Navigation-assisted bronchoscopy for ground-glass opacity lesions
We thank Dr. Chaves and colleagues for their interest and comments on our article (1). We have attempted to diagnose ground-glass opacity (GGO)-predominant-type lesions by bronchoscopic biopsy using endobronchial ultrasonography with a guide sheath (EBUS-GS) (1,2). The diagnostic rate of GGO-predominant-type lesions is lower than that of solid-type lesions. One of the reasons for this is that the lesions may not be visible under X-ray fluoroscopy. Identifying the bronchial routes to reach GGO lesions within a limited examination time is not easy. We have previously reported a retrospective study that evaluated the efficacy of EBUS-GS combined with a virtual bronchoscopic navigation (VBN) system for diagnosing GGO-predominant-type lesions (1). The VBN system provides virtual images of the bronchial path to a peripheral lesion obtained from computed tomography (CT) digital imaging and communications in medicine (DICOM) data. In that study, we showed that VBN increased the diagnostic yield of GGO-predominant-type lesions from 57% to 69% by transbronchial biopsy (TBB) using EBUS-GS. Furthermore, in pure GGO lesions, the combination of VBN and EBUS-GS increased the diagnostic yield from 45% to 65%. We concluded in that study that addition of VBN to EBUS-GS can be more useful than EBUS-GS alone for diagnosing GGO predominant-type lesions.
Although peripheral GGO predominant-type lesions are difficult to diagnose by bronchoscopy, even with EBUS technique (3). Especially, in the case of pure GGO, the change in brightness on EBUS images was very delicate when the EBUS probe was in and out of the lesions (4,5). The use of VBN images makes it easier to identify such a faint change in an EBUS image. It is then possible to focus on the change in the EBUS image with simple movement of the EBUS probe (forward and backward), because the lesion may exist along with the target bronchus navigated in the virtual images.
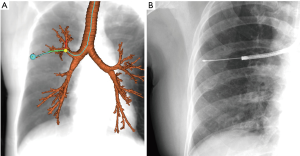
Moreover, the new VBN system (e.g., DirectPath™; Cybernet, Tokyo, Japan) can show virtual X-ray fluoroscopic images obtained from CT DICOM data. The target lesion is also indicated in the image, even if the lesion is not visible under X-ray fluoroscopy. These images may have advantages over X-ray fluoroscopic images for leading an EBUS probe to GGO-predominant-type lesions (Figure 1). A similar function is included in other navigation systems for bronchoscopes (SuperDimension™, Covidien, Plymouth, MN, USA; LungPoint™, Broncus Technologies, Inc., Mountain View, CA, USA; SYNAPSE VINCENT™, Fujifilm Corp, Tokyo, Japan).
As Dr. Chaves mentioned, tissue sampling from GGO lesions is another problem that complicates diagnosis (3). I agree with their opinion that sampling a large specimen using a large forceps or cryobiopsy might have advantages for diagnosis of GGO lesions. Prospective studies would be useful for evaluating such new technologies.
Acknowledgements
None.
Footnote
Conflicts of Interest: The author has no conflicts of interest to declare.
References
- Ikezawa Y, Shinagawa N, Sukoh N, et al. Usefulness of EBUS-GS and virtual bronchoscopic navigation for ground-glass opacity lesions. Ann Thorac Surg 2017;103:470-5. [Crossref] [PubMed]
- Ikezawa Y, Sukoh N, Shinagawa N, et al. Endobronchial ultrasonography with a guide sheath for pure or mixed ground-glass opacity lesions. Respiration 2014;88:137-43. [Crossref] [PubMed]
- Chavez C, Izumo T. The many facets of diagnostic bronchoscopy for pulmonary ground glass nodules. J Thorac Dis 2017;9:501-3. [Crossref] [PubMed]
- Sukoh N, Shinagawa N, Ikezawa Y, et al. Characteristics of endobronchial ultrasonographic (EBUS) images in three cases with ground glass opacity (GGO) predominant-type peripheral pulmonary lesions (PPLs). J Jpn Soc Resp Endoscopy 2014;36:298-303.
- Izumo T, Sasada S, Chavez C, et al. Radial endobronchial ultrasound images for ground-glass opacity pulmonary lesions. Eur Respir J 2015;45:1661-8. [Crossref] [PubMed]


