Development of acute parotitis after non-invasive ventilation
Introduction
The parotid gland is the largest of the three major salivary glands. The parotid duct, or Stensen duct, is the main excretory duct of the parotid gland. Saliva produced in the parotid gland flows through the parotid duct and enters the oral cavity in the region of the second maxillary molar (1). Any process disrupting salivary flow through the parotid duct, such as sialolithiasis, stenosis, mass, anatomic anomaly, and certain medications (especially those with anticholinergic activity) can lead to acute parotitis. Often such obstruction can lead to bacterial infection (acute suppurative parotitis), but other etiologies include viral (most commonly mumps), inflammatory (commonly due to obstruction such as stone or duct stricture), and neoplastic (1,2).
Noninvasive ventilation (NIV) is a commonly (and ever increasingly) used therapeutic modality in critical care medicine for the support of patients in acute respiratory failure (3,4). Advantages of NIV include the avoidance of endotracheal intubation and its associated complications. NIV modalities include continuous positive airway pressure (CPAP) and bilevel positive airway pressure (BiPAP). More recently introduced, provision of supplemental oxygen via high-flow nasal cannula (HFNC) may in some circumstances offer an alternative to NIV (5,6).
We herein describe a critically-ill patient developing acute, unilateral parotitis temporally related to BiPAP therapy for acute respiratory failure. Although the association of acute parotitis with NIV has rarely been reported (7-10), the escalating use of these modalities may promote an increased incidence of this entity. Thus, intensivists, pulmonologists and other physicians treating patients with acute respiratory failure should be familiar with this possible complication.
Case presentation
A 90-year-old woman with a 6-week history of diarrhea presented to the emergency department complaining of worsening abdominal pain and onset of bloody diarrhea and hematochezia. Past medical history included hypertension, dyslipidemia, carotid artery stenosis, coronary artery disease with coronary artery bypass grafting 19 years previously, distant total left hip replacement and cholecystectomy, and left breast cancer with lumpectomy 5 months before admission.
On examination she was in discomfort due to pain, hemodynamically stable, with diffuse abdominal tenderness with rebound tenderness. Initial evaluation was significant for elevated white blood cell count (19.8 k/µL) and serum lactic acid (4.7 mmol/L). Abdominal computed tomographic (CT) angiography demonstrated occlusion of the proximal superior mesenteric artery with distal reconstitution and high-grade stenosis of the celiac artery origin with post-stenotic dilatation and diverticulosis.
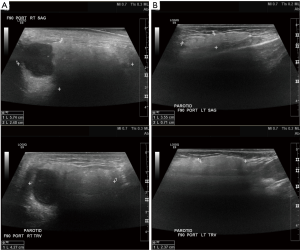
Given suspicion of mesenteric ischemia, the patient underwent prompt laparoscopic exploratory laparotomy that revealed absence of bowel inflammation or ischemia. Postoperative hypoxemia necessitated the initiation of NIV with BiPAP via oronasal mask. After approximately 8 hours of BiPAP therapy, on the morning of the second postoperative day, she developed a sudden swelling and tenderness of the right parotid gland, with erythema and warmth of the overlying skin. On examination by an otolaryngologist, no purulent material was expressed on parotid duct massage. Additional evaluation revealed a normal serum amylase level (77 U/L), decreasing leukocytosis, mumps ELISA was IgG (+). Ultrasound of the parotids demonstrated an enlarged right parotid gland (Figure 1) as well as bilateral hypoechoic lesions that most likely represent benign adenomas (11). Previously initiated broad spectrum antibiotics (piperacillin-tazobactam, vancomycin, and metronidazole) were continued, BiPAP was discontinued, and respiratory assistance was provided by HFNC. Supportive care included parotid gland massages, warm compresses and sialogogues. Swelling began to decrease after two days and had fully resolved by six days after initial onset.
Discussion
Given the temporal relation of the initiation of BiPAP to the development of acute unilateral parotitis, and its resolution subsequent to discontinuation of this NIV mode, administration of BiPAP appears to be the underlying etiology of acute parotitis in our patient. Four previous patients have been described as developing acute parotitis associated with NIV (7-10), including one treated with CPAP (8). Our case appears to report the shortest duration (8 hours) of NIV prior to the development of acute parotitis. It is of interest to note that, excluding the lone case reporting a patient receiving CPAP (8), who was young (36 years) and developed bilateral parotitis, the other three previously-published cases (7,9,10), as well as the patient reported herein, received NIV (not CPAP mode), were all elderly (age range, 82–90 years), and developed unilateral parotitis on the right side. Additional reports of this entity will be necessary to discern whether there is indeed a predilection for acute parotitis associated with NIV to occur preferentially on the right side, or whether this is simply a coincidence among a small sample size.
The development of acute parotitis due to NIV likely involves positive airway pressure transmitted to the oral cavity causing retrograde air flow and obstruction of the parotid (Stensen) duct (8,9). The initial report of this phenomenon (7) suggested compression of the external parotid duct by the oronasal mask used to deliver NIV, but this seems unlikely as subsequent reports described patients receiving NIV via total face mask as well as via oronasal mask.
Certain features of our patient may have predisposed her to develop acute, unilateral parotitis from exposure to positive airway pressure delivered by BiPAP mask. Advanced age, a state of dehydration, and absence of salivary gland stimulation due to restriction of oral intake can all contribute to increased salivary viscosity and salivary stasis (2,9), thus potentiating the local effect of NIV.
Numerous drugs have been suggested as associated with the development of acute parotitis, however a recent critical review of this topic (12) concluded that only three drugs, l-asparaginase, clozapine, and phenylbutazone have sufficient evidence to conclude a causal relationship. The patient reported herein had received none of these medications, but did undergo CT angiography on the day of admission. Administration of iodinated contrast dye has been associated with acute parotitis (“iodide mumps”), however this rare entity is typically bilateral (1,13). Our patient also underwent a laparoscopic exploratory laparotomy. General anesthesia has long been identified as a rare cause of acute parotitis (“anesthesia mumps”). This entity is typically bilateral (14,15), but has also been reported as a unilateral occurrence (16).
In summary, NIV may be causally linked to the development of acute parotitis, likely due to transmission of positive pressure to the oral cavity causing obstruction of salivary flow through the parotid duct. As the use of NIV for the treatment of acute respiratory failure will undoubtedly increase going forward, clinicians must be cognizant of this possible complication.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Informed consent was obtained from the patient's son for publication of this case report and any accompanying images.
References
- Hernandez S, Busso C, Walvekar RR. Parotitis and Sialendoscopy of the Parotid Gland. Otolaryngol Clin North Am 2016;49:381-93. [Crossref] [PubMed]
- Wilson KF, Meier JD, Ward PD. Salivary gland disorders. Am Fam Physician 2014;89:882-8. [PubMed]
- Bello G, De Pascale G, Antonelli M. Noninvasive Ventilation. Clin Chest Med 2016;37:711-21. [Crossref] [PubMed]
- Ozsancak Ugurlu A, Sidhom SS, Khodabandeh A, et al. Where is Noninvasive Ventilation Actually Delivered for Acute Respiratory Failure? Lung 2015;193:779-88. [Crossref] [PubMed]
- Mauri T, Turrini C, Eronia N, et al. Physiologic Effects of High-Flow Nasal Cannula in Acute Hypoxemic Respiratory Failure. Am J Respir Crit Care Med 2017;195:1207-15. [Crossref] [PubMed]
- Maury E, Alves M, Bigé N. High-flow nasal cannula oxygen therapy: more than a higher amount of oxygen delivery. J Thorac Dis 2016;8:E1296-E1300. [Crossref] [PubMed]
- Mottard N, Cour M, Chambonnet C, et al. Parotiditis secondary to NIV interface. Intensive Care Med 2014;40:1023-4. [Crossref] [PubMed]
- Abdullayev R, Saral FC, Kucukebe OB, et al. Rev Bras Anestesiol 2016;66:661-3. [Bilateral parotitis in a patient under continuous positive airway pressure treatment]. [Crossref] [PubMed]
- Alaya S, Mofredj A, Tassaioust K, et al. Acute Parotitis as a Complication of Noninvasive Ventilation. J Intensive Care Med 2016;31:561-3. [Crossref] [PubMed]
- Benito Bernáldez C, Romero Muñoz C, Rodríguez Martín PJ. Parotitis in a patient with non-invasive mechanical ventilation. Med Clin (Barc) 2017. [Epub ahead of print].
- Zajkowski P, Ochal-Choińska A. Standards for the assessment of salivary glands - an update. J Ultrason 2016;16:175-90. [Crossref] [PubMed]
- Brooks KG, Thompson DF. A review and assessment of drug-induced parotitis. Ann Pharmacother 2012;46:1688-99. [Crossref] [PubMed]
- Kohat AK, Jayantee K, Phadke RV, et al. Beware of parotitis induced by iodine-containing contrast media. J Postgrad Med 2014;60:75-6. [Crossref] [PubMed]
- Reilly DJ. Benign transient swelling of the parotid glands following general anesthesia: “anesthesia mumps Anesth Analg 1970;49:560-3. [Crossref] [PubMed]
- Jafra A, Arora S, Dwivedi D. Benign swelling of submandibular glands under general anesthesia "anesthesia mumps". J Clin Anesth 2016;34:325-6. [Crossref] [PubMed]
- Kwon SY, Kang YJ, Seo KH, et al. Acute unilateral anesthesia mumps after hysteroscopic surgery under general anesthesia: a case report. Korean J Anesthesiol 2015;68:300-3. [Crossref] [PubMed]


