Transcatheter aortic valve implantation with the repositionable and fully retrievable Lotus Valve SystemTM
Introduction
Transcatheter aortic valve implantation (TAVI) has become a therapeutic alternative for patients presenting with severe symptomatic aortic stenosis and considered either at high (1,2) or intermediate preoperative risk (3,4) for surgical aortic valve replacement (SAVR). Recent recommendations found that transfemoral TAVI, in comparison to SAVR, results in lower mortality and acute kidney injury at 2 years, and may reduce stroke rates (5). Over the past 15 years, several transcatheter devices have been tested and evolved to decrease access site complications with smaller profile delivery systems, decrease pacemaker rates, and avoid the risk of coronary obstruction and significant paravalvular leakage (PVL) (6-9).
The Lotus Valve System (Boston Scientific Corporation, Natick, MA, USA) consists of a braided nitinol wire frame with three bovine pericardial leaflets mounted on a pre-shaped delivery catheter (10). The valve is deployed via controlled mechanical expansion, which enables predictable and precise placement. The lower half of the Lotus ValveTM is surrounded by an adaptive seal, a polymer membrane designed to fill the space between the native annulus and the prosthetic valve frame, thereby reducing PVL (10). The Lotus Valve function can be assessed in the fully expanded position prior to release. Partial or full recapturing/repositioning of the valve, or full retrieval, is possible at any point prior to uncoupling and release (10).
In this editorial, we refer to the RESPOND (Repositionable Lotus Valve System-Post-Market Evaluation of Real World Clinical Outcomes) study recently published in the European Heart Journal. Falk and colleagues (11) report the results of a prospective, open-label, single-arm, multi-centre, post-market registry, to confirm the safety and efficacy of the Lotus ValveTM in a larger “all-comers” population at 30-day and 1-year follow-up.
Main findings
Study population, 30-day mortality and stroke
A total of 996 patients were included. The mean age was 80.8±6.5 years, 51% were female, with a mean predicted operative mortality risk of 6.0±6.9% and 8.0±8.4% as assessed by the Society of Thoracic Surgeons score and logistic EuroSCORE-II, respectively. Clinical end-points were reported upon the Valve Academic Research Consortium (VARC)-2 definitions (12). The device was successfully implanted in 98.1% of the 1,016 intention-to-treat population. Among these 996 as-treated patients, 99.7% had correct positioning of one valve in the proper anatomical location. Repositioning of the valve was attempted in 29.2%, and was successful (i.e., partial or complete re-sheathing of the Lotus ValveTM in the catheter and redeployment in a more accurate position within the aortic valve annulus) in 99%. The length of hospital stay was 7.3±5.9 days. The 30-day all-cause mortality was 2.6% and 2.2% in the intention-to-treat and as-treated populations, respectively. The overall 30-day stroke rate was 3%, and 2.2% was considered disabling stroke. Strokes were judged not related to repositioning of the valve.
Acute valve performance and paravalvular sealing
Post TAVI, a significantly decrease in mean aortic valve gradient (from 37.7±15.2 mmHg at baseline to 10.8±4.6 mmHg at discharge) and increase in effective orifice aortic valve area (from 0.7±0.2 cm2 at baseline to 1.8±0.4 cm2 at discharge) was observed. Importantly, PVL was absent or trace in 92% of patients, 7.7% of patients showed mild PVL, 0.3% of patients moderate PVL and none presented with severe PVL. The Lotus ValveTM device seals the aortic annulus adjusting to the patient’s anatomy with the mechanically expandable frame, and these results are equivalent or compare favorably to recent reports using different second-generation TAV devices (6,8,9,13,14). The results of the REPRISE II (Repositionable Percutaneous Replacement of Stenotic Aortic Valve through Implantation of Lotus Valve System Evaluation of Safety and Performance) Study Extended Cohort (15) showed that the independent predictors of mild/moderate PVL included the ratio of device area to annulus area, left ventricular outflow tract (LVOT) calcium volume, and annulus area. Interestingly, the rates of mild/moderate PVL were 17.5%, 2.9%, and 3.2%, with 0–5%, 5–10%, and >10% annular oversizing by area, respectively, suggesting therefore that optimal valve oversizing to minimize PVL is >5% by area.
Need for permanent pacemaker implantation (PPI)
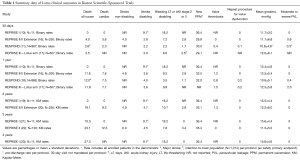
PPI was required in 34.6% of cases who did not have a pacemaker at baseline. This result is not surprising since studies with Lotus ValveTM have consistently reported high (30–36%) rates of PPI (Table 1). In the United Kingdom Experience (24), the incidence of new left bundle brunch block was 55% and 32% of the patients required PPI after Lotus ValveTM implantation (24). These rates are higher than those reported in studies with the self-expanding Accurate TA (8) and Acurate Neo (9) devices (Symetis, S.A., Ecublens, Switzerland/Boston Scientific, Marlborough, MA, USA) that is 5–10% and CoreValve (Medtronic, Inc., Minneapolis, Minnesota, USA), that is 15–26% (2,4,25-27). The Lotus ValveTM is shorter than the CoreValve prosthesis; therefore, one might expect a lower frequency of conduction disorders. However, to anchor the prosthesis within the aortic annulus, the inflow portion of the Lotus ValveTM protrudes into the LVOT thereby damaging the conduction system (28). Notably, an implantation depth of ≤6 mm was associated with a lower incidence of PPI compared with deeper implants with CoreValve (29); however, the UK experience with the Lotus ValveTM showed a mean implantation depth of 5.7±3.2 mm in the overall cohort. Hence, implantation depth was not found a predictor of PPI (24). Based on its mechanically expansion, the radial force of this device may be greater than the CoreValveTM. Importantly, the issue of requiring PPI after TAVI is of concern since it has been shown to be an independent predictor of long-term mortality (30). Moreover, since TAVI is nowadays being performed in intermediate and lower risks patients, hence, younger subjects exhibiting a longer life spam, PPI may predispose to pacing-induced cardiomyopathy. Long-term clinical outcomes as well as valve durability (31) are therefore needed with this device. Table 1 summarizes data on clinical outcomes in Boston Scientific-sponsored trials using the Lotus ValveTM.
Full table
Potential utilities of the Lotus ValveTM beyond the treatment of native aortic stenosis
The safety and feasibility of TAVI for the treatment of non-calcified pure aortic valve regurgitation has been previously reported (32,33). Certainly, the absence of aortic valve and/or annulus calcification to anchor the newly implanted bioprosthesis may contribute to valve malposition or migration needing a second valve (32,33). The use of a repositionable and completely retrievable Lotus ValveTM system permits a well-controlled and safe procedure, thus, it may provide advantages over the first-generation devices in cases of pure aortic regurgitation and/or absence of calcium (34). Data on TAVI in bicuspid aortic valve stenosis is still limited, with significant rates of post-procedural moderate-to-severe PVL (35). In these cases, the mechanically deployed Lotus ValveTM may also provide a valuable alternative (36). Finally, the Lotus ValveTM may also be an option for transcatheter valve-in-valve treatment of failed surgical bioprosthesis (37). Such speculations would nevertheless be off-label use of the Lotus ValveTM device.
Future perspectives for the device
The RESPOND study was conducted using the first-generation “classic” Lotus ValveTM, which is no longer available on the market. The valve that is currently on the market in Europe is the Lotus EdgeTM valve system, which incorporates new design features such as Depth GuardTM technology, designed to reduce LVOT interaction, minimizing the depth of the valve during deployment, a simplified locking mechanism, and a more flexible delivery catheter. The Depth GuardTM feature and increased catheter flexibility were intended to reduce the higher rates of PPI seen with classic Lotus device. Two small studies were conducted to evaluate these features: the RESPOND Extension and the Lotus Edge Feasibility Study. Preliminary (unpublished) data from both studies show a significant reduction in PPI rates (data from Boston Scientific).
Conclusions
TAVI with the repositionable, fully retrievably and mechanically deployed Lotus Valve system is safe, achieving optimal annular sealing with a remarkably low incidence of residual paravalvular aortic regurgitation, but at a cost of increased PPI rate. Future studies will help RESPOND the question around the need for PPI with this device.
Acknowledgements
The authors want to specially thank Vicki M. Houle, PhD and Ms Tamara Blair, from Boston Scientific Corporation, for the help in manuscript proofreading.
Footnote
Conflicts of Interest: Dr. Bagur has received speaking and consulting fees from Boston Scientific. Dr. Choudhury and Dr. Mamas have no conflicts of interest to declare.
References
- Smith CR, Leon MB, Mack MJ, et al. Transcatheter versus surgical aortic-valve replacement in high-risk patients. N Engl J Med 2011;364:2187-98. [Crossref] [PubMed]
- Adams DH, Popma JJ, Reardon MJ, et al. Transcatheter aortic-valve replacement with a self-expanding prosthesis. N Engl J Med 2014;370:1790-8. [Crossref] [PubMed]
- Leon MB, Smith CR, Mack MJ, et al. Transcatheter or Surgical Aortic-Valve Replacement in Intermediate-Risk Patients. N Engl J Med 2016;374:1609-20. [Crossref] [PubMed]
- Reardon MJ, Van Mieghem NM, Popma JJ, et al. Surgical or Transcatheter Aortic-Valve Replacement in Intermediate-Risk Patients. N Engl J Med 2017;376:1321-31. [Crossref] [PubMed]
- Vandvik PO, Otto CM, Siemieniuk RA, et al. Transcatheter or surgical aortic valve replacement for patients with severe, symptomatic, aortic stenosis at low to intermediate surgical risk: a clinical practice guideline. BMJ 2016;354:i5085. [Crossref] [PubMed]
- Thourani VH, Kodali S, Makkar RR, et al. Transcatheter aortic valve replacement versus surgical valve replacement in intermediate-risk patients: a propensity score analysis. Lancet 2016;387:2218-25. [Crossref] [PubMed]
- Bagur R, Kiaii B, Teefy PJ, et al. First North American Experience With the Engager Self-Expanding Transcatheter Aortic Valve: Insights From the London Health Sciences Centre Heart Team. Ann Thorac Surg 2016;102:e167-71. [Crossref] [PubMed]
- Chu MW, Bagur R, Losenno KL, et al. Early clinical outcomes of a novel self-expanding transapical transcatheter aortic valve bioprosthesis. J Thorac Cardiovasc Surg 2017;153:810-8. [Crossref] [PubMed]
- Bagur R, Teefy PJ, Kiaii B, et al. First North American experience with the transfemoral ACURATE-neoTM self-expanding transcatheter aortic bioprosthesis. Catheter Cardiovasc Interv 2017;90:130-8. [Crossref] [PubMed]
- Meredith IT, Worthley SG, Whitbourn RJ, et al. Transfemoral aortic valve replacement with the repositionable Lotus Valve System in high surgical risk patients: the REPRISE I study. EuroIntervention 2014;9:1264-70. [Crossref] [PubMed]
- Falk V, Wohrle J, Hildick-Smith D, et al. Safety and efficacy of a repositionable and fully retrievable aortic valve used in routine clinical practice: the RESPOND Study. Eur Heart J 2017. [Epub ahead of print]. [Crossref] [PubMed]
- Kappetein AP, Head SJ, Genereux P, et al. Updated standardized endpoint definitions for transcatheter aortic valve implantation: the Valve Academic Research Consortium-2 consensus document. J Am Coll Cardiol 2012;60:1438-54. [Crossref] [PubMed]
- Gooley RP, Talman AH, Cameron JD, et al. Comparison of Self-Expanding and Mechanically Expanded Transcatheter Aortic Valve Prostheses. JACC Cardiovasc Interv 2015;8:962-71. [Crossref] [PubMed]
- Manoharan G, Walton AS, Brecker SJ, et al. Treatment of Symptomatic Severe Aortic Stenosis With a Novel Resheathable Supra-Annular Self-Expanding Transcatheter Aortic Valve System. JACC Cardiovasc Interv 2015;8:1359-67. [Crossref] [PubMed]
- Blackman DJ, Meredith IT, Dumonteil N, et al. Predictors of Paravalvular Regurgitation After Implantation of the Fully Repositionable and Retrievable Lotus Transcatheter Aortic Valve (from the REPRISE II Trial Extended Cohort). Am J Cardiol 2017;120:292-9. [Crossref] [PubMed]
- Meredith IT, Dumonteil N, Blackman DJ, et al. Repositionable Percutaneous Aortic Valve Implantation with the Lotus Valve: 30-Day and 1-Year Outcomes in 250 High-Risk Surgical Patients. EuroIntervention 2017. [Epub ahead of print]. [PubMed]
- Feldman TE. A prospective, randomized investigation of a novel transcatheter aortic valve implantation system: the REPRISE III trial. EuroPCR 2017. Paris, France, May 16-19, 2017.
- Van Mieghem NM. The RESPOND study at 1-year: primary endpoint outcomes with a repositionable and fully retrievable aortic valve in routine clinical practice. EuroPCR Presentation 2017. Paris, France, May 16-19, 2017.
- Meredith IT. First report of two-year outcomes with the repositionable Lotus™ Aortic Valve Replacement System: Results from the REPRISE I Feasibility Study. Transcatheter and Cardiovascular Therapeutics 2014. Washington, DC, USA, September 13, 2014.
- Meredith IT. Two-year outcomes with a fully repositionable and retrievable percutaneous aortic valve in 250 high surgical risk patients: Results from the REPRISE II trial extended cohort. PCR London Valves 2016. London, UK, September 19, 2016.
- Meredith IT, Worthley SG, Whitbourn RJ, et al. First report of 3-year outcomes with the repositionable and fully retrievable Lotus Aortic Valve Replacement System: Results from the REPRISE I Feasibility Study. Transcatheter and Cardiovascular Therapeutics 2015. San Francisco, CA, USA, October 13, 2015.
- Meredith IT. Three-year outcomes with the fully repositionable and retrievable Lotus Transcatheter Aortic Replacement Valve in 120 high-risk surgical patients with severe aortic stenosis: Results from the REPRISE II CE-Mark study. Transcatheter and Cardiovascular Therapeutics 2016. Washington, DC, USA, October 31, 2016.
- Meredith IT, Stephen W, Robert W, et al. Four-year clinical outcomes following TAVR with the repositionable and fully retrievable Lotus Valve System: an update from the REPRISE I study. Transcatheter and Cardiovascular Therapeutics 2016. Washington, DC, USA, October 31, 2016.
- Rampat R, Khawaja MZ, Hilling-Smith R, et al. Conduction Abnormalities and Permanent Pacemaker Implantation After Transcatheter Aortic Valve Replacement Using the Repositionable LOTUS Device: The United Kingdom Experience. JACC Cardiovasc Interv 2017;10:1247-53. [Crossref] [PubMed]
- Tamburino C, Capodanno D, Ramondo A, et al. Incidence and predictors of early and late mortality after transcatheter aortic valve implantation in 663 patients with severe aortic stenosis. Circulation 2011;123:299-308. [Crossref] [PubMed]
- Moat NE, Ludman P, de Belder MA, et al. Long-term outcomes after transcatheter aortic valve implantation in high-risk patients with severe aortic stenosis: the U.K. TAVI (United Kingdom Transcatheter Aortic Valve Implantation) Registry. J Am Coll Cardiol 2011;58:2130-8. [Crossref] [PubMed]
- Bagur R, Kwok CS, Nombela-Franco L, et al. Transcatheter Aortic Valve Implantation With or Without Preimplantation Balloon Aortic Valvuloplasty: A Systematic Review and Meta-Analysis. J Am Heart Assoc 2016;5:e003191. [Crossref] [PubMed]
- Bagur R, Rodes-Cabau J, Gurvitch R, et al. Need for permanent pacemaker as a complication of transcatheter aortic valve implantation and surgical aortic valve replacement in elderly patients with severe aortic stenosis and similar baseline electrocardiographic findings. JACC Cardiovasc Interv 2012;5:540-51. [Crossref] [PubMed]
- Petronio AS, Sinning JM, Van Mieghem N, et al. Optimal Implantation Depth and Adherence to Guidelines on Permanent Pacing to Improve the Results of Transcatheter Aortic Valve Replacement With the Medtronic CoreValve System: The CoreValve Prospective, International, Post-Market ADVANCE-II Study. JACC Cardiovasc Interv 2015;8:837-46. [Crossref] [PubMed]
- Gilard M, Eltchaninoff H, Donzeau-Gouge P, et al. Late Outcomes of Transcatheter Aortic Valve Replacement in High-Risk Patients: The FRANCE-2 Registry. J Am Coll Cardiol 2016;68:1637-47. [Crossref] [PubMed]
- Foroutan F, Guyatt GH, Otto CM, et al. Structural valve deterioration after transcatheter aortic valve implantation. Heart 2017. [Epub ahead of print]. [Crossref] [PubMed]
- Roy DA, Schaefer U, Guetta V, et al. Transcatheter aortic valve implantation for pure severe native aortic valve regurgitation. J Am Coll Cardiol 2013;61:1577-84. [Crossref] [PubMed]
- Sawaya FJ, Deutsch MA, Seiffert M, et al. Safety and Efficacy of Transcatheter Aortic Valve Replacement in the Treatment of Pure Aortic Regurgitation in Native Valves and Failing Surgical Bioprostheses: Results From an International Registry Study. JACC Cardiovasc Interv 2017;10:1048-56. [Crossref] [PubMed]
- Wöhrle J, Rodewald C, Rottbauer W. Transfemoral aortic valve implantation in pure native aortic valve insufficiency using the repositionable and retrievable lotus valve. Catheter Cardiovasc Interv 2016;87:993-5. [Crossref] [PubMed]
- Mylotte D, Lefevre T, Sondergaard L, et al. Transcatheter aortic valve replacement in bicuspid aortic valve disease. J Am Coll Cardiol 2014;64:2330-9. [Crossref] [PubMed]
- Seeger J, Gonska B, Rodewald C, et al. Bicuspid Aortic Stenosis Treated With the Repositionable and Retrievable Lotus Valve. Can J Cardiol 2016;32:135 e17-9.
- Ruparelia N, Thomas K, Newton JD, et al. Transfemoral Transcatheter Aortic Valve-in-Valve Implantation for Aortic Valve Bioprosthesis Failure With the Fully Repositionable and Retrievable Lotus Valve: A Single-Center Experience. J Invasive Cardiol 2017. [Epub ahead of print]. [PubMed]


