Acute diseases, emergency admissions and mortality during weekends: should we be worried?
A series of studies has reported a so called “weekend (WE) effect” for hospital admissions, referring to a higher risk for mortality for patients admitted on WE (Saturday to Sunday) than for those admitted on weekdays (WD). A lot of water has flowed under the bridge since, more than fifteen years ago, Bell & Redelmeier reported an association between WE admissions and significantly higher in-hospital mortality (IHM) rates for some acute diseases (1). Interestingly, a higher mortality risk has been reported either from the majority of studies dealing with severe life-threatening diseases, even top rank positioned among the established causes of sudden death (2), such as myocardial infarction and stroke (Table 1), and with many other kinds of admissions as well (Table 2). As for aortic disease, in particular, Bell & Redelmeier found that WE admissions were associated with significantly higher IHM rates than were WD admissions among patients with ruptured abdominal aortic aneurysms (42% vs. 36%, P<0.001), with an odds ratio (OR) of 1.28 (95% confidence interval, 1.13 to 1.46) (1). Two studies from our group, the former conducted on the population of the region Emilia Romagna of Italy (3), the latter on a comprehensive sample of cases of all the regions of Italy (4), confirmed that WE was an independent risk factor for IHM (OR 1.32, 95% confidence interval, 1.14 to 1.52, and OR 1.34, 95% confidence interval, 1.24 to 1.44, respectively). On the other hand, a series of negative findings also exist, and it has been argued that the so-called WE effect could not result in increased mortality but rather affect other quality of care parameters (5). The underlying causal mechanisms are uncertain, and possible concerns can be raised by the wide use of administrative archives as the main source of data, and by the preponderance of data collected in the United States, United Kingdom and Europe, and lack of data from other world regions (6). Among the factors called as a possible explanation for different findings regarding a WE effect (7), some plausible could be (I) suspected suboptimal standards of care and quality of care during WE; (II) differences in case-mix; and (III) disease-specific studies.
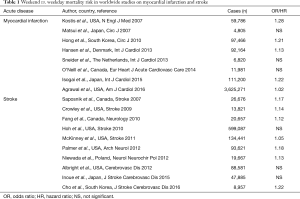
Full table
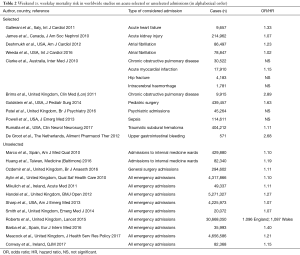
Full table
Suboptimal standard of care and quality of care
Several authors have called reduction in staffing and resources and presence of less experienced doctors as possible causes during WE, also due to the finding that hospitals with admitting consultant presence for a minimum of 4 h per day, had lower adjusted case fatality rates, including the ratio of WE/WD mortality (8). Understaffing is not to be intended as limited to doctors, but refers to nursing staff as well. It has been reported that the risk of death for stroke was higher in the case of a low nurse/bed ratio, and independent of rounds by specialist physicians (9). Studies on possible understaffing led the UK Government to be committed to working with the National Health Service to provide hospital care service with 7-day activity by 2020 (https://www.gov.uk/government/publications/7-day-nhs-services) (10).
Differences in case-mix
More patients are admitted on WD than at WE, and a higher proportion of patients are admitted during WE through the emergency department, therefore patients admitted at WE could have increased illness severity and altered case mix (11). Nanchal et al. reported a 19% increased risk of death in patients admitted on WE for pulmonary embolism (12), and the hypothesis of a higher severity could be strengthened by the existence of several parameters of severity, such as need for mechanical ventilation, thrombolytic therapy use, and use of vasopressors (13).
Disease-specific studies
WE effect appears to be related to mortality especially in conditions at high risk of death immediately following the onset of acute disease, and timely interventions could impact survival. A large study analyzing the database of the US Nationwide Inpatient Sample, reported a reduction over time of the WE effect for myocardial infarction, with a progressive reduction over time from years 2000–2002 (OR 1.10) and 2003–2005 (OR 1.11), and a disappearance in 2006–2008 (OR 1.02, not significant) (14).
In a recent elegant article in Lancet, Walker and colleagues provided novel and interesting evidence with their study on 503,938 emergency admissions to four Oxford University National Health Service hospitals, UK 2006–2014, with a primary outcome of evaluating in- or out-of-hospital death within 30 days of admission (15). The authors designed several models, considering the effect of adjusting for 15 common haematology and biochemistry test results (haemoglobin, platelets, lymphocytes, neutrophils, eosinophils, monocytes, C-reactive protein, urea, bilirubin, creatinine, albumin, alanine aminotransferase, alkaline phosphatase, sodium, and potassium) using the closest result to admission time within 2 days before or after admission. The main results of this study were that 4.7% of WD and 5.1% of WE emergency admissions, respectively, died within 30 days (P<0.0001). Moreover, 9,347 patients underwent 9,707 emergency admissions on public holidays of whom 5.8% died within 30 days (P<0.0001 vs. weekday). The analyzed 15 routine haematology and biochemistry test results were highly prognostic for mortality, since adjustment for test results and standard patient features explained 33% of the excess mortality associated with emergency admission on Saturdays compared with Wednesdays, 52% on Sundays, and 87% on public holidays. Interestingly, despite previous suggestions of the responsibility role played by reduced staffing for excess mortality risk associated with WE admissions, this study did not find any association with mortality and staffing levels and service provision relative to each specific day of the week.
Moreover, Walker and colleagues found that mortality risk differed significantly by admission hour, being lowest at 8–11 AM. Authors reported that circadian variation in mortality risk was as great as (if not greater than) differences in risk between WE and WD. Adding admission hour significantly improve both the statistical models used, and excess mortality risk associated with WE admissions was somewhat greater between 8 AM and midnight, particularly between 11 AM and 3 PM, and somewhat less for admissions from midnight to 8 AM (15).
Such close relationship between time and onset and severity of certain acute diseases is extremely intriguing and fascinating. The cardiovascular system, and most cardiovascular functions, are organized according to a specific circadian order. Since circadian pattern is rhythmic, predictable-in-time differences in the physiological status of the cardiovascular system give rise to rhythmic variations in the susceptibility of human beings to morbid and mortal events (16). On the other hand, the pathological mechanisms of cardiovascular disease themselves exhibit temporal changes in both their manifestation and severity, leading to predictable-in-time differences in their ability to precipitate and graduate the overt expression of disease (16). It is already well known that the occurrence of cardiovascular events is not evenly distributed in time, but shows peculiar temporal patterns that vary with time of the day, the day of the week, and the month of the year. Due to temporal variation in the (I) pathophysiological mechanisms that trigger cardiovascular events and (II) physiological changes in the body rhythms, it is possible that several factors, not harmful if taken alone, may trigger unfavorable events when presenting all together at the same time (chronorisk) (16). Myocardial infarction, for example, exhibits highest frequency of onset during morning hours (6–12 AM). It has been estimated that the incidence rate of acute myocardial infarction (AMI) onset is 40% higher in the morning period than throughout the rest of the day, and nearly 28% of morning infarctions and 22% of sudden cardiac deaths (accounting for approximately 9% and 7% of all AMIs and sudden deaths, respectively), are attributable to the morning excess (17). Moreover, it is possible that time-dependent differences in clinical outcome may be present as well. During 6 AM–noon period, a trend toward a higher frequency of fatal cases was also shown (41.5% vs. 35.2%), independent of age, infarct site, and peak levels of MB creatine-kinase (18). Moreover, a retrospective cohort study conducted in 1,946 consecutive acute coronary syndrome (ACS) admissions to assess presenting clinical variables in patients admitted on days vs. nights and WD vs. WE found that there were fewer ACS admissions than expected on nights and WE (P<0.001), but the proportion of patients with ACS presenting with ST-elevation myocardial infarction (STEMI) was 64% higher on WE (P<0.001) and 31% higher on nights (19). This could explain higher mortality during morning hours and WE.
Walker and colleagues added an important piece to the discussed puzzle of emergency admissions and WE effect (15). They found that 33–52% of the residual excess mortality associated with WE admissions, and 87% of the excess mortality associated with emergency admissions during public holidays, could be explained by results of the selected 15 blood test results. Moreover, mortality was not associated with hospital workload or availability of levels of either staffing and services, and rather differences in clinical conditions of patients admitted during WE compared to WD could contribute to determine worst outcome (15).
Further researches are certainly needed to more-in-depth investigate the underlying factors of the so-called WE effect, and we maybe should keep in our mind that worst outcome could also depend of endogenous factors, including disruption of circadian rhythms (20).
Acknowledgements
Funding: This work was supported, in part, by a scientific research grant [Fondo Ateneo Ricerca 2016 (FAR), prof. Roberto Manfredini] from the University of Ferrara, Italy.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Bell CM, Redelmeier DA. Mortality among patients admitted to hospitals on weekends as compared with weekdays. N Engl J Med 2001;345:663-8. [Crossref] [PubMed]
- Manfredini R, Portaluppi F, Grandi E, et al. Out-of-hospital sudden death referring to an emergency department. J Clin Epidemiol 1996;49:865-8. [Crossref] [PubMed]
- Gallerani M, Imberti D, Bossone E, et al. Higher mortality in patients hospitalized for acute aortic rupture or dissection during weekends. J Vasc Surg 2012;55:1247-54. [Crossref] [PubMed]
- Gallerani M, Volpato S, Boari B, et al. Outcomes of weekend versus weekday admission for acute aortic dissection or rupture: a retrospective study on the Italian National Hospital Database. Int J Cardiol 2013;168:3117-9. [Crossref] [PubMed]
- Black N. Higher Mortality in Weekend Admissions to the Hospital: True, False, or Uncertain? JAMA 2016;316:2593-4. [Crossref] [PubMed]
- Fedeli U, Gallerani M, Manfredini R. Factors Contributing to the Weekend Effect. JAMA 2017;317:1582. [Crossref] [PubMed]
- Lilford RJ, Chen YF. The ubiquitous weekend effect: moving past proving it exists to clarifying what causes it. BMJ Qual Saf 2015;24:480-2. [Crossref] [PubMed]
- Bell D, Lambourne A, Percival F, et al. Consultant input in acute medical admissions and patient outcomes in hospitals in England: a multivariate analysis. PLoS One 2013;8:e61476. [Crossref] [PubMed]
- Bray BD, Ayis S, Campbell J, et al. Associations between stroke mortality and weekend working by stroke specialist physicians and registered nurses: prospective multicentre cohort study. PLoS Med 2014;11:e1001705. [Crossref] [PubMed]
- Collection: NHS 7 days service. Information on the government’s plans for the NHS to provide a 7 day service by 2020. Department of Health, UK Government. 2015 Oct 30. Available online: https://www.gov.uk/government/collections/nhs-7-day-services
- Mikulich O, Callaly E, Bennett K, et al. The increased mortality associated with a weekend emergency admission is due to increased illness severity and altered case-mix. Acute Med 2011;10:182-7. [PubMed]
- Nanchal R, Kumar G, Taneja A, et al. Pulmonary embolism: the weekend effect. Chest 2012;142:690-6. [Crossref] [PubMed]
- Manfredini R, Salmi R, Gallerani M. Weekend effect for pulmonary embolism and other acute cardiovascular diseases. Chest 2013;143:275-6. [Crossref] [PubMed]
- Kumar G, Deshmukh A, Sakhuja A, et al. Acute myocardial infarction: a national analysis of the weekend effect over time. J Am Coll Cardiol 2015;65:217-8. [Crossref] [PubMed]
- Walker AS, Mason A, Quan TP, et al. Mortality risks associated with emergency admissions during weekends and public holidays: an analysis of electronic health records. Lancet 2017;390:62-72. [Crossref] [PubMed]
- Portaluppi F, Manfredini R, Fersini C. From a static to a dynamic concept of risk: the circadian epidemiology of cardiovascular events. Chronobiol Int 1999;16:33-49. [Crossref] [PubMed]
- Cohen MC, Rohtla KM, Lavery CE, et al. Meta-analysis of the morning excess of acute myocardial infarction and sudden cardiac death. Am J Cardiol 1997;79:1512-6. [Crossref] [PubMed]
- Manfredini R, Boari B, Bressan S, et al. Influence of circadian rhythm on mortality after myocardial infarction: data from a prospective cohort of emergency calls. Am J Emerg Med 2004;22:555-9. [Crossref] [PubMed]
- LaBounty T, Eagle KA, Manfredini R, et al. The impact of time and day on the presentation of acute coronary syndromes. Clin Cardiol 2006;29:542-6. [Crossref] [PubMed]
- Manfredini R, Gallerani M. Temporal variation of cardiovascular diseases: an internal biological rhythm disruption may play a role? N Am J Med Sci 2013;5:280-1. [PubMed]


