Taking the measure of lung adenocarcinoma: towards a quantitative approach to tumor spread through air spaces (STAS)
In less than a decade, we have witnessed dramatic changes in the histologic classification of lung adenocarcinoma. In 2011, the International Association for the Study of Lung Cancer, the American Thoracic Society, and the European Respiratory Society (IASLC/ATS/ERS) put forth a new adenocarcinoma classification (1) that recognizes five major histologic patterns (lepidic, acinar, papillary, solid, and micropapillary) with prognostic implications that have been validated extensively (2-4) and adopted by the World Health Organization (WHO) classification of Tumours of the Lung, Pleura, Thymus and Heart 4th edition 2015 (5). Shortly thereafter, we and a group of researchers from the Memorial Sloan Kettering Cancer Center (MSKCC) independently reported distinct patterns of tumor extension through the air spaces of the lung (6,7), which are now encompassed by the concept of tumor “spread through air spaces” (STAS). STAS is currently considered as a novel pattern of invasion in lung adenocarcinoma by the WHO 2015 classification (5) and recent studies from different countries have corroborated the association between the presence of STAS and adverse pathological features (e.g., lymphovascular invasion, high-grade histologic subtypes), EGFR wild-type, and higher risk of recurrence and death in resected (early-stage and advanced) lung adenocarcinomas (Table 1) (8-10).
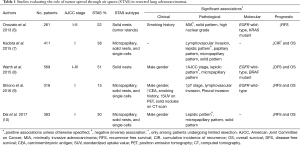
Full table
Given our very recent appreciation of STAS, several questions about this entity remain unanswered. One such question is whether the amount of STAS in a tumor matters. Up until now, studies have focused predominantly on the presence or absence of STAS but not on its quantity. What are the clinical and prognostic implications of small amounts of STAS? Do increasing amounts of STAS lead to worse outcomes? In a study recently published in the Journal of Thoracic Oncology, Uruga et al. shed light on this issue for the first time (11). The authors evaluated the relationship between the amount of STAS and clinicopathological features, recurrence-free survival (RFS), and overall survival (OS) in 208 patients who underwent lobectomy or limited resection for small (≤2 cm) Stage I lung adenocarcinomas at their institution. In accordance with the original report by Kadota et al., the authors defined STAS as “tumor cells within air spaces beyond the edge of the main tumor” and classified it as (I) micropapillary structures, (II) solid nests/tumor islands, or (III) scattered dyscohesive single cells (7). Using a semi-quantitative approach, the authors assessed the amount of STAS in a tumor as no STAS, low STAS (1–4 tumor cell clusters in tumors with micropapillary- or solid subtype of STAS, or 1–4 of tumor cells in those with single-cell predominant STAS), and high STAS (≥5 tumor cell clusters in those with micropapillary- or solid subtype of STAS, or ≥5 tumor cells in those with single-cell predominant STAS).
In their results, Uruga et al. found that 52.4% of tumors had no STAS, 18.3% had low STAS, and 29.3% had high STAS. Higher amounts of STAS were associated with pleural invasion (P<0.001), lymphovascular invasion (P<0.001), and tumor size ≥10 mm (P=0.037). The quantity of STAS was also associated with predominant histologic pattern. While solid-predominant pattern was found in 16% of tumors with high STAS, it was seen only in 8% and 2% of those with low and no STAS, respectively (P<0.001). Conversely, lepidic-predominant pattern was observed in only 3% of tumors with high STAS, and in 16% of both low and no STAS tumors (P<0.001). Notably, the authors did not report on the relationship between STAS and the micropapillary-predominant histologic pattern.
Importantly, high amounts of STAS were associated with higher risk of recurrence and mortality compared to no STAS. After adjusting for presence of lymphovascular invasion and the predominant histologic pattern, patients with high STAS had a hazard ratio (HR) for RFS of 7.34 (95% CI: 1.54–35.17) compared to patients with no STAS, and this difference was statistically significant. When compared to patients with low STAS, those with high STAS had higher risk of recurrence but this had limited statistical significance (HR for RFS 4.45, 95% CI: 0.96–20.56). Presence of low STAS was not significantly associated with worse RFS (HR 1.65, 95% CI: 0.23–12.00) compared to no STAS. Similarly, multivariate analysis revealed that high STAS was associated with significantly poorer OS compared to no STAS (HR for OS 4.17, 95% CI: 1.14–15.20) but not compared to low STAS (HR for OS 2.10, 95% CI: 0.61–7.29). Patients with low STAS demonstrated statistically similar OS compared to those with no STAS (HR for OS 1.98, 95% CI: 0.53–7.48).
Interestingly, nearly all patients with high STAS underwent lobectomy (95%), compared with 79% and 69% of patients with low and no STAS, respectively (P<0.001). Thus, the authors performed secondary analyses stratified by the type of resection. In patients who underwent lobectomy, high STAS was associated with worse RFS (median 140.4, 150.4, and 116.3 months for patients with no-, low-, and high STAS, respectively, P<0.001). Among patients who underwent limited resection, there was a strong trend towards worse RFS in those with high STAS (median 152.9, 117.5, and 85.8 months for patients with no-, low-, and high STAS, respectively, P=0.084) but it did not reach statistical significance, possibly due to the small number of patients in the limited resection group (n=45).
In summary, the study by Uruga et al. confirms the previous findings that presence of STAS is associated with adverse pathological features such as lymphovascular invasion and solid-predominant histologic pattern of invasion. The novel and most important finding of this study is the prognostic relevance of the amount of STAS in a tumor, beyond its mere presence or absence. The results clearly demonstrated that high amounts of STAS (defined as 5 or more clusters/single tumor cells) were associated with poor RFS and OS compared to no STAS. Whether high amounts of STAS are associated with worse patient outcomes compared to low STAS is not entirely clear. While there was a significant difference in median RFS (115.6 and 154.2 months, respectively) between the two groups by the log-rank test, multivariate analysis of RFS had limited statistical significance, potentially due to small sample size (only 38 patients, or 18% of the entire cohort, had low STAS). More importantly, the results of this study strongly suggest that small amounts of STAS have little or no prognostic value for disease recurrence rates.
Taken together, these data suggest that not all early-stage adenocarcinomas with STAS behave similarly: tumors with high amounts of STAS exhibit a very high risk of disease recurrence after resection, while those with small amounts of STAS have similar recurrence rates to those with no STAS. As it is often the case, these answers have led to even more questions.
The study by Uruga et al. represents the first effort towards a standardized, quantitative appreciation of STAS. The quantitative measurement can be helpful in the histologic classification and risk-stratification, as evidenced by the IASL/ATS/ERS semi-quantitative assessment of the predominant histologic pattern for lung adenocarcinoma. The amount of STAS in a tumor, however, is not the only measure that may play a role in prognosis: its distance from the main tumor mass has also been a focus of interest. In a study with 569 resected lung adenocarcinomas of all stages, Warth et al. (8) assessed whether STAS located <3 alveoli away from the main tumor mass (denominated “limited” STAS) and STAS located >3 alveoli away from the main tumor mass (“extensive” STAS) had distinct prognoses. The authors found that patients with limited and extensive STAS had significantly worse outcomes than patients with no STAS, but there was no difference in outcomes between limited and extensive STAS. Of interest, they did find that extensive STAS was strongly associated with micropapillary-predominant tumors. Unfortunately, however, the authors did not perform an analysis restricted to patients with Stage I tumors or stratified by type of resection.
There are three additional questions that are germane to the findings of Uruga et al. The first one pertains to the relationship between STAS and the micropapillary histologic pattern. The association between these two entities is well documented (6-8). In fact, one of the morphological subtypes of STAS consists of “small papillary structures without central fibrovascular cores” compatible with the cytoarchitectural features of the micropapillary pattern (7). Several studies have demonstrated that resected lung adenocarcinomas with micropapillary-predominant pattern show increased recurrence and mortality rates (2,3,12-14). Moreover, even very small fractions of micropapillary pattern (1%, 5%, and 10%) have been associated with poor patient outcomes in multiple series (15-17). It has been hypothesized that these small fractions of micropapillary pattern may represent the micropapillary subtype of STAS (7). Given the above evidence, it is perplexing that the association of micropapillary pattern and high STAS was not reported in the study by Uruga et al. It is also interesting to see whether the subtype of STAS (micropapillary, solid nests, or single cells) has prognostic significance, and larger scale studies evaluating this question are warranted.
The second question is whether the amount of STAS plays a significant role in determining the type of resection for patients with early-stage lung adenocarcinomas, in particular for those with comorbidities. Lobectomy with hilar and mediastinal lymph node dissection is the procedure of choice for the treatment of early-stage lung adenocarcinomas; however, growing evidence suggests that limited resection (wedge resection and segmentectomy) may be an effective and safe approach to removing small (≤2 cm) peripheral tumors while preserving pulmonary function (18-20). Before the formal introduction of STAS, another study from the MSKCC group found that the presence of even a small micropapillary component (≥5% of tumor cells) in patients with small (≤2 cm) adenocarcinomas undergoing limited resection was associated with higher risk of recurrence (most of which were locoregional), but this association was not seen among patients undergoing lobectomy (20). Moreover, micropapillary components were associated with local recurrences in resections with narrow surgical margins (<1 cm) but not in those with wider margins. Thus, the presence of a micropapillary histologic pattern has important surgical implications for small tumors. Similarly, in their original report, Kadota et al. (7) found that STAS was an independent predictor of disease recurrence (both locoregional and distant) in patients with Stage I adenocarcinomas undergoing limited resection, while the presence of STAS did not influence recurrence rates among patients who underwent lobectomy. In their study, Uruga et al. found that among patients undergoing limited resection, those with increasing amounts of STAS had shorter RFS. While this difference was not statistically significant, the analysis was potentially underpowered by the small sample size. These findings suggest that patients whose tumors demonstrate micropapillary pattern and/or STAS, in particular, high STAS may warrant lobectomy and raise the question of whether these patients could benefit from intensified locoregional and/or systemic treatment regimens in the postoperative setting.
Lastly but not the least, we must acknowledge that while the prognostic significance of STAS in lung adenocarcinoma continues to be validated—and more recently also in lung squamous cell carcinoma (21,22)—there are alternative perspectives that suggest STAS may not be a biological phenomenon, but rather an artifact resulting from mechanical manipulation of the lung specimen during operation and/or gross examination (23). Thunnissen et al. described an incidence reportedly occurring at the time of specimen prospection whereby tumor cells would be mobilized by the knife along the plane of sectioning—“spreading through a knife surface” (STAKS) (24). Tumor cells displaced in this fashion may thus be trapped in the empty air spaces as free-floating tumor cell clusters and interpreted as STAS (23). In a prospective, multi-center study with forty-four resected lung cancers (26 of which were adenocarcinomas), Blaauwgeers et al. (23) observed free-floating tumor cell clusters in 73% of the cases and attributed 93% of these to mechanical artifacts, predominantly following sequential specimen sectioning using the same knife without cleaning it between the sections. They found that the number of cell clusters significantly increased with the number of sections, and that micropapillary-predominant lung adenocarcinomas demonstrated higher numbers of these clusters. The authors hypothesized that rather than an actual mechanism of invasion, what has been described as STAS may be an artifact reflecting tumor cell dyshesion, such that tumors with poor intercellular cohesion (which is a feature of micropapillary pattern) would be more prone to tumor cell displacement. More prospective studies will be necessary to better characterize the nature of STAS, but irrespective of whether STAS represents an artifactual surrogate of aggressive tumor biology or a true biological phenomenon, the presence of tumor cell clusters floating in alveoli away from the main tumor has consistently proven to be a marker of poor patient outcomes, and the number of these tumor cell clusters may correlate with aggressiveness of the tumor.
In conclusion, the study by Uruga et al. represents an important step forward in the research of STAS. As our understanding of this entity evolves, we face numerous new challenges. One of them is to determine whether we can reliably identify STAS at the time of intraoperative consultation to aid decision-making on the extent of surgical resection during operation. Data about our ability to detect STAS in frozen section specimens is lacking, but recent evidence on the accuracy of histologic pattern classification in frozen sections suggests that it will be an extremely challenging endeavor (25). Further, if more studies continue to validate the adverse recurrence rates associated with STAS in resected lung adenocarcinomas, we will need to assess a role for adjuvant therapy to improve the outcomes of these high-risk patients.
Acknowledgements
None.
Footnote
Conflicts of Interest: V Morales-Oyarvide has no conflicts of interest to declare. M Mino-Kenudson has served as a consultant for Merrimack Pharmaceuticals, H3 Biomedicine, and Advanced Cell Diagnostics and as an advisory board member for Roche.
References
- Travis WD, Brambilla E, Noguchi M, et al. International Association for the Study of Lung Cancer/American Thoracic Society/European Respiratory Society international multidisciplinary classification of lung adenocarcinoma. J Thorac Oncol 2011;6:244-85. [Crossref] [PubMed]
- Yoshizawa A, Sumiyoshi S, Sonobe M, et al. Validation of the IASLC/ATS/ERS lung adenocarcinoma classification for prognosis and association with EGFR and KRAS gene mutations: analysis of 440 Japanese patients. J Thorac Oncol 2013;8:52-61. [Crossref] [PubMed]
- Tsuta K, Kawago M, Inoue E, et al. The utility of the proposed IASLC/ATS/ERS lung adenocarcinoma subtypes for disease prognosis and correlation of driver gene alterations. Lung Cancer 2013;81:371-6. [Crossref] [PubMed]
- Rocco R, Jones DR, Morabito A, et al. Validation of the new IASLC/ATS/ERS lung adenocarcinoma classification: a surgeon's perspective. J Thorac Dis 2014;6:S547-51. [PubMed]
- Travis W, Brambilla E, Burke A, et al. WHO Classification of Tumours of the Lung, Pleura, Thymus and Heart. 4th ed. Lyon, France: International Agency for Research on Cancer, 2015. World Health Organization Classification of Tumours, vol. 7.
- Onozato ML, Kovach AE, Yeap BY, et al. Tumor islands in resected early-stage lung adenocarcinomas are associated with unique clinicopathologic and molecular characteristics and worse prognosis. Am J Surg Pathol 2013;37:287-94. [Crossref] [PubMed]
- Kadota K, Nitadori J, Sima CS, et al. Tumor Spread through Air Spaces is an Important Pattern of Invasion and Impacts the Frequency and Location of Recurrences after Limited Resection for Small Stage I Lung Adenocarcinomas. J Thorac Oncol 2015;10:806-14. [Crossref] [PubMed]
- Warth A, Muley T, Kossakowski CA, et al. Prognostic Impact of Intra-alveolar Tumor Spread in Pulmonary Adenocarcinoma. Am J Surg Pathol 2015;39:793-801. [Crossref] [PubMed]
- Shiono S, Yanagawa N. Spread through air spaces is a predictive factor of recurrence and a prognostic factor in stage I lung adenocarcinoma. Interact Cardiovasc Thorac Surg 2016;23:567-72. [Crossref] [PubMed]
- Dai C, Xie H, Su H, et al. Tumor Spread through Air Spaces Affects the Recurrence and Overall Survival in Patients with Lung Adenocarcinoma >2 to 3 cm. J Thorac Oncol 2017;12:1052-60. [Crossref] [PubMed]
- Uruga H, Fujii T, Fujimori S, et al. Semiquantitative Assessment of Tumor Spread through Air Spaces (STAS) in Early-Stage Lung Adenocarcinomas. J Thorac Oncol 2017;12:1046-51. [Crossref] [PubMed]
- Kadota K, Yeh YC, Sima CS, et al. The cribriform pattern identifies a subset of acinar predominant tumors with poor prognosis in patients with stage I lung adenocarcinoma: a conceptual proposal to classify cribriform predominant tumors as a distinct histologic subtype. Mod Pathol 2014;27:690-700. [Crossref] [PubMed]
- Zhang J, Wu J, Tan Q, et al. Why do pathological stage IA lung adenocarcinomas vary from prognosis?: a clinicopathologic study of 176 patients with pathological stage IA lung adenocarcinoma based on the IASLC/ATS/ERS classification. J Thorac Oncol 2013;8:1196-202. [Crossref] [PubMed]
- Gu J, Lu C, Guo J, et al. Prognostic significance of the IASLC/ATS/ERS classification in Chinese patients-A single institution retrospective study of 292 lung adenocarcinoma. J Surg Oncol 2013;107:474-80. [Crossref] [PubMed]
- Cha MJ, Lee HY, Lee KS, et al. Micropapillary and solid subtypes of invasive lung adenocarcinoma: clinical predictors of histopathology and outcome. J Thorac Cardiovasc Surg 2014;147:921-8.e2. [Crossref] [PubMed]
- Sumiyoshi S, Yoshizawa A, Sonobe M, et al. Pulmonary adenocarcinomas with micropapillary component significantly correlate with recurrence, but can be well controlled with EGFR tyrosine kinase inhibitors in the early stages. Lung Cancer 2013;81:53-9. [Crossref] [PubMed]
- Koga K, Hamasaki M, Kato F, et al. Association of c-Met phosphorylation with micropapillary pattern and small cluster invasion in pT1-size lung adenocarcinoma. Lung Cancer 2013;82:413-9. [Crossref] [PubMed]
- Berfield KS, Wood DE. Sublobar resection for stage IA non-small cell lung cancer. J Thorac Dis 2017;9:S208-S210. [Crossref] [PubMed]
- Veluswamy RR, Ezer N, Mhango G, et al. Limited Resection Versus Lobectomy for Older Patients With Early-Stage Lung Cancer: Impact of Histology. J Clin Oncol 2015;33:3447-53. [Crossref] [PubMed]
- Nitadori J, Bograd AJ, Kadota K, et al. Impact of micropapillary histologic subtype in selecting limited resection vs lobectomy for lung adenocarcinoma of 2cm or smaller. J Natl Cancer Inst 2013;105:1212-20. [Crossref] [PubMed]
- Kadota K, Kushida Y, Katsuki N, et al. Tumor Spread Through Air Spaces Is an Independent Predictor of Recurrence-free Survival in Patients With Resected Lung Squamous Cell Carcinoma. Am J Surg Pathol 2017;41:1077-86. [Crossref] [PubMed]
- Lu S, Tan KS, Kadota K, et al. Spread through Air Spaces (STAS) Is an Independent Predictor of Recurrence and Lung Cancer-Specific Death in Squamous Cell Carcinoma. J Thorac Oncol 2017;12:223-34. [Crossref] [PubMed]
- Blaauwgeers H, Flieder D, Warth A, et al. A Prospective Study of Loose Tissue Fragments in Non-Small Cell Lung Cancer Resection Specimens: An Alternative View to "Spread Through Air Spaces". Am J Surg Pathol 2017;41:1226-30. [Crossref] [PubMed]
- Thunnissen E, Blaauwgeers HJ, de Cuba EM, et al. Ex Vivo Artifacts and Histopathologic Pitfalls in the Lung. Arch Pathol Lab Med 2016;140:212-20. [Crossref] [PubMed]
- Trejo Bittar HE, Incharoen P, Althouse AD, et al. Accuracy of the IASLC/ATS/ERS histological subtyping of stage I lung adenocarcinoma on intraoperative frozen sections. Mod Pathol 2015;28:1058-63. [Crossref] [PubMed]


