Chemotherapy treatment in malignant pleural mesothelioma: a difficult history
Introduction
Malignant pleural mesothelioma (MPM) is a rare neoplasm linked to asbestos exposure that typically arises from mesothelial surfaces of the pleural cavity. It is characterized by a poor prognosis, with a medium life-expectancy between 12 and 18 months after diagnosis (1). However, carefully selected patients with localized disease who receive multimodal treatment have relatively prolonged survival.
Males are 3.8 times more affected than females and have a worse survival rate (2,3). Moreover, two prognostic scoring systems published from EORTC and CALGB include pleural primary site, high serum level of LDH, poor ECOG performance status, high serum levels of platelets, non-epithelial histology and advanced age as independent predictors of poor outcome (4,5).
Notably, the global incidence and mortality of MPM is rising, primarily in developing countries, in which the incidence peak is predicted within 2025 (6). Thus, health and economic burden correlated to this disease is expected to increase.
The pathogenesis of MPM is multifactorial, though up to 80% of MPM cases is correlated to asbestos exposure due to occupational, para-occupational or environmental factors. However, the other 20% of patients does not report any exposure, suggesting that genetic predisposition could play a crucial role in MPM pathogenesis (6).
Symptoms are generally present only once extensive intrathoracic disease has developed, with dyspnea, pleural effusion and chest pain occurring in 60–70% of cases (6,7). Clinical suspicion may arise in the setting of respiratory symptoms associated with pleural thickening or effusion on chest imaging and a history of asbestos exposure. However, a pleural biopsy or at least a cytological examination is necessary to confirm the diagnosis (8).
Unfortunately, the outcome of MPM has not been substantially improved over the last decades and its treatment remains a critical challenge.
Several new drugs and potential molecular prognostic factors are under investigation in order to tailor treatment approaches and to improve the outcome of these patients.
Clinical management
Every patient should be initially evaluated by an expert multidisciplinary team and the following multidisciplinary treatment plan should be based upon the assessment of the extent of the disease, the patient’s general conditions (age, performance status, cardiopulmonary function, comorbidities) and their preferences for aggressive potentially curative or only palliative treatment (3).
To date, therapeutic options are represented by surgery, radiotherapy (RT) and chemotherapy (CT), differently combined in a multimodal approach.
Approximately, only 20% of patients are suitable for radical surgery, intended as macroscopic complete resection (R0 or R1), and more than 85% of them die within 5 years. The remaining 80% of patients will not be candidate for combined approach including definitive surgery; in these cases, CT remains the standard treatment option (9).
Patients with resectable disease
The role of definitive surgery for MPM is controversial. No prospective randomized clinical trial has yet established whether this approach leads to an improvement in survival. Moreover, both invasive extrapleural pneumonectomy (EPP) and, to a lesser extent, pleurectomy/decortication (P/D) are associated with substantial morbidity and mortality, though a better outcome has been observed when surgery was performed in centers with adequate expertise (10).
Additionally, the optimal procedure to be performed (EPP or P/D) is uncertain and there are no data from randomized trials comparing these two different approaches.
Local and distant recurrence rates after surgery are still high, leading to the development of new treatment strategies to evaluate adjuvant therapy in order to improve local control and particularly OS.
Several non-randomized studies have evaluated a trimodality treatment consisting of induction CT with active agents such as cisplatin and pemetrexed, followed by surgery and subsequent RT, with median OS ranging from 14 to 25.5 months (6). Krug et al. performed a multicenter phase II trial evaluating neoadjuvant cisplatin plus pemetrexed followed by EPP and adjuvant RT; the results of this trial showed a median survival of 17 months. However, the impact of a high selection of patients in these trials should not be underestimated (11).
Accordingly, the Mesothelioma and Radical Surgery (MARS) trial randomized 50 patients to EPP or no EPP in the setting of trimodal treatment (12). The authors demonstrated no survival or quality of life benefit deriving from EPP; on the contrary, patients in the no-EPP group had a better outcome compared to EPP-group (HR adjusted for prognostic variables 2.75). Additionally, Stahel et al. reported no differences in loco-regional relapse-free survival (RFS) between patients receiving hemithoracic RT after neoadjuvant CT and EPP compared with those receiving only observation (13). Nevertheless, carefully selected patients may benefit from multimodality approach.
Patients with unresectable disease: the mainstay role of CT
For patients who have unresectable disease and for those in which surgery is not feasible due to medical comorbidities or old age, CT and symptomatic treatment, including the management of pleural effusion, represent the gold-standard.
First-line single-agent CT
Since the 1980s, several phase II studies have evaluated the role of single-agent CT with anthracyclines, taxanes, platinum compounds, alkylating agents, and topoisomerase inhibitors in mesothelioma patients; however, these trials showed low response rates ranging from 0% to 13% (3,14-16). Tsao et al. reported single-agent response rates from 7% to 20% in patients treated with platinum analogues, antimetabolites (e.g., pemetrexed, raltitrexed, methotrexate), doxorubicin, vinorelbine, and gemcitabine (17).
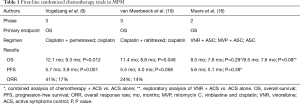
Furthermore, a randomized trial performed by Muers et al. has evaluated the impact of first-line CT on survival compared with active symptoms control alone (18). In this study, which has been the only one where CT has been directly compared with no active anti-cancer treatment, 409 patients with MPM were randomly assigned to symptomatic treatment, symptomatic treatment plus CT including cisplatin, vinblastine and mitomycin or to symptomatic treatment plus single-agent vinorelbine. The authors demonstrated a trend toward improved outcome only in the vinorelbine group compared with symptom control alone (HR 0.8, P=0.08; mOS 9.5 months) (Table 1).
Full table
First-line combination CT
To date, the combination CT with cisplatin plus pemetrexed represents the most widely used regimen for patients with unresectable MPM. The role of this regimen was initially assessed in a phase I trial where 11 patients were enrolled and were given pemetrexed combined with cisplatin, at increasing doses of both drugs.
The results of the trial showed that the combination was tolerable as well as active with five (45%) out of 11 patients experiencing a partial response (20). Subsequently, cisplatin plus pemetrexed was approved by FDA on the basis of the phase III EMPHACIS trial published by Vogelzang et al., that randomized 456 patients to cisplatin plus pemetrexed or cisplatin alone (9). The results showed a statistically significant prolongation of median OS (12.1 vs. 9.3 months, HR, 0.77), progression-free survival (PFS, 5.7 vs. 3.9 months) and overall response rate (ORR, 41% vs. 17%) in the combination arm (Table 1). Notably, patients who received folic acid plus vitamin B12 during CT showed the most striking differences in outcome, less toxicities and a greater number of administered cycles compared with patients not receiving supplementation.
In the EMPHACIS trial quality of life was also assessed through the LCSS-Meso questionnaire which had been previously validated in mesothelioma patients. The overall symptom score favored the combination arm after 6 cycles. Moreover, a statistically significant improvement in pain, cough and dyspnea was noted after 4 cycles in the pemetrexed plus cisplatin arm. Likewise, an improvement in global quality of life and fatigue was also observed in the combination arm (21).
The International Expanded Access Program (EAP) allowed more than 3,000 MPM patients to receive single-agent pemetrexed or pemetrexed in combination with cisplatin or carboplatin in 13 different countries. In the pemetrexed plus cisplatin arm a response rate of 26.3% was observed compared with 21.7% in the pemetrexed plus carboplatin arm. The 1-year survival rates were 63.1% versus 64.0%, respectively; median TTP was also similar (7 vs. 6.9 months) (22).
Additionally, a randomized EORTC phase III trial compared cisplatin 80 mg/mq plus the antimetabolite raltitrexed 3 mg/mq every 21 days to cisplatin alone (19). This first-line combination showed an improvement of both OS (mOS 11.4 vs. 8.8 months, P=0.04; 1 year-OS 46% vs. 40%, P=0.06) and PFS (5.3 vs. 4 months), with a magnitude of clinical benefit similar to that reached in the previous pemetrexed study (Table 1). A quality of life analysis was also performed in this trial showing no differences or deterioration of overall health status/QoL scale with the addition of raltitrexed to cisplatin.
However, currently there are no data to support a preference of pemetrexed vs. raltitrexed. A recent network metanalysis of these two randomized trials provided an indirect comparison between cisplatin-pemetrexed and cisplatin-raltitrexed. The authors found no significant difference in OS, ORR and safety between the two regimens, suggesting a comparable efficacy.
Thus, the clinical choice between the two antifolates should also be guided by pharmacoeconomic aspects, different toxicity profiles and personal clinical experience.
Both the EMPHACIS trial and the EORTC trials not only highlighted the role of thymidylate synthase inhibitors, in addition to platinum, in the treatment of MPM but they also showed that the combination regimens are superior to single-agent CT, and therefore, indirectly, also to palliative care only (18).
In clinical practice, carboplatin has often been substituted for cisplatin to decrease toxicity, particularly in fragile patients. Three non-randomized phase II trials evaluated the role of carboplatin plus pemetrexed in MPM patients, and reported median OS ranging from 12.7 to 14 months (23-25). In the study by Ceresoli et al., 102 patients were treated with carboplatin 5AUC plus pemetrexed 500 mg/mq every 21 days, with folic acid and vitamin B12 supplementation. Objective responses were observed in 19% of cases, with a median PFS and OS of 6.5 months and 12.7 months, respectively (24). Furthermore, a secondary combined analysis of two of these trials found that this combination was well tolerated and had a similar level of activity in elderly patients (≥70 years), compared with younger ones (26). These results are similar to those with the cisplatin-based combination. Additionally, Santoro et al. reported similar survival outcome between patients treated with cisplatin plus pemetrexed and those receiving carboplatin plus pemetrexed (mPFS 7 vs. 6.9 months; 1 year-OS 64% vs. 63.1%) (22). To date, carboplatin-pemetrexed regimen may be a reasonable alternative if cisplatin toxicity represents a concern.
The combination of cisplatin plus gemcitabine was also evaluated in some phase II trials suggesting that it may be an alternative in patients not candidates to pemetrexed, despite heterogeneity between studies with response rates and survival ranging from 12–48% and 9.5–12 months, respectively (3,27-31). Furthermore, the use of carboplatin with gemcitabine has been investigated showing good tolerance and a response rate of 26% (32).
In a multicenter randomized phase II trial performed by Kindler et al. (33), 106 chemonaive patients were treated with cisplatin plus gemcitabine with or without bevacizumab; no OS benefit (15 months in both arms) was observed with the addition of bevacizumab, though a potential benefit may have potentially been obscured by the use of second-line pemetrexed.
Cisplatin has also been tested in combination with other older chemotherapeutic agents, such as anthracyclines, mitomycin, methotrexate and vinblastine (15,34-37). However, these phase II trials do not suggest any possible advantage of these regimens, either in terms of activity or of toxicity, compared with the combination of cisplatin with pemetrexed or gemcitabine.
More recently, the large multicenter phase III MAPS trial randomized 448 naive patients to receive cisplatin-pemetrexed alone or cisplatin-pemetrexed plus bevacizumab (38). The addition of bevacizumab to CT improved both median PFS (9.2 vs. 7.3 months, HR, 0.61, 95% CI: 0.50–0.75) and median OS (18.8 vs. 16.1 months, HR, 0.77, 95% CI: 0.62–0.95) compared with CT alone, though with an increased toxicity (grade 3 hypertension, proteinuria, thrombotic events). Despite its role remains controversial, this regimen is now an option for first-line therapy in carefully selected patients with unresectable mesothelioma. No data from large studies regarding the addition of bevacizumab to a carboplatin-based regimen are available as yet.
Another issue is the appropriate timing of first-line CT start, particularly in asymptomatic or symptomatically stable patients. The randomized MED trial showed a trend towards a longer time-to-symptom-progression in patients receiving immediate CT (mitomycin-vinblastine-cisplatin/carboplatin) compared with patients randomized to initial best supportive care (BSC) and subsequent addition of CT (39). These data support the early start of CT also in patients with stable symptoms, suggesting a superiority of immediate treatment. strategy. However, the small sample size of the trial does not allow to draw any definitive conclusions and, in everyday clinical practice, a watchful waiting strategy in carefully selected and asymptomatic patients can be considered as an option.
Additionally, to date, there are no standard assays for biomarkers that are currently recommended to predict response to first-line CT. In a multivariate regression analysis of prognostic factors derived from EMPHACIS trial, predictive variables that seem to be related to longer OS were represented by therapy group, vitamin supplementation, Karnofsky performance status, stage of disease, histologic subtype and white blood cell count (40). A retrospective study of 60 patients with MPM receiving pemetrexed correlated low thymidylate synthase levels with improved outcome (41). A prospective trial evaluating the role of thymidylate synthase as a predictive biomarker for pemetrexed-based therapy is ongoing (42).
Second-line treatment with single-agent CT
Most MPM patients progressing after first-line treatment can receive further courses of CT. Few data are available to guide the clinical decision making in the selection of second-line therapy.
If disease progression occurs after a prolonged break from a platinum-pemetrexed-based regimen, patients can be rechallenged with the antifolate. As a matter of fact, Jassem et al. conducted a phase III trial to compare pemetrexed to BSC in 243 previously treated pemetrexed-naive patients showing a statistically improvement in median PFS, time to progression (TTP) and time to treatment failure (TTF) in the pemetrexed arm. However, no statistically significant differences were detected in terms of overall survival (43).
To date, single agent-based CT is an accepted practice, based upon phase II studies demonstrating improved response rates with gemcitabine, vinorelbine or anthracyclines (44-47). The combination of cisplatin-gemcitabine (48), irinotecan-cisplatin-mitomycin (49), and oxaliplatin-raltitrexed (50,51), have also been evaluated as second-line approaches. Additionally, in the phase II trial by Giaccone et al., the platinum-complex ZD0473 showed no benefit as second-line strategy (52).
However, few prospective studies have been published regarding pemetrexed-pretreated MPM patients; as a result, it is still unknown which are the best agents to be used in the second-line setting.
Currently, trials assessing the role of maintenance therapy with pemetrexed are ongoing (53).
Conclusions
The management of MPM currently represents a critical challenge.
Cumulative evidence suggests that CT does have a role in the palliative treatment of advanced mesothelioma yielding an objective response in 40–50% of patients, an improvement of symptoms in most patients and a modest survival benefit over BSC. Most guidelines therefore recommend its use with the combination of platinum compounds plus pemetrexed, with or without bevacizumab, representing the standard first-line CT for MPM patients. Despite the systemic treatment, the prognosis of these patients remains poor, with median OS of approximately 12 months (3).
Many therapeutic strategies have been studied or are under development in order to improve the outcome of MPM patients, focusing on the underlying biology and molecular pathways of the disease.
However, the molecular heterogeneity and the low incidence of mesothelioma hinder the development of tailored effective treatments. Thus, patients’ participation in clinical trials should also be encouraged whenever possible.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Wu L, de Perrot M. Radio-immunotherapy and chemo-immunotherapy as a novel treatment paradigm in malignant pleural mesothelioma. Transl Lung Cancer Res 2017;6:325-34. [Crossref] [PubMed]
- Taioli E, Wolf AS, Camacho-Rivera M, et al. Women with malignant pleural mesothelioma have a threefold better survival rate than men. Ann Thorac Surg 2014;98:1020-4. [Crossref] [PubMed]
- Mancuso MR, Neal JW. Novel systemic therapy against malignant pleural mesothelioma. Transl Lung Cancer Res 2017;6:295-314. [Crossref] [PubMed]
- Herndon JE, Green MR, Chahinian AP, et al. Factors predictive of survival among 337 patients with mesothelioma treated between 1984 and 1994 by the Cancer and Leukemia Group B. Chest 1998;113:723-31. [Crossref] [PubMed]
- Curran D, Sahmoud T, Therasse P, et al. Prognostic factors in patients with pleural mesothelioma: the European Organization for Research and Treatment of Cancer experience. J Clin Oncol 1998;16:145-52. [Crossref] [PubMed]
- Patel SC, Dowell JE. Modern management of malignant pleural mesothelioma. Lung Cancer 2016;7:63-72. [PubMed]
- Bibby AC, Tsim S, Kanellakis N, et al. Malignant pleural mesothelioma: an update on investigation, diagnosis and treatment. Eur Respir Rev 2016;25:472-86. [Crossref] [PubMed]
- Hjerpe A, Ascoli V, Bedrossian CWM, et al. Guidelines for the cytopathologic diagnosis of epithelioid and mixed-type malignant mesothelioma. Complementary statement from the International Mesothelioma Interest Group, also endorsed by the International Academy of Cytology and the Papanicolaou Society of Cytopathology. Acta Cytol 2015;59:2-16. [Crossref] [PubMed]
- Vogelzang NJ, Rusthoven JJ, Symanowski J, et al. Phase III study of pemetrexed in combination with cisplatin versus cisplatin alone in patients with malignant pleural mesothelioma. J Clin Oncol 2003;21:2636-44. [Crossref] [PubMed]
- Maziak DE, Gagliardi A, Haynes AE, et al. Surgical management of malignant pleural mesothelioma: a systematic review and evidence summary. Lung Cancer 2005;48:157-69. [Crossref] [PubMed]
- Krug LM, Pass HI, Rusch VW, et al. Multicenter phase II trial of neoadjuvant pemetrexed plus cisplatin followed by extrapleural pneumonectomy and radiation for malignant pleural mesothelioma. J Clin Oncol 2009;27:3007-13. [Crossref] [PubMed]
- Treasure T, Lang-Lazdunski L, Waller D, et al. Extra-pleural pneumonectomy versus no extra-pleural pneumonectomy for patients with malignant pleural mesothelioma: clinical outcomes of the Mesothelioma and Radical Surgery (MARS) randomised feasibility study. Lancet Oncol 2011;12:763-72. [Crossref] [PubMed]
- Stahel RA, Riesterer O, Xyrafas A, et al. Neoadjuvant chemotherapy and extrapleural pneumonectomy of malignant pleural mesothelioma with or without hemithoracic radiotherapy (SAKK 17/04): a randomised, international, multicentre phase 2 trial. Lancet Oncol 2015;16:1651-8. [Crossref] [PubMed]
- Samson MK, Wasser LP, Borden EC, et al. Randomized comparison of cyclophosphamide, imidazole carboxamide, and adriamycin versus cyclophosphamide and adriamycin in patients with advanced stage malignant mesothelioma: a Sarcoma Intergroup Study. J Clin Oncol 1987;5:86-91. [Crossref] [PubMed]
- Chahinian AP, Antman K, Goutsou M, et al. Randomized phase II trial of cisplatin with mitomycin or doxorubicin for malignant mesothelioma by the Cancer and Leukemia Group B. J Clin Oncol 1993;11:1559-65. [Crossref] [PubMed]
- Ellis P, Davies AM, Evans WK, et al. The use of chemotherapy in patients with advanced malignant pleural mesothelioma: a systematic review and practice guideline. J Thorac Oncol 2006;1:591-601. [Crossref] [PubMed]
- Tsao AS, Wistuba I, Roth JA, et al. Malignant pleural mesothelioma. J Clin Oncol 2009;27:2081-90. [Crossref] [PubMed]
- Muers MF, Stephens RJ, Fisher P, et al. Active symptom control with or without chemotherapy in the treatment of patients with malignant pleural mesothelioma (MS01): a multicentre randomised trial. Lancet 2008;371:1685-94. [Crossref] [PubMed]
- van Meerbeeck JP, Gaafar R, Manegold C, et al. Randomized phase III study of cisplatin with or without raltitrexed in patients with malignant pleural mesothelioma: an intergroup study of the European Organisation for Research and Treatment of Cancer Lung Cancer Group and the National Cancer Institute of Canada. J Clin Oncol 2005;23:6881-9. [Crossref] [PubMed]
- Thödtmann R, Depenbrock H, Dumez H, et al. Clinical and pharmacokinetic phase I study of multitargeted antifolate (LY231514) in combination with cisplatin. J Clin Oncol 1999;17:3009-16. [Crossref] [PubMed]
- Goudar RK. Review of pemetrexed in combination with cisplatin for the treatment of malignant pleural mesothelioma. Ther Clin Risk Manag 2008;4:205-11. [Crossref] [PubMed]
- Santoro A, O’Brien ME, Stahel RA, et al. Pemetrexed plus cisplatin or pemetrexed plus carboplatin for chemonaïve patients with malignant pleural mesothelioma: results of the International Expanded Access Program. J Thorac Oncol 2008;3:756-63. [Crossref] [PubMed]
- Castagneto B, Botta M, Aitini E, et al. Phase II study of pemetrexed in combination with carboplatin in patients with malignant pleural mesothelioma (MPM). Ann Oncol 2008;19:370-3. [Crossref] [PubMed]
- Ceresoli GL, Zucali PA, Favaretto AG, et al. Phase II study of pemetrexed plus carboplatin in malignant pleural mesothelioma. J Clin Oncol 2006;24:1443-8. [Crossref] [PubMed]
- Katirtzoglou N, Gkiozos I, Makrilia N, et al. Carboplatin plus pemetrexed as first-line treatment of patients with malignant pleural mesothelioma: a phase II study. Clin Lung Cancer 2010;11:30-5. [Crossref] [PubMed]
- Ceresoli GL, Castagneto B, Zucali PA, et al. Pemetrexed plus carboplatin in elderly patients with malignant pleural mesothelioma: combined analysis of two phase II trials. Br J Cancer 2008;99:51-6. [Crossref] [PubMed]
- Nowak AK, Byrne MJ, Williamson R, et al. A multicentre phase II study of cisplatin and gemcitabine for malignant mesothelioma. Br J Cancer 2002;87:491-6. [Crossref] [PubMed]
- Byrne MJ, Davidson JA, Musk AW, et al. Cisplatin and gemcitabine treatment for malignant mesothelioma: a phase II study. J Clin Oncol 1999;17:25-30. [Crossref] [PubMed]
- van Haarst JMW, Baas P, Manegold C, et al. Multicentre phase II study of gemcitabine and cisplatin in malignant pleural mesothelioma. Br J Cancer 2002;86:342-5. [Crossref] [PubMed]
- Castagneto B, Zai S, Dongiovanni D, et al. Cisplatin and gemcitabine in malignant pleural mesothelioma: a phase II study. Am J Clin Oncol 2005;28:223-6. [Crossref] [PubMed]
- Kalmadi SR, Rankin C, Kraut MJ, et al. Gemcitabine and cisplatin in unresectable malignant mesothelioma of the pleura: a phase II study of the Southwest Oncology Group (SWOG 9810). Lung Cancer 2008;60:259-63. [Crossref] [PubMed]
- Favaretto AG, Aversa SML, Paccagnella A, et al. Gemcitabine combined with carboplatin in patients with malignant pleural mesothelioma: a multicentric phase II study. Cancer 2003;97:2791-7. [Crossref] [PubMed]
- Kindler HL, Karrison TG, Gandara DR, et al. Multicenter, double-blind, placebo-controlled, randomized phase II trial of gemcitabine/cisplatin plus bevacizumab or placebo in patients with malignant mesothelioma. J Clin Oncol 2012;30:2509-15. [Crossref] [PubMed]
- Ardizzoni A, Rosso R, Salvati F, et al. Activity of doxorubicin and cisplatin combination chemotherapy in patients with diffuse malignant pleural mesothelioma. An Italian Lung Cancer Task Force (FONICAP) Phase II study. Cancer 1991;67:2984-7. [Crossref] [PubMed]
- Berghmans T, Lafitte JJ, Paesmans M, et al. A phase II study evaluating the cisplatin and epirubicin combination in patients with unresectable malignant pleural mesothelioma. Lung Cancer 2005;50:75-82. [Crossref] [PubMed]
- Hunt KJ, Longton G, Williams MA, et al. Treatment of malignant mesothelioma with methotrexate and vinblastine, with or without platinum chemotherapy. Chest 1996;109:1239-42. [Crossref] [PubMed]
- Middleton GW, Smith IE, O’Brien ME, et al. Good symptom relief with palliative MVP (mitomycin-C, vinblastine and cisplatin) chemotherapy in malignant mesothelioma. Ann Oncol 1998;9:269-73. [Crossref] [PubMed]
- Zalcman G, Mazieres J, Margery J, et al. Bevacizumab for newly diagnosed pleural mesothelioma in the Mesothelioma Avastin Cisplatin Pemetrexed Study (MAPS): a randomised, controlled, open-label, phase 3 trial. Lancet 2016;387:1405-14. [Crossref] [PubMed]
- O’Brien MER, Watkins D, Ryan C, et al. A randomised trial in malignant mesothelioma (M) of early (E) versus delayed (D) chemotherapy in symptomatically stable patients: the MED trial. Ann Oncol 2006;17:270-5. [Crossref] [PubMed]
- Rollins KD, Lindley C. Pemetrexed: a multitargeted antifolate. Clin Ther 2005;27:1343-82. [Crossref] [PubMed]
- Righi L, Papotti MG, Ceppi P, et al. Thymidylate synthase but not excision repair cross-complementation group 1 tumor expression predicts outcome in patients with malignant pleural mesothelioma treated with pemetrexed-based chemotherapy. J Clin Oncol 2010;28:1534-9. [Crossref] [PubMed]
- Study of Cytoreductive Surgery and Hyperthermic Intraoperative Chemotherapy With Pemetrexed and Cisplatin for Malignant Pleural Mesotheliomas. Available online: https://clinicaltrials.gov/ct2/show/NCT02838745
- Jassem J, Ramlau R, Santoro A, et al. Phase III trial of pemetrexed plus best supportive care compared with best supportive care in previously treated patients with advanced malignant pleural mesothelioma. J Clin Oncol 2008;26:1698-704. [Crossref] [PubMed]
- Zucali PA, Simonelli M, Michetti G, et al. Second-line chemotherapy in malignant pleural mesothelioma: results of a retrospective multicenter survey. Lung Cancer 2012;75:360-7. [Crossref] [PubMed]
- Skubitz KM. Phase II trial of pegylated-liposomal doxorubicin (Doxil) in mesothelioma. Cancer Invest 2002;20:693-9. [Crossref] [PubMed]
- Stebbing J, Powles T, McPherson K, et al. The efficacy and safety of weekly vinorelbine in relapsed malignant pleural mesothelioma. Lung Cancer 2009;63:94-7. [Crossref] [PubMed]
- Toyokawa G, Takenoyama M, Hirai F, et al. Gemcitabine and vinorelbine as second-line or beyond treatment in patients with malignant pleural mesothelioma pretreated with platinum plus pemetrexed chemotherapy. Int J Clin Oncol 2014;19:601-6. [Crossref] [PubMed]
- Vogelzang NJ. Gemcitabine and cisplatin: second-line chemotherapy for malignant mesothelioma? J Clin Oncol 1999;17:2626-7. [PubMed]
- Fennell DA, Steele JPC, Shamash J, et al. Efficacy and safety of first- or second-line irinotecan, cisplatin, and mitomycin in mesothelioma. Cancer 2007;109:93-9. [Crossref] [PubMed]
- Fizazi K, Doubre H, Le Chevalier T, et al. Combination of raltitrexed and oxaliplatin is an active regimen in malignant mesothelioma: results of a phase II study. J Clin Oncol 2003;21:349-54. [Crossref] [PubMed]
- Porta C, Zimatore M, Bonomi L, et al. Raltitrexed-Oxaliplatin combination chemotherapy is inactive as second-line treatment for malignant pleural mesothelioma patients. Lung Cancer 2005;48:429-34. [Crossref] [PubMed]
- Giaccone G, O’Brien MER, Byrne MJ, et al. Phase II trial of ZD0473 as second-line therapy in mesothelioma. Eur J Cancer 2002;38 Suppl 8:S19-24. [Crossref] [PubMed]
- Pemetrexed Disodium/Observation in Treating Patients W/ Malignant Pleural Mesothelioma w/Out Progressive Disease After 1st Line Chemotherapy. Available online: https://clinicaltrials.gov/ct2/show/NCT01085630


