Outcomes of surgical treatment in 115 patients with primary cardiac tumours: a 15-year experience at a single institution
Introduction
Primary cardiac tumours are rare. According to the literature, the incidence of these tumours at autopsy ranges from 0.001% to 0.030%. Approximately 75% of cardiac tumours are benign, and myxomas account for half of benign tumours. Other benign tumours include lipomas, fibromas, and teratomas. The incidence of metastatic malignant tumours in the heart is 50 times higher than the incidence of primary cardiac tumours. Sarcomas account for 95% of malignant primary cardiac tumours, with the remainder including angiosarcomas, leiomyosarcomas, rhabdomyosarcomas, and lymphomas.
In some patients, cardiac tumours may be associated with clinical symptoms, such as chest tightness, chest pain, dyspnoea, and embolization events. Gross total resection is considered the best treatment modality for cardiac tumours and achieves satisfactory clinical outcomes. Due to the low incidence and highly varied pathological distribution of primary cardiac tumours, most of the published literature in this field consists of case reports. Studies with large sample sizes are lacking, especially in the Chinese population. This study retrospectively analysed 115 consecutive cases of primary cardiac tumours in our centre to explore treatment strategies and prognoses.
Methods
Patient data
From April 2002 to January 2017, 119 consecutive patients with primary cardiac tumours presented to our institution. Four patients declined surgery due to severe illness or for financial reasons, and one patient was hospitalized twice due to tumour recurrence and received a second operation. The 115 patients included in this study ranged from 7 to 85 years in age, with a mean age of 55±14 years. Forty-three patients were male (37.4%). All patients underwent echocardiography and enhanced chest computed tomography (CT) to determine the size and location of the tumour prior to surgery. Surgery was performed using a median sternotomy and a right atrial approach under cardiopulmonary bypass. The patients were divided into three groups according to their tumour pathology (myxomas, other benign tumours, and malignant tumours). Eighty-four patients (73.0%) were followed up for 8–147 months (mean 40.8±31.2 months).
Statistical analysis
The baseline patient data were obtained from the Department of Cardiothoracic Surgery at Nanjing Drum Tower Hospital. Two cardiothoracic surgeons conducted follow-up assessments using written correspondence with local physicians and telephone questionnaires administered to the patients or their families. The Shapiro-Wilk test was used to examine the normality of the data. All continuous and categorical variables with normal distributions were analysed for heterogeneity using one-way ANOVA with the multiple comparison post hoc test and the Chi-square test, respectively. Data with non-normal distributions were analysed using the Kruskal-Wallis test with adjustments for multiple comparisons. The Kaplan-Meier method was used to analyse long-term survival, and the log-rank test was used to identify significant differences between groups. The Cox proportional multivariate analysis was used to identify the most significant mortality predictors. After the univariate analysis, risk factors with a P value <0.1 were selected for the multivariate model. All statistical analyses were performed with SPSS 24.0 (IBM, Armonk, NY, USA). A P value <0.05 was considered significant.
Results
Baseline data
A review of the patients’ baseline data (Table 1) showed that 87 (75.7%) patients suffered from the following clinical symptoms: 86 (74.1%) patients had chest tightness and dyspnoea and 26 (22.6%) had embolic symptoms. Based on their symptoms, 11 (9.6%), 24 (20.9%), 62 (53.9%), and 18 (15.7%) patients were classified as New York Heart Association (NYHA) classes I, II, III, and IV, respectively. Most patients (74.8%) belonged to NYHA classes II and III. Twenty-five patients in the myxomas group and one patient with another type of benign tumour had embolic symptoms, including stroke, pulmonary embolism, and limb embolism. No significant differences in the baseline data were observed among the patients with myxomas, other benign tumours, and malignant tumours except for the right ventricular systolic pressure (42.2±17.2 vs. 32.3±14.1 vs. 58.2±20.8 mmHg respectively, P=0.011).
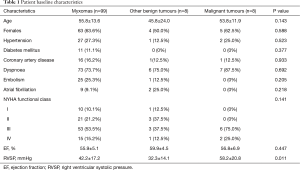
Full table
Diagnosis
All patients were diagnosed by echocardiography. Twenty-eight patients (24.3%) had cardiac murmurs found incidentally on chest auscultation during routine examinations. After admission, all patients underwent enhanced CT to precisely identify the tumour location. Due to equipment and economic limitations, most patients declined cardiac magnetic resonance imaging (MRI) and/or three-dimensional echocardiography. The left atrium (76.5%) was the predominant location of the primary cardiac tumours (Table 2). No aortic valve tumours were detected in our patients, but 6 tumours were found on the mitral valve and 3 on the tricuspid valve. The distribution of the tumour pathology differed by location. For example, myxomas accounted for 98.9% of the tumours in the left atrium compared to 43.8% of the tumours in the right atrium. Similarly, the distribution of the tumour locations differed by pathological type. The left atrium (87.9%) was the most frequent site in the myxomas group, whereas 75% of the other benign tumours originated in the right atrium. In contrast, malignant tumours were distributed uniformly throughout the heart, including the valves. Another interesting finding was that the left ventricular tumours did not cause moderate or severe mitral regurgitation. However, tumours in the right heart, especially tricuspid valve and right ventricular tumours, all caused moderate or severe tricuspid regurgitation and elevated right ventricular systolic pressure (P=0.031). Additionally, tricuspid valve tumours were associated with a lower ejection fraction (EF) (P=0.036).
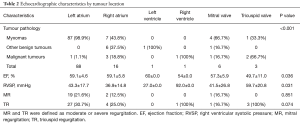
Full table
Surgical outcomes
All patients underwent median sternotomy and cardiopulmonary bypass, and the surgeons used a right atrial approach. For tumours in the left heart, the atrial septum was incised to expose the tumour. Gross total resection was performed in all patients. When the patients had moderate or severe regurgitation at the mitral or tricuspid valve, valve repair or replacement was performed to relieve the regurgitation, especially in patients with valve tumours. A total of 3 mitral valve replacements, 34 mitral valve repairs, and 56 tricuspid valve repairs were performed. Cardiac reconstruction using autologous pericardial or bovine pericardial patches was commonly performed for atrial tumours, especially those that invaded the atrium. Atrial fibrillation ablation (3 patients) or coronary artery bypass grafting (11 patients) was performed concomitantly if needed (Table 3). All patients were transferred into an intensive care unit (ICU) and then were transferred out of the ICU after tracheal extubation and haemodynamic stabilization. Postoperative echocardiography and chest X-rays were performed in all patients to confirm the success of the operation.
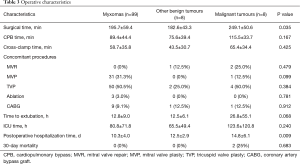
Full table
The surgical time (P=0.035) and hospitalization time (P=0.009) were significantly longer among the patients with malignant tumours than among the patients in the other two groups. A total of 13 patients had a prolonged ICU stay (>120 h), of whom 6 had delayed extubation (>24 h). The time to extubation and the duration of the ICU stay were also longer in the malignant tumour group, although these differences were not significant. Two patients in the myxomas group underwent re-operation due to bleeding. Four patients in the myxomas group and 1 patient in the malignant tumour group developed acute kidney insufficiency. Postoperative echocardiography showed complete excision of the tumours in all patients, and all patients with high preoperative right ventricular systolic pressures showed a marked decrease. All patients with benign tumours were discharged uneventfully, whereas 2 (25%) patients in the malignant tumour group died. According to the pathological results, the group with other benign tumours included 3 fibromas, 3 lipomas, 1 atrioventricular node cystic tumour, and 1 mesothelioma. The malignant group included 3 pulmonary vein endothelial sarcomas (including 1 case of recurrence), 2 angiosarcomas, 1 Burkitt lymphoma, 1 malignant fibroma, and 1 rhabdomyosarcoma.
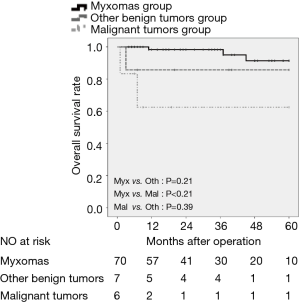
Survival analysis
A total of 84 (73.0%) patients were followed up, and Kaplan-Meier survival curves were generated based on the patient outcomes (Figure 1). The 5-year survival rate was 95.7% in the myxomas group, 85.7% in the patients with other benign tumours, and 57.1% in the patients with malignant tumours (P=0.003). No significant difference was observed between the myxomas group and the other benign tumour group (P=0.21), but survival was significantly higher in the myxomas group than in the malignant tumour group (P<0.001). No significant difference in survival was observed between the patients with other benign tumours and those with malignant tumours (P=0.39). No recurrence was observed among the patients with myxomas and other benign tumours. However, one patient with pulmonary vein endothelial sarcoma underwent a second operation 10 years after the first procedure due to recurrence at the same site and is now recovering well. None of the patients with malignant tumours received chemotherapy or radiotherapy postoperatively. Of the four patients who did not undergo surgery, 2 died from cardiac-related causes at 2 and 6 months after the diagnosis of their cardiac tumours.
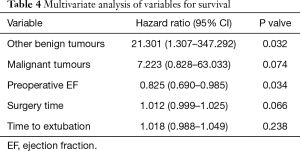
The Cox proportional multivariate analysis (Table 4) with an excellent discriminatory ability (P<0.0001) confirmed that the tumour histology was the strongest predictor of survival. Patients with other benign tumours might suffer worse survival (HR=21.301, 95% CI, 1.307–347.292, P=0.032), whereas malignant tumours showed a trend as a risk factor, although the difference was not significant (HR=7.223, 95% CI, 0.828–63.033, P=0.074). Another great predictor was the preoperative EF (HR=0.825, 95% CI, 0.690–0.985, P=0.034), with a better preoperative EF potentially decreasing the hazard of death.
Full table
Discussion
Primary cardiac tumours are rare, and few retrospective studies are available in the literature. The pathological type of cardiac tumours has a significant effect on the treatment and prognosis. ElBardissi et al. (1) reviewed 323 patients examined from 1957 to 2006 at the Mayo Clinic and found that 50% of the primary cardiac tumours were myxomas and 26% were papillary fibroelastomas. Other studies have reported a proportion of myxomas of less than 75% (2,3). However, in our report, 86% of the patients were diagnosed with myxomas. This difference has two possible explanations. First, the aetiology and epidemiology of cardiac tumours remain unclear, and the incidence of other tumours, especially papillary myxomas, is most likely lower in the Chinese population. Second, the diagnosis of asymptomatic cardiac tumours relies on echocardiography, CT, cardiac MRI, or even cardioangiography (2-7). Most papillary fibroelastomas are detected incidentally (1), often during routine examinations. However, in China, routine examinations are still not universal, and the level of diagnostic evaluation available in primary-level hospitals is insufficient to identify patients with cardiac tumours.
Blockage of the outflow tract and tumour fragmentation leading to embolic symptoms are the main dangerous complications of cardiac tumours (8). ElBardissi et al. (9) reported that the incidence of embolic events was 24.8% and that left atrium and aortic valve tumours were more likely to cause embolic events. A small volume and an absence of mitral regurgitation may be risk factors for embolic events. Nevertheless, embolic events do not affect the long-term survival of patients. The incidence of embolic events in our patients was 22.6%, and the vast majority occurred in the myxomas group. All patients with embolic events had good outcomes, and none of these patients died within 30 days of surgery.
Gross total resection is the gold standard treatment for cardiac tumours (10,11). For benign tumours, gross total resection can achieve outcomes similar to radical resection in most cases (12,13). The outcomes of gross total resection also depend on the tumour location and pathological characteristics. Gross total resection can be performed successfully for most tumours in the left or right atrium, especially myxomas with the tumour pedicle connected to the atrial septum. However, gross total resection is much more difficult to perform for valvular tumours and invasive malignant tumours (11,14). For these patients, cardiac reconstruction and valve repair or replacement should be performed simultaneously to achieve optimal results. For some malignant tumours that are too difficult to remove using gross total resection, en bloc resection or debulking should be performed to reduce the tumour volume and prevent blockage of the valves or the outflow tract, because these procedures can effectively relieve symptoms.
Most cardiac primary malignant tumours are associated with a poor prognosis, with even patients who undergo adjuvant chemotherapy or radiotherapy showing poor postoperative survival (1,11,14,15). A recent study by Pacini and colleagues (14) reported an average survival time of 28.8±28 months in 14 patients with cardiac malignant tumours treated by surgery combined with radiotherapy and adjuvant chemotherapy. Simpson et al. (16) reported that the median survival for patients who underwent complete surgical excision was 17 months compared to 6 months for patients whose tumours could not be completely removed by surgery. The survival time is also related to the pathological tumour types. In our study, although patients with malignant tumours had worse symptoms, more difficult surgeries and higher in-hospital mortality, more than half of these patients achieved satisfactory long-term survival, possibly due to early detection and timely radical resection. The older ages of the patients in our study may also account for the increased survival, because the median age in Simpson’s study was only 44 years (16). The only established treatment for cardiac malignant tumours is radical resection when possible; additionally, no clear standard for adjuvant chemotherapy or radiotherapy exists, which may be another reason for the poor survival of these patients. Randomized controlled trials are required to provide more convincing evidence and to guide the treatment of malignant tumours.
Recurrence of primary cardiac tumours has mainly been reported in myxoma cases. Some reports describe 3% recurrence in sporadic myxomas compared to 22% in familial myxomas (1,17-19). Reber et al. (20) reported that recurrence may be due to incomplete resection. Non-myxomatous tumours have a higher incidence of long-term recurrence, which can be as high as 30% in some instances. Recurrence of primary cardiac tumours peaks 4 years after surgery and then gradually decreases (1). In our study, we did not observe any recurrence of myxomas; the only case of recurrence occurred in a patient with pulmonary vein endothelial sarcoma who relapsed 10 years after the first surgery, underwent a second operation, and had an excellent quality of life at 12 months of follow-up. The low observed recurrence in our study may be due to the short duration of follow-up and the fact that most of our patients had sporadic rather than familial tumours. Additionally, gross total resection may also be key in preventing tumour recurrence.
We presented a study of surgical results and follow-up for primary cardiac tumours spanning a 14-year period. This study has some limitations, especially regarding the observation period. First, this study is a single-centre retrospective study, and the number of patients is small, especially in the other benign tumour group and the malignant tumour group. This issue may have resulted in a relatively large random error. Second, the short duration of follow-up may have resulted in biased estimates of recurrence and survival. A follow-up duration of 10 years or more would allow for better assessment of these outcomes. Third, due to ongoing social developments in China, many patients had a change of address and contact information at least 2–3 times during the study, which resulted in considerable loss of follow-up. Despite these limitations, we believe that our study provides valuable perioperative and follow-up data for patients with primary cardiac tumours in the Chinese population, which will be useful for cardiac surgeons.
Conclusions
Gross total resection of primary cardiac tumours is an effective treatment approach. The prognosis is significantly associated with the pathological tumour type. The surgical time and postoperative hospitalization time are also associated with the prognosis. The incidence of myxomas in the Chinese population is higher than the incidence reported elsewhere, and the relapse rate is relatively low. Overall, patients with benign tumours enjoyed a satisfactory prognosis, whereas the outcomes for patients with malignant tumours were poor. Early detection and radical resection may extend survival.
Acknowledgements
Funding: This work was supported by the Fundamental Research Funds for the Central Universities (No. 021414380190).
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The study was approved by the institutional ethics board of Nanjing Drum Tower Hospital (No. 2017-089-01).
References
- Elbardissi AW, Dearani JA, Daly RC, et al. Survival after resection of primary cardiac tumors: a 48-year experience. Circulation 2008;118:S7-15. [Crossref] [PubMed]
- Hoey ET, Mankad K, Puppala S, et al. MRI and CT appearances of cardiac tumours in adults. Clin Radiol 2009;64:1214-30. [Crossref] [PubMed]
- Colin GC, Dymarkowski S, Gerber B, et al. Cardiac myxoma imaging features and tissue characteristics at cardiovascular magnetic resonance. Int J Cardiol 2016;202:950-1. [Crossref] [PubMed]
- Butany J, Nair V, Naseemuddin A, et al. Cardiac tumours: diagnosis and management. Lancet Oncol 2005;6:219-28. [Crossref] [PubMed]
- Fussen S, De Boeck BW, Zellweger MJ, et al. Cardiovascular magnetic resonance imaging for diagnosis and clinical management of suspected cardiac masses and tumours. Eur Heart J 2011;32:1551-60. [Crossref] [PubMed]
- Maraj S, Pressman GS, Figueredo VM. Primary cardiac tumors. Int J Cardiol 2009;133:152-6. [Crossref] [PubMed]
- Shapiro LM. Cardiac tumours: diagnosis and management. Heart 2001;85:218-22. [Crossref] [PubMed]
- Shimizu Y, Itoda Y, Higashikuni Y, et al. Giant left atrial myxoma that caused mitral valve obstruction and pulmonary hypertension. Int J Cardiol 2015;199:38-9. [Crossref] [PubMed]
- Elbardissi AW, Dearani JA, Daly RC, et al. Embolic potential of cardiac tumors and outcome after resection: a case-control study. Stroke 2009;40:156-62. [Crossref] [PubMed]
- Gošev I, Paic F, Duric Z, et al. Cardiac myxoma the great imitators: comprehensive histopathological and molecular approach. Int J Cardiol 2013;164:7-20. [Crossref] [PubMed]
- Neragi-Miandoab S, Kim J, Vlahakes GJ. Malignant tumours of the heart: a review of tumour type, diagnosis and therapy. Clin Oncol (R Coll Radiol) 2007;19:748-56. [Crossref] [PubMed]
- ElBardissi AW, Dearani JA, Daly RC, et al. Analysis of benign ventricular tumors: long-term outcome after resection. J Thorac Cardiovasc Surg 2008;135:1061-8. [Crossref] [PubMed]
- Pacini D, Careddu L, Pantaleo A, et al. Primary benign cardiac tumours: long-term results. Eur J Cardiothorac Surg 2012;41:812-9. [Crossref] [PubMed]
- Pacini D, Careddu L, Pantaleo A, et al. Primary malignant tumors of the heart: Outcomes of the surgical treatment. Asian Cardiovasc Thorac Ann 2015;23:645-51. [Crossref] [PubMed]
- Bakaeen FG, Jaroszewski DE, Rice DC, et al. Outcomes after surgical resection of cardiac sarcoma in the multimodality treatment era. J Thorac Cardiovasc Surg 2009;137:1454-60. [Crossref] [PubMed]
- Simpson L, Kumar SK, Okuno SH, et al. Malignant primary cardiac tumors: review of a single institution experience. Cancer 2008;112:2440-6. [Crossref] [PubMed]
- Kuroczyński W, Peivandi AA, Ewald P, et al. Cardiac myxomas: short- and long-term follow-up. Cardiol J 2009;16:447-54. [PubMed]
- Padalino MA, Basso C, Milanesi O, et al. Surgically treated primary cardiac tumors in early infancy and childhood. J Thorac Cardiovasc Surg 2005;129:1358-63. [Crossref] [PubMed]
- Vroomen M, Houthuizen P, Khamooshian A, et al. Long-term follow-up of 82 patients after surgical excision of atrial myxomas. Interact Cardiovasc Thorac Surg 2015;21:183-8. [Crossref] [PubMed]
- Reber D, Birnbaum DE. Recurrent cardiac myxoma: why it occurs. A case report with literature review. J Cardiovasc Surg (Torino) 2001;42:345-8. [PubMed]


