Deep sternal wound infection after cardiac surgery in the Chinese population: a single-centre 15-year retrospective study
Introduction
Median sternotomy has been the most frequently used incision for cardiac surgery since its introduction in 1956 (1). One of the life-threatening complications that occurs in patients following cardiovascular surgery through median sternotomy is deep sternal wound infection (DSWI). The incidence of DSWI that has been reported ranges from 0.2% to 8% (2,3). However, the mortality varies from 8% to 45%. Additionally, DSWI is associated with increased medical cost, prolonged hospital stays and even reoperation (4-6). Therefore, precautionary intervention before cardiac surgery and effective treatment after the occurrence of DSWI are significant.
Previous studies have attempted to determine risk factors of DSWI. However, a consensus on the significant risk factors of DSWI has not been reached. The identified risk factors include obesity, diabetes mellitus, tracheostomy, use of the bilateral mammary arteries, reoperation, transfusion, and prolonged operation time (6,7). Patients who suffer from DSWI is divided into three types according to time between operation and onset of DSWI, each of type has different pathogenic bacteria. Staphylococcus was the most common pathogenic bacterium in DSWI patients (8).
Although studies of DSWI have been reported for many years, little had been shown about DSWI in the Chinese population. The present study was designed to investigate the clinical characteristic of DSWI in patients who underwent cardiac surgery at our institution in order to conduct timely effective intervention.
Methods
Study design
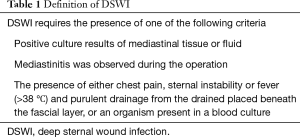
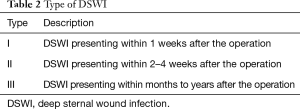
A retrospective study was performed at the department of cardiothoracic surgery at the Drum Tower Hospital that is affiliated with the medical school of Nanjing University. Consecutive patients who underwent cardiac surgery via median sternotomy during 1 January 2002 and 31 December 2016 were included. All patients were Chinese. The patients were diagnosed with DSWI by an attending physician and an infection control physician during their hospital stay and readmission period based on the definition of DSWI (Table 1) (9,10). The time interval between the operation and the date of diagnosis was obtained to determine the type of DSWI (11) (Table 2). We have treated these DSWI patients 15 years ago and use old diagnoses criteria at that time. In order to ensure the validity and consistency of data, we select the old definition. So, patients who suffer from sternal wound infection between one week after operation are excluded.
Full table
Full table
Patient selection
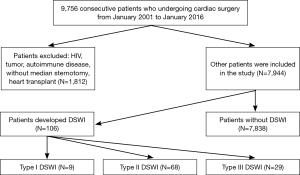
As follow chart showed, the study group did not include patients who underwent heart transplantation operations (Figure 1). Patients who suffered preoperative infection were divided into two types: patients who suffered from a simple bacterial infection were included into the study after antibiotic treatment (pneumonia, infective endocarditis and urinary tract infection); and patients who suffered from immune diseases were excluded from the study (HIV, tumour and autoimmune diseases). To confirm the diagnosis of DSWI, the group reviewed the database and collected relevant information regarding the patients, including their clinical records and laboratory examination results. Control patients were selected by the study group among eligible patients without evidence of DSWI or superficial wound infection. Patients who had delayed sternal closure after cardiac surgery were excluded from both the case and control patient groups.
Operation procedure
Antibiotic prophylaxis was used in all patients; cefuroxime was most commonly used, starting 30 minutes before the operation until 72 hours after surgery. The interlocked figure of “8” wire closure technique was generally used in patients who underwent cardiac surgery through a median sternotomy. However, if patients had an osteoporotic sternum, the Robicsek technique was adopted. Establishment of cardiopulmonary bypass (CPB) involved the vena cava and aorta or vena cava, axillary artery and femoral artery. All surgeries were performed by four experienced surgeons at the institution.
Treatment of DSWI
Treatment of DSWI included antibiotics, sternal debridement and flap reconstruction. Cefuroxime was the most commonly used agent. However, if patients were allergic to cefuroxime or culture MASA after the operation, cefuroxime was replaced by vancomycin. Tienam was added to the antibiotic treatment in patients with complicated respiratory diseases. The pectoral muscle flap was the most commonly used material for flap reconstruction. Extensive wound debridement was the first step of flap reconstruction, which involved resecting the necrotic tissue and sternum. Then, the tissue defect caused by the resection was closed by the transposition of the pectoralis major flap. In patients who only suffered from a minor tissue defect, iodine irrigation was performed instead.
Statistical analysis
Comparisons of the categorical variables were performed using the chi-square test. Comparisons of the continuous variables were performed by one-way ANOVA. The multiple logistic regression was used to identify the most significant mortality predictors. After the univariate analysis, risk factors with a P value <0.1 were selected for the multivariate model. Statistical significance was assessed at α=0.05. All analyses were performed by the SPSS version 17 software.
Results
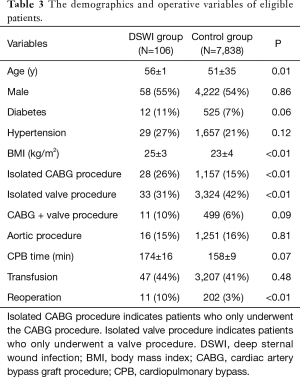
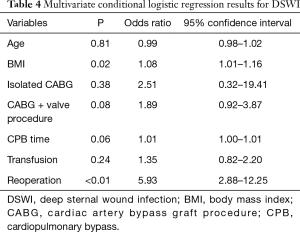
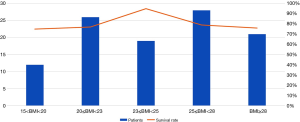
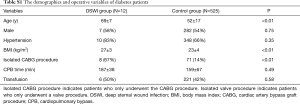
Table 3 shows the patient characteristics and operation data. There were 7,944 patients included in the study between January 2002 and December 2016, among whom 106 patients met the criteria of DSWI, and 7,838 patients were included as control patients. Several variables were different between the case patients and the control patients, including age (P=0.01), diabetes (P=0.06), body mass index (BMI) (P<0.01), isolated cardiac artery bypass graft procedure (CABG) (P<0.01), isolated valve procedure (P<0.01), CPB time (P=0.07) and reoperation (P<0.01). Then, we conducted a multiple logistic regression analysis that included age, BMI, CABG, CABG with valve surgery, CPB time, transfusion and reoperation as risk factors. The results are summarized in Table 4. BMI (OR=1.08; P=0.02;95% CI: 1.01–1.16) and reoperation (OR=5.93; P<0.01;95% CI: 2.88–12.25) were identified as significant risk factors for DSWI. In particular, patients who suffered from reoperation were five times as likely to have DSWI compared with patients who did not.-Although BMI is not a risk factor of DSWI, we observed that the association of BMI and outcomes is inverted “V” shape (Figure S1).
Full table
Full table
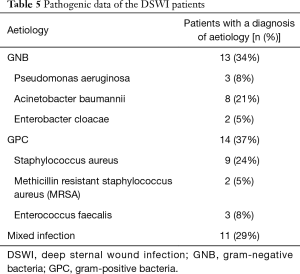
All patients who were suspected of having DSWI or had symptoms of DSWI underwent a blood culture and an exudation culture. It is worth noting that the overall number of positive bacterial culture was observed in only 38 out of 106 patients (35.85%). We identified that the most common bacteria that were isolated from the wound were staphylococcus aureus (n=9, 23.68%) and Acinetobacter baumannii (n=8, 21.05%) in patients diagnosed DSWI, as shown in Table 5. The positive rate of gram-positive organisms (n=14, 36.84%) was comparable with the positive rate of gram-negative organisms (n=13, 34.21%). In addition, there was mixed infection in patients with DSWI (n=11, 28.95%).
Full table
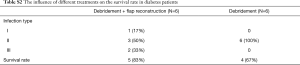
Based in the time interval between the operation and the date of DSWI diagnosis, patients in the DSWI group were divided into three types of DSWI, as summarized in Table 6. Patients who were diagnosed as type III exhibited a significant difference between the two treatment groups (P=0.01). But, we do not observed difference in diabetes patients (Tables S1-S3). Compared with antibiotic treatment and debridement, which were widely used in patients with DSWI, flap reconstruction was reported as an effective treatment in those patients. Hence, we analysed the survival rate of patients who were treated with antibiotics, debridement and flap reconstruction. As showed in Table 6, the latter group had an obviously better prognosis than the former group. It may be worth indicating that timely surgical intervention was better than conservative treatment in patients with DSWI, especially in patients who were diagnosed as type III DSWI (P=0.01).

Full table
Full table
Full table

Full table
Discussion
In the present study, we conducted a retrospective study on patients who underwent a cardiac operation in the past 15 years. To our knowledge, this is the largest retrospective study about DSWI in the Chinese population. Recently, some definition of criteria of DSWI have changed. In order to ensure the validity and consistency of data, we select the old definition. But new definition of DSWI is more suitable to current clinic status (10). The investigation provided an overall evaluation of DSWI after cardiac surgery in the Chinese population. Robinson et al reported that the incidence of DSWI was 1.3% in 12,000 patients who underwent cardiac surgery from July 2001 to June 2005 (6). We found that the incidence of DSWI is 1.33% and is comparable with the report above. However, considering that there were case patients who were not readmitted to the institution, the occurrence of DSWI may have been underestimated. Improvements in aseptic technique and the prevention of antibiotic use may contribute to a reduction in the incidence of DSWI after cardiac surgery. Some studies have reported that antibiotic prophylaxis was beneficial for reducing the incidence of DSWI after the operation (12-15).
The occurrence of DSWI has multifactorial causes. Floros et al. determined that the risk factors for DSWI consisted of smoking, re-exploration, oral hypoglycemic drug, emergency surgery, obesity, IABP and transfusion (2). In addition, Pilarczyk et al. identified that percutaneous dilatational tracheotomy within 48 hours after cardiac surgery was associated with mediastinitis (16). Our study identified that the potential risk factors for DSWI were BMI and reoperation. Although it was not identified as a significant risk factor, age was a significant variable between case patients and control patients, as the study group was older than the control group. Patients who have higher BMI are in danger of sternal instability. Therefore, sternal instability may contribute to the development of DSWI in elderly patients who received cardiac surgery via a median sternotomy.
Furthermore, our results presented that reoperation was a risk factor for DSWI after operation and that CPB time has a trend of difference (P=0.06). It was a little different from other studies that have been published (17-21), which have reported that operation time but not CPB time was a risk factor for DSWI. Prolonged CPB time may be associated with complex procedures and more surgical implants; patients who undergo reoperation often suffer a worse tissue situation and need more time, usually because of bleeding or unstable haemodynamics. These situations probably significantly increase DSWI risk, but an additional randomized control trial is needed to verify the conjecture (2,20,22,23). Although transfusion rates were not significantly different in our study, there was a trend of difference. Whether there are other factors involved in DSWI in patients included in our study population need further investigation.
Pathogenic microorganisms were confirmed with exudation culture. The low rate of positive results may be attributed to: (I) the selection pressure of antibiotic prophylaxis, as broad spectrum antibiotic is routinely used before cardiac operation at present, which may result in a negative result from blood culture and exudation culture; (II) aetiology of DSWI was atypical pathogens (mycoplasma, anaerobic bacteria), which are difficult to culture in vitro; (III) there were some DSWI patients who underwent sternal dehiscence without infection; and (IV) antibiotic abuse is still a complicated problem in the treatment of infection in the Chinese population. The most common bacterium was staphylococcus aureus, which was in agreement with a previous study. However, the proportion of staphylococcus aureus varied from previous reports (2,8,21,24,25). Some studies have attempted to investigate the benefit of antibiotic prophylaxis and confirm that intervention strategies were efficient (12,13,22,26).
For the treatment of DSWI, it is thought that debridement was the most effective treatment after a timely diagnosis, and the use of antibiotics targeting the pathogenic bacterium was better than dilute povidone-iodine irrigation for the treatment of DSWI (23,27). Some studies have reported that an antibiotic-collagen sponge was effective for the prevention of DSWI. However, the results from different studies have been controversial (12,13,28,29). In this study, we showed that the group treated with intravenous antibiotic, sternal debridement and flap reconstruction had a better prognosis than the group treated with intravenous antibiotic and sternal debridement (30-33). Negative pressure wound therapy system is also used in the treatment of DSWI patients. But, due to this treatment equipment is applied in our department recently, not of all patients received this new therapy system. So, the influence of negative pressure wound therapy system on DSWI patients remain to be further study. The periods are not consecutive. Someone with an infection at 10 days is not included in either type I or type II. It is noteworthy that the proportion of type III DSWI patients are significantly different between the two groups. Considering this, we assumed that the type of DSWI may a considerable factor that affects the results of treatment. In died patients, time to death after diagnosis of infection is respectively 55±14 and 34±3 days in debridement and flap reconstruction group and debridement group. So, if they died before they were well enough to get a flap reconstruction included in the debridement group, there, there exist potential bias. Overall, the results indicate that timely surgical intervention is beneficial for patients with DSWI (23).
Although the findings were statistically supported with a large sample size, there were some limitations that may have affect the findings. First, this is a retrospective study, which cannot account for the effect of unknown variables. In addition, the low event incidence, such as risk factors and bacteriological characteristics, precluded us from further investigation about the details of DSWI. Furthermore, the positive rate of pathogenic bacteria was low and may have affected the result. Therefore, a prospective randomized controlled trial should be implemented to analyse the characteristics of DSWI in the Chinese population.
Conclusions
In this retrospective study of DSWI in the Chinese population, we determined the incidence of DSWI in patients who underwent cardiac surgery via median sternotomy and the pathogenic characteristics of the bacteria. DSWI was associated with several risk factors, including BMI and reoperation. Additionally, flap reconstruction is a valid treatment for patients with DSWI, especially for patients with type III DSWI. Effective intervention strategies could improve the outcome of patients undergoing cardiac surgery
Acknowledgements
Funding: This work was supported by the Fundamental Research Funds for the Central Universities (No. 021414380190).
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The study was approved by the institutional ethics board of Nanjing Drum Tower Hospital (No. 2017-090-01).
References
- Peivandi AA, Kasper-Konig W, Quinkenstein E, et al. Risk factors influencing the outcome after surgical treatment of complicated deep sternal wound complications. Cardiovasc Surg 2003;11:207-12. [Crossref] [PubMed]
- Floros P, Sawhney R, Vrtik M, et al. Risk factors and management approach for deep sternal wound infection after cardiac surgery at a tertiary medical centre. Heart Lung Circ 2011;20:712-7. [Crossref] [PubMed]
- Schimmer C, Sommer SP, Bensch M, et al. Management of poststernotomy mediastinitis: experience and results of different therapy modalities. Thorac Cardiovasc Surg 2008;56:200-4. [Crossref] [PubMed]
- Sjögren J, Nilsson J, Gustafsson R, et al. The impact of vacuum-assisted closure on long-term survival after post-sternotomy mediastinitis. Ann Thorac Surg 2005;80:1270-5. [Crossref] [PubMed]
- Kubota H, Miyata H, Motomura N, et al. Deep sternal wound infection after cardiac surgery. J Cardiothorac Surg 2013;8:132. [Crossref] [PubMed]
- Robinson PJ, Billah B, Leder K, et al. Factors associated with deep sternal wound infection and haemorrhage following cardiac surgery in Victoria. Interact Cardiovasc Thorac Surg 2007;6:167-71. [Crossref] [PubMed]
- Lu JC, Grayson AD, Jha P, et al. Risk factors for sternal wound infection and mid-term survival following coronary artery bypass surgery. Eur J Cardiothorac Surg 2003;23:943-9. [Crossref] [PubMed]
- Gårdlund B, Bitkover CY, Vaage J. Postoperative mediastinitis in cardiac surgery - microbiology and pathogenesis. Eur J Cardiothorac Surg 2002;21:825-30. [Crossref] [PubMed]
- Garner JS, Jarvis WR, Emori TG, et al. CDC definitions for nosocomial infections, 1988. Am J Infect Control 1988;16:128-40. [Crossref] [PubMed]
- Berríos-Torres SI, Umscheid CA, Bratzler DW, et al. Centers for disease control and prevention guideline for the prevention of surgical site infection, 2017. JAMA Surg 2017. [Epub ahead of print]. [Crossref] [PubMed]
- Pairolero PC, Arnold PG. Management of infected median sternotomy wounds. Ann Thorac Surg 1986;42:1-2. [Crossref] [PubMed]
- Kępa K, Krzych L, Krejca M. Gentamicin-containing collagen implant reduces sternal wound complications after cardiac surgery: a retrospective analysis. Int J Surg 2015;13:198-206. [Crossref] [PubMed]
- Kowalewski M, Pawliszak W, Zaborowska K, et al. Gentamicin-collagen sponge reduces the risk of sternal wound infections after heart surgery: Meta-analysis. J Thorac Cardiovasc Surg 2015;149:1631-40.e1-6.
- Osawa H, Yoshii S, Abraham SJ, et al. Topical spraying of cefazolin and gentamicin reduces deep sternal wound infections after heart surgery: a multicenter, large volume, retrospective study. Gen Thorac Cardiovasc Surg 2016;64:197-202. [Crossref] [PubMed]
- Raja SG, Salhiyyah K, Rafiq MU, et al. Impact of gentamicin-collagen sponge (Collatamp) on the incidence of sternal wound infection in high-risk cardiac surgery patients: a propensity score analysis. Heart Surg Forum 2012;15:E257-61. [Crossref] [PubMed]
- Pilarczyk K, Marggraf G, Dudasova M, et al. Tracheostomy after cardiac surgery with median sternotomy and risk of deep sternal wound infections: Is It a Matter of Timing? J Cardiothorac Vasc Anesth 2015;29:1573-81. [Crossref] [PubMed]
- Al-Zaru IM, Ammouri AA, Al-Hassan MA, et al. Risk factors for deep sternal wound infections after cardiac surgery in Jordan. J Clin Nurs 2010;19:1873-81. [Crossref] [PubMed]
- Parisian Mediastinitis Study Group. Risk factors for deep sternal wound infection after sternotomy: a prospective, multicenter study. J Thorac Cardiovasc Surg 1996;111:1200-7. [Crossref] [PubMed]
- Miyahara K, Matsuura A, Takemura H, et al. Implementation of bundled interventions greatly decreases deep sternal wound infection following cardiovascular surgery. J Thorac Cardiovasc Surg 2014;148:2381-8. [Crossref] [PubMed]
- Trick WE, Scheckler WE, Tokars JI, et al. Modifiable risk factors associated with deep sternal site infection after coronary artery bypass grafting. J Thorac Cardiovasc Surg 2000;119:108-14. [Crossref] [PubMed]
- Yumun G, Erdolu B, Toktas F, et al. Deep sternal wound infection after coronary artery bypass surgery: management and risk factor analysis for mortality. Heart Surg Forum 2014;17:E212-6. [Crossref] [PubMed]
- Schersten H. Modified prophylaxis for preventing deep sternal wound infection after cardiac surgery. Apmis 2007;115:1025-8. [Crossref] [PubMed]
- Wu L, Chung KC, Waljee JF, et al. A national study of the impact of initial debridement timing on outcomes for patients with deep sternal wound infection. Plast Reconstr Surg 2016;137:414e-23e. [Crossref] [PubMed]
- Lu JC. Risk factors for sternal wound infection and mid-term survival following coronary artery bypass surgery. Eur J Cardiothorac Surg 2003;23:943-9. [Crossref] [PubMed]
- Ben-Ami E, Levy I, Katz J, et al. Risk factors for sternal wound infection in children undergoing cardiac surgery: a case-control study. J Hosp Infect 2008;70:335-40. [Crossref] [PubMed]
- Schweizer ML, Chiang HY, Septimus E, et al. Association of a bundled intervention with surgical site infections among patients undergoing cardiac, hip, or knee surgery. JAMA 2015;313:2162-71. [Crossref] [PubMed]
- Lazar HL, Salm TV, Engelman R, et al. Prevention and management of sternal wound infections. J Thorac Cardiovasc Surg 2016;152:962-72. [Crossref] [PubMed]
- Schimmer C, Ozkur M, Sinha B, et al. Gentamicin-collagen sponge reduces sternal wound complications after heart surgery: a controlled, prospectively randomized, double-blind study. J Thorac Cardiovasc Surg 2012;143:194-200. [Crossref] [PubMed]
- Bennett-Guerrero E, Ferguson TB Jr, Lin M, et al. Effect of an implantable gentamicin-collagen sponge on sternal wound infections following cardiac surgery: a randomized trial. JAMA 2010;304:755-62. [Crossref] [PubMed]
- Immer FF, Durrer M, Muhlemann KS, et al. Deep sternal wound infection after cardiac surgery: modality of treatment and outcome. Ann Thorac Surg 2005;80:957-61. [Crossref] [PubMed]
- Eifert S, Kronschnabl S, Kaczmarek I, et al. Omental flap for recurrent deep sternal wound infection and mediastinitis after cardiac surgery. Thorac Cardiovasc Surg 2007;55:371-4. [Crossref] [PubMed]
- Kobayashi T, Mikamo A, Kurazumi H, et al. Secondary omental and pectoralis major double flap reconstruction following aggressive sternectomy for deep sternal wound infections after cardiac surgery. J Cardiothorac Surg 2011;6:56. [Crossref] [PubMed]
- Liu D, Wang W, Cai A, et al. Analysis of surgical treatment with pectoralis major muscle flap for deep sternal infection after cardiac surgery: a case series of 189 patients. Zhonghua Wai Ke Za Zhi 2015;53:193-6. [PubMed]