Gender and cardiovascular impact of obstructive sleep apnea: work in progress!
In the last decades, obstructive sleep apnea (OSA) has gained substantial attention due to the high prevalence and multiple consequences not limited to sleep quality and quality of life (1). Particularly, the cardiovascular impact of OSA has been consistently suggested by multiple, basic (2), translational (2) and clinical studies (3-10). However, because OSA is at least twice more common in men than in women (11) much of this evidence comprised basically only men or a small proportion of women that prevented us to have substantial data stratified by sex. However, considering the current burden of OSA (12), the amount of women with significant OSA is by far relevant. Therefore, there is an obvious interest in exploring whether the cardiovascular impact of OSA is potentially true regardless of gender. This notion has been extensively explored in other cardiovascular research areas, and not surprisingly has been recently addressed in the sleep medicine field.
One of the examples of sex-related impact of OSA on cardiovascular diseases came out from the Victoria Sleep Cohort study (13), an adult cohort designed to assess the prevalence and natural history of OSA in residents of Vitoria-Gasteiz, Spain. In this study, Cano-Pumarega and colleagues explored the association of untreated OSA and incident stage 2 hypertension (blood pressure ≥160/100 mmHg) based on gender differences in 1,155 normotensive subjects (650 of them women, 56%) at baseline. The presence of moderate to severe OSA was higher in men than in women (18.6% vs. 8.6%). After a mean follow-up of 7.5 years, the authors found that 23% of the hypertensive patients developed stage 2 hypertension and they found a significant difference between men and women (13.7% vs. 3.2%, P<0.001). A respiratory disturbance index (RDI) ≥14/h (comprising moderate and severe OSA) was independently associated with incident stage 2 hypertension in men (OR 2.54, 95% CI: 1.09‡5.95) but not in women. Interestingly, no significant association was observed in the baseline RDI between the subjects who developed stage 1 hypertension and the subjects who remained normotensive.
How to interpret these provocative and interesting prospective findings? Are women really protected from the cardiovascular effects of OSA, including clinical, relevant hypertension? Or the relative small sample of moderate to severe OSA women (n=48) may prevent us any definitive conclusion? Supporting the last, the OR for women with OSA to develop stage 2 hypertension was not so different from men (2.14, 95% CI: 0.40–11.36).
Putting the Victoria Sleep Cohort in context (Table 1), the next question is: how consistent are these results in comparison to recent evidence addressing surrogate markers, intermediary pathways and cardiovascular events in women with OSA? As described on Table 1, there are more questions than answers regarding this important research area. However, it is important to note that the majority of the evidence suggests that the presence of OSA in women were associated with significant impairment in arterial stiffness, coronary calcium, and higher cardiovascular risk (Table 1). Some of these studies pointed to the opposite direction: only women with OSA but not men are on risk! For instance, Faulx et al. found that the impact of OSA on endothelial function was only significant in women (16).
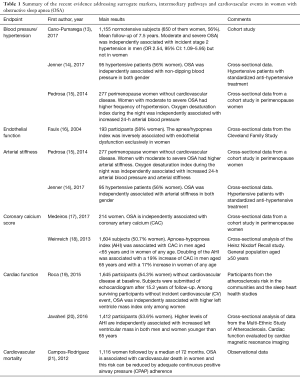
Full table
So, what is the take-home message so far: work in progress (22)! Particularly, future investigations addressing several endpoints with significant amount of women and men with similar OSA severity may help to clarify whether the apparently differences in women and men with OSA is justified by differences in frequency and severity of OSA. In addition, intervention studies addressing the effects of OSA treatment is highly desired. For instance, a recent randomized controlled trial investigation addressed the effects of CPAP or conservative treatment for 12 weeks on blood pressure levels and the glucose and lipid profile in 307 women with moderate-to-severe OSA. Compared with the control group, the CPAP group achieved a significantly greater decrease in diastolic blood pressure (−2.04 mmHg), and a non-significant greater decrease in systolic blood pressure (−1.54 mmHg) and mean blood pressure (−1.90 mmHg). CPAP therapy did not change any of the metabolic variables assessed (23). New studies with direct comparisons of men and women are warranted. Finally, despite the recent neutral results of OSA treatment in the second prevention scenario of coronary artery disease and stroke (24), there is still too much to respond in the primary prevention and in patients with established cardiovascular diseases.
Acknowledgements
Funding: Dr. Drager is supported by a research fellowship Grant (2012/02953-2) from Fundação de Amparo à Pesquisa do Estado de São Paulo (FAPESP) and Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq).
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Jordan AS, McSharry DG, Malhotra A. Adult obstructive sleep apnoea. Lancet 2014;383:736-47. [Crossref] [PubMed]
- Drager LF, Polotsky VY, O'Donnell CP, et al. Translational approaches to understanding metabolic dysfunction and cardiovascular consequences of obstructive sleep apnea. Am J Physiol Heart Circ Physiol 2015;309:H1101-11. [Crossref] [PubMed]
- Yaggi HK, Concato J, Kernan WN, et al. Obstructive sleep apnea as a risk factor for stroke and death. N Engl J Med 2005;353:2034-41. [Crossref] [PubMed]
- Marin JM, Carrizo SJ, Vicente E, et al. Long-term cardiovascular outcomes in men with obstructive sleep apnoea-hypopnoea with or without treatment with continuous positive airway pressure: an observational study. Lancet 2005;365:1046-53. [Crossref] [PubMed]
- Valham F, Mooe T, Rabben T, et al. Increased risk of stroke in patients with coronary artery disease and sleep apnea: a 10-year follow-up. Circulation 2008;118:955-60. [Crossref] [PubMed]
- Javaheri S, Caref EB, Chen E, et al. Sleep apnea testing and outcomes in a large cohort of Medicare beneficiaries with newly diagnosed heart failure. Am J Respir Crit Care Med 2011;183:539-46. [Crossref] [PubMed]
- Maia FC, Goulart AC, Drager LF, et al. Impact of High Risk for Obstructive Sleep Apnea on Survival after Acute Coronary Syndrome: Insights from the ERICO Registry. Arq Bras Cardiol 2017;108:31-7. [PubMed]
- Uchôa CHG, Danzi-Soares NJ, Nunes FS, et al. Impact of OSA on cardiovascular events after coronary artery bypass surgery. Chest 2015;147:1352-60. [Crossref] [PubMed]
- Lee CH, Sethi R, Li R, et al. Obstructive Sleep Apnea and Cardiovascular Events After Percutaneous Coronary Intervention. Circulation 2016;133:2008-17. [Crossref] [PubMed]
- Uchôa CHG, Pedrosa RP, Javaheri S, et al. OSA and Prognosis After Acute Cardiogenic Pulmonary Edema: The OSA-CARE Study. Chest 2017. [Epub ahead of print]. [Crossref] [PubMed]
- Young T, Palta M, Dempsey J, et al. The occurrence of sleep-disordered breathing among middle-aged adults. N Engl J Med 1993;328:1230-5. [Crossref] [PubMed]
- Heinzer R, Vat S, Marques-Vidal P, et al. Prevalence of sleep-disordered breathing in the general population: the HypnoLaus study. Lancet Respir Med 2015;3:310-8. [Crossref] [PubMed]
- Cano-Pumarega I, Barbé F, Esteban A, et al. Sleep Apnea and Hypertension: Are There Sex Differences? The Vitoria Sleep Cohort. Chest 2017;152:742-50. [Crossref] [PubMed]
- Jenner R, Fatureto-Borges F, Costa-Hong V, et al. Association of obstructive sleep apnea with arterial stiffness and nondipping blood pressure in patients with hypertension. J Clin Hypertens (Greenwich) 2017;19:910-8. [Crossref] [PubMed]
- Pedrosa RP, Barros IML, Drager LF, et al. OSA is common and independently associated with hypertension and increased arterial stiffness in consecutive perimenopausal women. Chest 2014;146:66-72. [Crossref] [PubMed]
- Faulx MD, Larkin EK, Hoit BD, et al. Sex influences endothelial function in sleep-disordered breathing. Sleep 2004;27:1113-20. [Crossref] [PubMed]
- Medeiros AK, Coutinho RQ, Barros IM, et al. Obstructive sleep apnea is independently associated with subclinical coronary atherosclerosis among middle-aged women. Sleep Breath 2017;21:77-83. [Crossref] [PubMed]
- Weinreich G, Wessendorf TE, Erdmann T, et al. Association of obstructive sleep apnoea with subclinical coronary atherosclerosis. Atherosclerosis 2013;231:191-7. [Crossref] [PubMed]
- Roca GQ, Redline S, Claggett B, et al. Sex-Specific Association of Sleep Apnea Severity With Subclinical Myocardial Injury, Ventricular Hypertrophy, and Heart Failure Risk in a Community-Dwelling Cohort: The Atherosclerosis Risk in Communities-Sleep Heart Health Study. Circulation 2015;132:1329-37. [Crossref] [PubMed]
- Javaheri S, Sharma RK, Wang R, et al. Association between Obstructive Sleep Apnea and Left Ventricular Structure by Age and Gender: the Multi-Ethnic Study of Atherosclerosis. Sleep 2016;39:523-9. [Crossref] [PubMed]
- Campos-Rodriguez F, Martinez-Garcia MA, de la Cruz-Moron I, et al. Cardiovascular mortality in women with obstructive sleep apnea with or without continuous positive airway pressure treatment: a cohort study. Ann Intern Med 2012;156:115-22. [Crossref] [PubMed]
- Jenner R, Lorenzi-Filho G, Drager LF. Cardiovascular impact of obstructive sleep apnea: does gender matter? Expert Rev Cardiovasc Ther 2014;12:281-3. [Crossref] [PubMed]
- Campos-Rodriguez F, Gonzalez-Martinez M, Sanchez-Armengol A, et al. Effect of continuous positive airway pressure on blood pressure and metabolic profile in women with sleep apnoea. Eur Respir J 2017.50. [PubMed]
- McEvoy RD, Antic NA, Heeley E, et al. CPAP for Prevention of Cardiovascular Events in Obstructive Sleep Apnea. N Engl J Med 2016;375:919-31. [Crossref] [PubMed]


