A rare large tracheal glomus tumor with postoperative haematemesis
Glomus tumors are rare, benign but often painful tumors arising from modified smooth muscle cells (SMCs) of the glomus body, generally much less than 1 cm in diameter. These tumors are usually found in the distal portion of the digits, especially under the fingernails. They are morphologically characterized by round, slightly elevated, red-blue, firm nodules (1). However, these tumors can also occur occasionally at sites such as the chest wall, bone, gastrointestinal tract, nerve, eyelid, mediastinum, and trachea, where normal glomus bodies may be few or even absent (2). We reported a rare tracheal glomus tumor which was successfully resected.
Case report
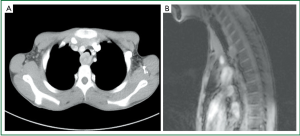
A 15-year-old boy was admitted to our hospital for a 3-month history of cough, hemoptysis and intermittent shortness of breath, without any past medical and smoking history. Physical examination was negative except for dry rales of trachea in auscultation. Radiological examinations revealed a mass at the posterior wall of thoracic trachea, with its size of approximately 2.0 cm × 2.3 cm (Figure 1).
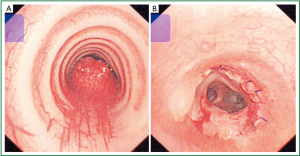
The operation was performed via right posterolateral thoracotomy through the fourth intercostal space. During the operation, a mass with a base about 2.0 cm in diameter was found to be located at the posterior tracheal wall and no pleural adhesion or effusion was found. En bloc resection of the tumor was achieved with 0.5 cm spare of both surgical margins. The tumor was taken out and measured. Maximal and minimal diameter was 2.5 and 2.0 cm respectively. Frozen-section pathological examination confirmed a benign tumor with negative resection margins. Then, tracheal anastomosis was performed by continuous suture using 3-0 prolene stitches. Postoperative bronchoscopy showed that the trachea was successfully anastomosed with no stricture or bleeding (Figure 2).
The tumor was pathologically diagnosed as glomus tumor. The patient’s symptoms were relieved and was discharged 11 days after surgery without any main complication.
Three hours later, the boy was sent to the emergency room (ER) with severe hemoptysis, or probably, haematemesis. He was attacked by cardiac arrest and was fortunately resuscitated by CPR. Lots of fresh blood was sucked out via endotracheal suction. Anastomotic bleeding came up as the first diagnosis. An emergency exploratory thoracotomy through the original incision was performed immediately. There was about 400 mL pleural effusion in the right chest, but no active bleeding was found, intraoperative bronchoscopy did not find any bleeding site in the anastomotic stoma either. Then upper gastrointestinal hemorrhage came in to consideration, and intraoperative gastroscopy was assigned. It found plenty of blood and blood clots in the stomach but further exploration was restrained because of poor imaging field. Thus, the patient was treated by hypervolemic therapy, hemostasis therapy with somatostatin and Carbazochrome Sodium Sulfonate, gastrointestinal decompression, anti-infection therapy and nutrition support. Postoperative enhanced abdominal CT scan with vascular reconstruction showed nothing abnormal. Another gastroscopy 2 weeks later found nothing special either. The patient finally recovered and was discharged 3 weeks after surgery. The symptoms disappeared, and no sign of postoperative stenosis was found at the patient’s 1-year follow up, neither was recurrence or hemorrhage.
Discussion
Glomus tumors are biologically benign but often painful tumors arising from modified SMCs of the glomus body, histologically, these tumors are aggregates, nests, and masses of specialized glomus cells associated with branching vascular channels, all surrounded by connective tissue matrix.
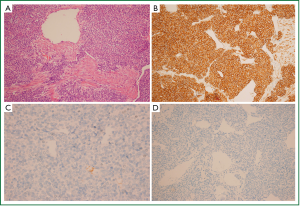
In the sections of the tumor, plenty of small round or oval cells, vessels and smooth muscle were seen by microscope. Immunohistochemistry stain supported the diagnosis of glomus tumor (Figure 3).
Surgical removal of the tumor with primary reconstruction of trachea was usually the first choice for treatment (3). Successful removal via flexible bronchoscope has been reported (4), but in their case, the tumor was 2.0 cm × 1.0 cm in size and there seemed to be no tight adhesion with tissue surrounding though it locates at the lower tracheal segment. Cervical collar incision has also been reported recently (5), and in their case, the tumor was 1.3 cm × 1.2 cm in size, located at the upper portion of the trachea. On the other hand, posterolateral thoracotomy, instead of bronchoscope, was performed on our patient because the tumor located at the lower portion of trachea, had a relatively large size, the base of the tumor was wide and risk of severe bleeding was high.
To our knowledge, this is the first report of postoperative severe hemorrhage of upper digestive tract after removal of tracheal glomus tumor. However, the reason that caused the severe hemorrhage after the first surgery remains unclear.
Glomus tumor of the stomach has been reported (6), as well as multiple lesions (7). With regard to our case, nothing abnormal was found through radiological and endoscopic examinations. Therefore, we made two hypotheses as following: first, the patient simultaneously suffered from another mini glomus tumor, which caused severe hemorrhage but could hardly be detected by CT scan or gastroscopy; second, the patient suffered from severe stress ulcer due to the surgery and the ulcer had been cured when postoperative gastroscopy was performed. When we reviewed the treatment strategies, the second thoracotomy seemed to be unnecessary since it only played a role in excluding problems of anastomotic stoma, which could be manifested by bronchoscopy, a simpler and less invasive test. If we chose to apply the bronchoscopy to check whether the anastomotic bleeding existed at the beginning, the second thoracotomy could be avoided.
Conclusions
Glomus tumor is rare benign tumor derived from soft tissue with good long-term prognosis (8). While coping with patients with tracheal glomus tumor, potential multiple lesions should be intentionally evaluated. Tracheal resection via thoracotomy should be taken in order to remove the tumor of lower portion of the trachea or with a relatively large size (maximum diameter >2.0 cm) safely and integrallty. In addition, the misdiagnosis of the case reminds us to confirm the anastomotic bleeding carefully as long as the situation is not extremely urgent so that unnecessary invasive procedures can be avoided.
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- Weiss SW, Goldblum JR. Perivascular tumors. In: Weiss SW. eds. Enzinger and Weiss’s soft tissue tumors. 4th ed. St. Louis: Mosby Inc, 2001:985-93.
- Kumar V, Abbas AK, Fausto N, et al. eds. Robbins basic pathology, 8th ed. Elsevier, 2007.
- Schiefer TK, Parker WL, Anakwenze OA, et al. Extradigital glomus tumors: a 20-year experience. Mayo Clin Proc 2006;81:1337-44. [PubMed]
- Shang Y, Huang Y, Huang HD, et al. Removal of glomus tumor in the lower tracheal segment with a flexible bronchoscope: report of two cases. Intern Med 2010;49:865-9. [PubMed]
- Baek SH, Huh DM, Park JH, et al. Glomangiomyoma of the trachea. Korean J Thorac Cardiovasc Surg 2011;44:440-3. [PubMed]
- Wang LM, Chetty R. Selected unusual tumors of the stomach: a review. Int J Surg Pathol 2012;20:5-14. [PubMed]
- Freire M, Rubin B, Lietman S, et al. Solitary glomus tumor recurring as multiple glomus tumors. Skeletal Radiol 2012;41:1333-7. [PubMed]
- Gowan RT, Shamji FM, Perkins DG, et al. Glomus tumor of the trachea. Ann Thorac Surg 2001;72:598-600. [PubMed]


