Successful removal of embolized chemoport catheter within the heart and pericardium: 3 case reports
Introduction
Central venous access devices are routinely used in patients with cancer for infusing medications, delivering chemotherapy agents and parenteral nutrition. The first reported case of embolized foreign bodies, including catheters, ports, instruments, and devices, was in 1954 (1-4). Intracardiac and pericardial foreign bodies are rare complications, however the immediate removal of the foreign bodies is required because of associated complications such as infection, extrusion, extravasation, thrombosis, and even death if the foreign body migrates into the heart (5,6). Herein, we describe three patients for whom we successfully removed embolized chemoport catheters from the heart and pericardium using fluoroscopy and pericardiotomy.
Case description
Case 1
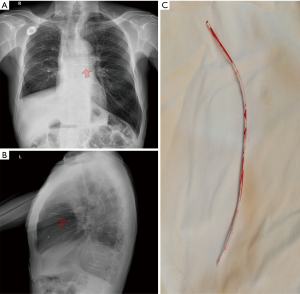
A 66-year-old male patient had been diagnosed with non-small cell lung cancer (NSCLC) in 2004. The NSCLC recurred in November 2011. A vascular access chemoport catheter was surgically inserted via the right internal jugular vein for administration of chemotherapeutic drugs and nutritional support. The catheter had remained in position without any complications for one year followed up. After the 1-year routine follow-up, the patient reported headaches to his oncologist. A chest X-ray was performed for evaluation, revealing that the chemoport catheter had torn and the tube was in the pulmonary trunk (Figure 1). The patient was transferred to the catheterization laboratory, and the fragmented catheter was easily removed using a goose-neck snare technique (AMPLATZ, 4.0 Fr, EV3 Inc., 4600 Nathan Lane, North Plymouth, MN, USA) under fluoroscopy without complications.
Case 2
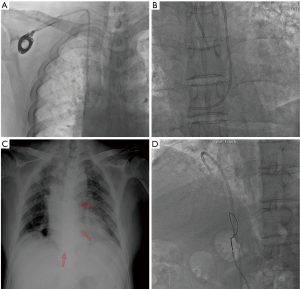
A 68-year-old male patient had been diagnosed with NSCLC in 2011, and then received chemotherapy and radiotherapy for 4 years. A chemoport catheter was implanted below the right clavicle with catheter access into the right internal jugular vein in January 2015. After 2 months, removal of the chemoport was recommended because of an infectious spondylodiscitis diagnosis. Unfortunately, during the removal procedure, there was abnormal resistance to retrieval. The proximal portion fractured and the distal part was embolized. Chest radiography showed that the intra-cardiac fragmented chemoport catheter lay in the right atrium to the left of the pulmonary artery trunk (Figure 2). It was removed with the goose-neck snare technique using an interventional endovascular procedure under fluoroscopy in the right femoral vein with no complications.
Case 3
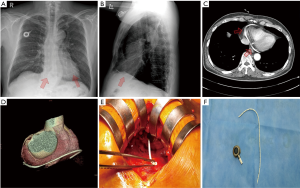
A 70-year-old male patient undergoing a scheduled arthroscopic meniscectomy was transferred to the cardiology department. He had undergone a Miles’ procedure for rectal cancer, followed by chemotherapy, 8 years prior. A chemoport was implanted below the right clavicle with catheter access into the right jugular vein at that time. After 3 months of chemotherapy, he stopped due to weight gain. Since then, he had been told by the hospital staff that he was cancer-free and he had been getting along without any discomfort. He had visited another hospital 1 year prior complaining of chest pain, and received percutaneous coronary intervention to the proximal left anterior descending artery. At this time, a chest X-ray was performed for preoperative evaluation. It showed that a foreign body, thought to be a chemoport catheter, was situated in the inferior border of heart (Figure 3). A percutaneous intracatheter removal procedure was attempted, but it could not be removed. Subsequently, chest computed tomography (CT), echocardiography, and 3D cardiac CT were performed and revealed a fragmented chemoport catheter in the pericardial space. The 3D cardiac CT showed the position and length of the fragmented catheter in the pericardium more definitively (Figure 3). The patient was transferred to the thoracic surgery department for surgical removal of the fractured catheter. There was no pericardial adhesion to the embolized catheter, and it was removed through elective subxiphoid pericardiotomy without any complications (Figure 3).
Discussion
The increasing use of central and peripheral access devices is associated with various types of complications. However, catheter transaction with subsequent embolization is a rare complication (7,8). The causes of catheter fracture and embolization include improper connection, distortion or angulation of the anastomosis site, malposition, fatigue of the catheter, and the compression of the catheter between the clavicle and the first rib (“pinch-off”) (9). To prevent such fractures, the port catheter should be implanted more laterally to the mid-clavicular line, or in some patients, using the jugular vein (10). Fracture and/or migration of a chemoport catheter show a variety of clinical manifestations, including chest discomfort, cough, dyspnea, and palpitations (11). Additionally intra-vascular embolization of port catheters may go undetected for prolonged periods of time because it can be asymptomatic and consequently, it is often diagnosed incidentally. However, embolized catheter fragments can induce serious cardiovascular, pulmonary, and infectious complications (3).
Since the first case reported by Turner et al. in 1954, many more embolized catheter cases have been reported (1-4). Before the first report of percutaneous retrieval of a foreign body in 1964, surgery was the only way to remove an intra- or extra-vascular foreign body using procedures such as thoracotomy or arteriotomy. Since 1964, many studies have reported non-surgical methods, such as loop snare, grasping forcep, deflecting wire, pincher device, and retrieval basket. Percutaneous retrieval of intra-vascular foreign bodies using wire snares has been the preferred method as it is a safe, simple, and effective procedure in most patients. Snare techniques have high success rates and a low complication rate (11,12). The nitinol goose-neck snare has a right angle design. These days, the Amplatz goose-neck snare is the first choice for retrieval of foreign bodies because the right angle provides easy capture of foreign bodies (13,14).
In our first 2 patients, the fractured catheter was removed easily using the goose-neck snare catheter technique. To use this technique, the free end of the foreign body must be accessible. In our patients, the free end of the catheter was in the right atrium, and we successfully entrapped the catheter fragment in the right atrium. In our last patient, however, we attempted percutaneous intracatheter removal procedure under fluoroscopy, but failed because of inaccessibility of the catheter which was situated in the pericardial space. There have been no previous reports of intra-vascular catheters situated in the pericardial space. Just how the chemoport catheter managed to migrate and sit in the pericardial space without any patient symptoms or signs, such as dyspnea or tamponade, is unclear. One possible conjecture is that the tip of the chemoport may have migrated into the pericardial space through the transverse sinus of the supra vena cava covering the pericardium or may have slowly moved through the oracle of the right atrium.
It is important to remember that it is difficult to accurately estimate the position of a foreign body with a simple chest X-ray. The transthoracic echocardiography, chest CT, and 3D cardiac CT were helpful to evaluate the definite position and length of the fragmented foreign body.
According to various reports, the success rate of non-surgical percutaneous foreign body removal is relatively high at about 90%, and the incidence of complications is relatively low (15). Therefore, percutaneous intracatheter removal should be considered for intra-vascular foreign bodies. However, prior to the procedure, various methods should be used to evaluate the exact size and position of the foreign body so as not to perform unnecessary procedures.
Embolized catheter fragments can induce serious complications, and surgical removal should be considered if there are no symptoms, or if percutaneous intracatheter removal is not possible. Above all, the catheters should be routinely removed when treatment is finished in order to avoid this complication, or a routine chest X-ray should be performed early in order to detect complications.
In conclusion, the percutaneous intracatheter procedure is a very useful method for removal of intra- or extra-vascular foreign bodies. Furthermore, periodic evaluation of the intra-vascular catheter is important for the early detection of an embolized catheter. This provides a good opportunity to safely remove foreign bodies and prevent subsequent complications. Evaluation of the exact position and size of the foreign body should be carried out prior to non-surgical or surgical procedures.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent were obtained from the patients for publication of this manuscript and any accompanying images.
References
- Turner DD, Sommers SC. Accidental passage of a polyethylenecatheter from cubital vein to right atrium; report of a fatal case. N Engl J Med 1954;251:744-5. [Crossref] [PubMed]
- Bernhardt LC, Wegner GP, Mendenhall JT. Intravenous catheter embolization to the pulmonary artery. Chest 1970;57:329-32. [Crossref] [PubMed]
- Surov A, Wienke A, Carter JM, et al. Intravascular embolization of venous cathetercauses, clinical signs, and management: a systematic review. JPEN J Parenter Enteral Nutr 2009;33:677-85. [Crossref] [PubMed]
- Mitsopoulos G, Hanna RF, Brejt SZ, et al. Retrieval of a Dislodged Catheter Using Combined Fluoroscopy and intracardiac Echocardiography. Case Rep Radiol 2015;2015:610362. [Crossref] [PubMed]
- McGee DC, Gould MK. Preventing Complications of Central Venous Catheterization. N Engl J Med 2003;348:1123-33. [Crossref] [PubMed]
- Ballarini C, Intra M, Pisani Ceretti A, et al. Complications of subcutaneous infusion port in the general oncology population. Oncology 1999;56:97-102. [Crossref] [PubMed]
- Rauthe G, Altmann C. Complications in connection with venous port systems: prevention and therapy. Eur J Surg Oncol 1998;24:192-9. [Crossref] [PubMed]
- Yildizeli B, Laçin T, Baltacioğlu F, et al. Approach to fragmented central venous catheters. Vascular 2005;13:120-3. [Crossref] [PubMed]
- Aitken DR, Minton JP. The “pinch-off sign”: a warning of impending problems with permanent subclavian catheters. Am J Surg 1984;148:633-6. [Crossref] [PubMed]
- Surov A, Jordan K, Buerke M, et al. Atypical pulmonary embolism of port catheter frag¬ments in oncology patients. Support Care Cancer 2006;14:479-83. [Crossref] [PubMed]
- Cheng CC, Tsai TN, Yang CC, et al. Percutaneousretrieval of dislodged totally implantable central venousaccess system in 92 cases: experience in a single hospital. Eur J Radiol 2009;69:346-50. [Crossref] [PubMed]
- Savader SJ, Brodkin J, Osterman FA Jr. In-situ formation of a loop snare for retrieval of a foreign body without a free end. Cardiovasc Intervent Radiol 1996;19:298-301. [Crossref] [PubMed]
- Cekirge S, Weiss JP, Foster RG, et al. Percutaneous retrieval of foreign bodies: experience with the nitinol Goose Neck snare. J Vasc Interv Radiol 1993;4:805-10. [Crossref] [PubMed]
- Park JH, Yoon DY, Han JK, et al. Retrieval of intravascular foreign bodies with the snare and catheter capture technique. J Vasc Interv Radiol 1992;3:581-2. [Crossref] [PubMed]
- Dondelinger RF, Lepoutre B, Kurdziel JC. Percutaneous vascular foreign body retrieval: experience of an 11-yearperiod. Eur J Radiol 1991;12:4-10. [Crossref] [PubMed]


