techniques used are typically computed tomographic (CT) evaluation and positron emission tomography (PET) (2). Among the invasive techniques, endobronchial ultrasound-guided transbronchial needle aspiration (EBUS-TBNA) plays a key role (3).
EBUS-TBNA and EUS-FNA
EBUS-TBNA and oesophageal ultrasound guided fine needle aspiration (EUS-FNA) can be performed in an out-patient setting under local anaesthesia with mild sedation. The two procedures are complementary to each other (4,5). EUS is traditionally performed with the regular EUS endoscope, but the use of the EBUS endoscope in the oesophagus (so called EUS-B) is gaining ground and current evidence suggest it to be a safe method (6,7). Established indications are to obtain a biopsy from a primary lung lesion and/or mediastinal lymph nodes in order to diagnose and stage lung cancer (3) and other diseases for example sarcoidosis (8). Endosonography can help a considerable proportion of patients to avoid surgical staging procedures in the initial evaluation of the mediastinum as it has a similar yield with fewer complications (9,10).
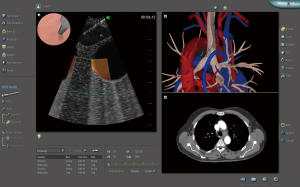
A range of instruments with linear transducers that are suitable for monitoring the needle during biopsy are available. The instrument provides an endoscopic picture and an ultrasonic picture at the same time. The procedure is performed with a dedicated needle assembly consisting of a long steel needle, a sheath, and a handle for manipulation of the needle. The needle assembly is attached to the working channel of the endoscope. When the lesion has been outlined, the needle is advanced under real time ultrasonic guidance.
Simulation-based education in EBUS-TBNA
EBUS-TBNA is a complex clinical procedure with a long learning curve and the success is dependent on the competence of the operator. New trainees in endosonography should follow a structured training curriculum (11) consisting of simulation-based training followed by supervised practice on patients with systematic feedback to become certified in EBUS-TBNA. A general needs assessment in pulmonary medicine (12) showed a huge need for simulation-based education in EBUS-TBNA. Recently, a training programme was developed by the European Respiratory Society (ERS) (13) consisting of three parts: (I) theory; (II) clinical observation and simulation training and (III) supervised training. Each part ends with certification which the trainee has to pass before moving to the next part. At our institution, simulation training can be accessed as a 2-day intensive course or alternatively as primarily self-training sessions distributed over a few weeks at a simulation centre (14). The course consists of four steps: theoretical preparation including a basic handbook on EBUS and EUS, introduction to simulator training, self-training and a validated test. This approach is described in greater detail below.
Introduction to simulation training
Safe handling of the EBUS endoscope and aspiration needle is demonstrated and practiced in great detail using a “dummy-scope” before starting exercises in the simulator. Prior to practicing EBUS procedures on the simulator, a complete bronchoscopy is performed to ensure that the participant knows the anatomy of the bronchial tree and how to handle a conventional bronchoscope. This also allows the participant to be acquainted with the safe use of the simulator. The participant navigates through the bronchial tree and identifies key anatomical positions where the underlying lymph node stations are located.
Thereafter, the insertion of the EBUS endoscope is practiced in the simulator (30-degree oblique angle view). The next step is to turn on the ultrasound transducer and to practice locating the six simple anatomical EBUS landmarks (15). It is easier to remember six EBUS landmarks instead of trying to remember the whole anatomy at once. You can always go back to these landmarks if you lose your way. Six simple landmarks for EUS also exist and are used in the clinical setting. However, EUS modules for simulation training have yet to be developed.
The six EBUS landmarks: pattern recognition
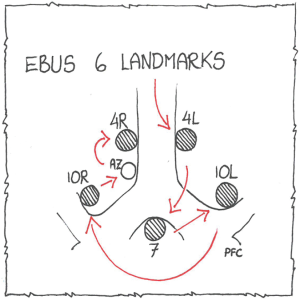
The participant is encouraged to identify the six landmarks systematically in the order mentioned below (Figure 1). This approach ensures that the procedure is done systematically without missing any structures and prepares the participant to the test in the clinical setting, which is done after the education in the simulator using the validated endobronchial ultrasound assessment tool (EBUSAT) (11,16-20).
- Station 4L: the endoscope is turned counter clockwise in the trachea. The lymph node station is found between the arch of the aorta and the left pulmonary artery. The ultrasonographic image showing 4L and the two vessels resembles the ears of Mickey Mouse. The superior margin of the arch of the aorta forms the border between station 2L and 4L;
- Station 7 is found below the carina with the EBUS scope in the right or the left main bronchus facing medially. Carina forms the upper border of this station;
- Station 10L is found when looking upwards with the transducer in the left main bronchus and the left upper lobe bronchus. The superior rim of the left pulmonary artery forms the boundary between station 4L and 10L;
- Station 10R is found when looking upwards with the transducer in the right main bronchus and the right upper lobe bronchus. Station 10R lies caudal to the inferior border of the azygos vein close to the right main bronchus;
- The azygos vein: look for the azygos vein by turning the transducer to the right in the trachea. Note that the azygos vein communicates with the superior vena cava;
- Station 4R: this lymph node is found to the right or in front of trachea above the azygos vein. The inferior border of the azygos vein marks the inferior border of station 4R. The intersection of the caudal margin of the right brachiocephalic vein with the right-sided border of the trachea marks the border between stations 2R and 4R.
The TBNA technique is practiced in a systematic way. The participant learns the correct positioning of the transducer and proper use of the sheath, stylet and the needle. Each lymph node is punctured several times.
Finally, the participant practices on different cases by identifying anatomical landmarks and performing the biopsy procedure (Figure 2).
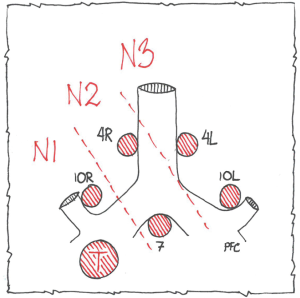
It is important to note that the order mentioned above (station 4L → station 7 → station 10L/11L → station 10R/11R → azygos vein → station 4R) (20) is the initial diagnostic approach to ensure that the procedure is done systematically (Figure 1). When taking biopsies, the order should be from the lymph node with the highest N-value to the lowest, after which the lung tumour is biopsied (N3 → N2 → N1 → lung tumour). This order is used to avoid falsely upstaging the patient to an inoperable stage (Figure 3). It is important for the EBUS operator to be aware of the anatomical orientation and the six landmarks as a patient might be falsely upstaged if, for example, the operator biopsies a malignant N1 lymph node believing it is an N2 lymph node. This mistake would classify the patient as N2 and inoperable.
Self-training sessions
The participant trains on the simulator by following the provided programme and completing different tasks and cases. A training assistant (i.e., a nurse, medical student, or junior doctor) is available for support and technical guidance.
Certification and assessment
The EBUS simulation course at our institution is a part of the ERS structured training programme (13). Part one of the education ends with a theoretical test.
The certification after part two is a practical test in the simulator. It consists of EBUS-TBNA procedures on simulated patient cases. The participant performs complete procedures including introduction of the endoscope, identification of the six anatomical landmarks in the correct order, checking for enlarged lymph nodes, and obtaining biopsies. The performance is assessed and a pass/fail-decision is reached based on two validated assessment tools using simulator metrics and direct observation by an EBUS expert, respectively (20,21).
Part three of the course consists of supervised training at the home institution of the trainee. Final certification consists of clinical videos (13).
Endosonography training and certification requirements are under discussion. The establishment of competence should be based on an objective and valid assessment of all three.
Currently, validity evidence has been gathered for two assessment tools for testing technical EBUS skills and anatomical orientation: the endobronchial ultrasound skills and tasks assessment tool (EBUS-STAT) (22) and the EBUSAT (20). The EBUSAT is the first assessment tool allowing for blinded assessment of clinical performance. It is used in the ERS structured EBUS training programme (13).
Simulation training versus traditional methods
In recent years, there has been increasing focus on patient safety especially in connection with invasive diagnostic procedures including EBUS-TBNA. It has been suggested that 40–50 procedures for initial acquisition of competence should be sufficient (23,24). However, these arbitrary numbers are based on expert opinions. Studies of EBUS learning curves have shown that the performance of 50 procedures does not necessarily ensure basic competency (25).
Simulation-based training has been compared with wet laboratory training and apprenticeship training, respectively (26,27), and were found to be equally effective. In another study physician- versus respiratory therapist-proctored simulation-based training was compared, which also turned out to be equal in effectiveness (28). Furthermore, clinical training has been compared with simulator training and the resulting learning curves were analysed (29). It was found that simulator training lead to rapid acquisition of skills comparable with clinical training. Konge et al. found simulator training to be effective in the beginning of the learning curve for EBUS skills and showed that skills acquired on a simulator can be transferred to a clinical setting (20).
Simulation-based education in the procedure is superior to the traditional apprenticeship model in the beginning of the learning curve (20) and the newest guidelines recommend the use of simulators for training the procedure (3). There are simulators commercially available for EBUS-TBNA, including phantoms and virtual reality. Despite the positive effects of simulation-based education, it is important to remember that no simulator is completely realistic and not all aspects of the procedure can be practiced. Supervised performance during initial patient encounters is essential after the completion of the simulation-based education and test.
The staging of patients with lung cancer by ultrasonic access via both the trachea and oesophagus is superior to staging by a single technique (30). It is therefore logical that the two techniques are learned and performed in combination (31). For practical reasons, the two procedures can be performed with one endoscope (the EBUS endoscope for both EBUS-TBNA and EUS-B-FNA) (4). Currently, solely EBUS simulators for the tracheal access exist, but we hope that simulation-based education of EBUS-TBNA as well as EUS-B-FNA will be possible in the near future.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Ferlay J, Steliarova-Foucher E, Lortet-Tieulent J, et al. Cancer incidence and mortality patterns in Europe: estimates for 40 countries in 2012. Eur J Cancer 2013;49:1374-403. [Crossref] [PubMed]
- Vansteenkiste J, De Ruysscher D, Eberhardt WE, et al. Early and locally advanced non-small-cell lung cancer (NSCLC): ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol 2013;24 Suppl 6:vi89-98. [Crossref] [PubMed]
- Vilmann P, Clementsen PF, Colella S, et al. Combined endobronchial and esophageal endosonography for the diagnosis and staging of lung cancer: European Society of Gastrointestinal Endoscopy (ESGE) Guideline, in cooperation with the European Respiratory Society (ERS) and the European Society of Thoracic Surgeons (ESTS). Endoscopy 2015;47:c1. [Crossref] [PubMed]
- Vilmann P, Clementsen PF. Combined EUS and EBUS are complementary methods in lung cancer staging: Do not forget the esophagus. Endosc Int Open 2015;3:E300-1. [Crossref] [PubMed]
- Dietrich CF, Annema JT, Clementsen P, et al. Ultrasound techniques in the evaluation of the mediastinum, part I: endoscopic ultrasound (EUS), endobronchial ultrasound (EBUS) and transcutaneous mediastinal ultrasound (TMUS), introduction into ultrasound techniques. J Thorac Dis 2015;7:E311-25. [PubMed]
- Kang HJ, Hwangbo B, Lee GK, et al. EBUS-centred versus EUS-centred mediastinal staging in lung cancer: a randomised controlled trial. Thorax 2014;69:261-8. [Crossref] [PubMed]
- Dhooria S, Aggarwal AN, Gupta D, et al. Utility and Safety of Endoscopic Ultrasound With Bronchoscope-Guided Fine-Needle Aspiration in Mediastinal Lymph Node Sampling: Systematic Review and Meta-Analysis. Respir Care 2015;60:1040-50. [Crossref] [PubMed]
- von Bartheld MB, Dekkers OM, Szlubowski A, et al. Endosonography vs conventional bronchoscopy for the diagnosis of sarcoidosis: the GRANULOMA randomized clinical trial. JAMA 2013;309:2457-64. [Crossref] [PubMed]
- Annema JT, van Meerbeeck JP, Rintoul RC, et al. Mediastinoscopy vs endosonography for mediastinal nodal staging of lung cancer: a randomized trial. JAMA 2010;304:2245-52. [Crossref] [PubMed]
- Sehgal IS, Dhooria S, Aggarwal AN, et al. Endosonography Versus Mediastinoscopy in Mediastinal Staging of Lung Cancer: Systematic Review and Meta-Analysis. Ann Thorac Surg 2016;102:1747-55. [Crossref] [PubMed]
- Konge L, Colella S, Vilmann P, et al. How to learn and to perform endoscopic ultrasound and endobronchial ultrasound for lung cancer staging: A structured guide and review. Endosc Ultrasound 2015;4:4-9. [Crossref] [PubMed]
- Nayahangan LJ, Clementsen PF, Paltved C, et al. Identifying Technical Procedures in Pulmonary Medicine That Should Be Integrated in a Simulation-Based Curriculum: A National General Needs Assessment. Respiration 2016;91:517-22. [Crossref] [PubMed]
- Farr A, Clementsen P, Herth F, et al. Endobronchial ultrasound: launch of an ERS structured training programme. Breathe 2016;12:217-20. [Crossref] [PubMed]
- Konge L, Ringsted C, Bjerrum F, et al. The Simulation Centre at Rigshospitalet, Copenhagen, Denmark. J Surg Educ 2015;72:362-5. [Crossref] [PubMed]
- Jenssen C, Annema JT, Clementsen P, et al. Ultrasound techniques in the evaluation of the mediastinum, part 2: mediastinal lymph node anatomy and diagnostic reach of ultrasound techniques, clinical work up of neoplastic and inflammatory mediastinal lymphadenopathy using ultrasound techniques and how to learn mediastinal endosonography. J Thorac Dis 2015;7:E439-58. [PubMed]
- Konge L, Vilmann P, Clementsen P, et al. Reliable and valid assessment of competence in endoscopic ultrasonography and fine-needle aspiration for mediastinal staging of non-small cell lung cancer. Endoscopy 2012;44:928-33. [Crossref] [PubMed]
- Konge L, Annema J, Vilmann P, et al. Transesophageal ultrasonography for lung cancer staging: learning curves of pulmonologists. J Thorac Oncol 2013;8:1402-8. [Crossref] [PubMed]
- Colella S, Vilmann P, Konge L, et al. Endoscopic ultrasound in the diagnosis and staging of lung cancer. Endosc Ultrasound 2014;3:205-12. [Crossref] [PubMed]
- Savran MM, Clementsen PF, Annema JT, et al. Development and validation of a theoretical test in endosonography for pulmonary diseases. Respiration 2014;88:67-73. [Crossref] [PubMed]
- Konge L, Clementsen PF, Ringsted C, et al. Simulator training for endobronchial ultrasound: a randomised controlled trial. Eur Respir J 2015;46:1140-9. [Crossref] [PubMed]
- Konge L, Annema J, Clementsen P, et al. Using virtual-reality simulation to assess performance in endobronchial ultrasound. Respiration 2013;86:59-65. [Crossref] [PubMed]
- Davoudi M, Colt HG, Osann KE, et al. Endobronchial ultrasound skills and tasks assessment tool: assessing the validity evidence for a test of endobronchial ultrasound-guided transbronchial needle aspiration operator skill. Am J Respir Crit Care Med 2012;186:773-9. [Crossref] [PubMed]
- Bolliger CT, Mathur PN, Beamis JF, et al. ERS/ATS statement on interventional pulmonology. European Respiratory Society/American Thoracic Society. Eur Respir J 2002;19:356-73. [PubMed]
- Ernst A, Silvestri GA, Johnstone D, et al. Interventional pulmonary procedures: Guidelines from the American College of Chest Physicians. Chest 2003;123:1693-717. [Crossref] [PubMed]
- Wahidi MM, Silvestri GA, Coakley RD, et al. A prospective multicenter study of competency metrics and educational interventions in the learning of bronchoscopy among new pulmonary fellows. Chest 2010;137:1040-9. [Crossref] [PubMed]
- Stather DR, MacEachern P, Chee A, et al. Wet laboratory versus computer simulation for learning endobronchial ultrasound: a randomized trial. Can Respir J 2012;19:325-30. [Crossref] [PubMed]
- Stather DR, MacEachern P, Chee A, et al. Evaluation of clinical endobronchial ultrasound skills following clinical versus simulation training. Respirology 2012;17:291-9. [Crossref] [PubMed]
- Stather DR, Chee A, Maceachern P, et al. Evaluation of a novel method of teaching endobronchial ultrasound: physician- versus respiratory therapist-proctored simulation training. Can Respir J 2013;20:243-7. [Crossref] [PubMed]
- Stather DR, Maceachern P, Rimmer K, et al. Assessment and learning curve evaluation of endobronchial ultrasound skills following simulation and clinical training. Respirology 2011;16:698-704. [Crossref] [PubMed]
- Zhang R, Ying K, Shi L, et al. Combined endobronchial and endoscopic ultrasound-guided fine needle aspiration for mediastinal lymph node staging of lung cancer: a meta-analysis. Eur J Cancer 2013;49:1860-7. [Crossref] [PubMed]
- Annema JT, Rabe KF. Why respiratory physicians should learn and implement EUS-FNA. Am J Respir Crit Care Med 2007;176:99; author reply 99. [Crossref] [PubMed]