Posterior mediastinal tuberculous lymphadenitis with dysphagia as the main symptom: a case report and literature review
Introduction
Mediastinal tuberculous lymphadenitis (MTL) is mostly seen in primary tuberculosis in children (1), uncommon observed in adults (2). It usually presents the toxic symptoms of tuberculosis but rarely with symptoms characteristic of esophageal compression, such as dysphagia. Such patients can easily be misdiagnosed as esophageal neoplasm and get delayed or faulty treatment. Here is such a case.
Case report
A 32-year-old man presented with dull chest pain of one month and dysphagia for solid food of five days. He had no other digestive symptoms, denied weight loss, mild fever, cough and night sweating. He had been admitted because of allergic purpura twice from 2002 to 2003, and it did not relapse until two weeks before hospitalization. Some petechiaes were noted on the lower legs in a symmetrical distribution. His other past medical history was unremarkable. CRP was elevated, and a skin test was strongly positive. Tests for infectious diseases were negative, including HIV, hepatitis B, hepatitis C and syphilis. The other laboratory tests were all within normal limits, including ESR, LDH, ADA and tuberculosis protein chip.
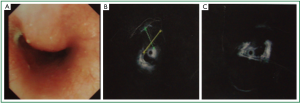
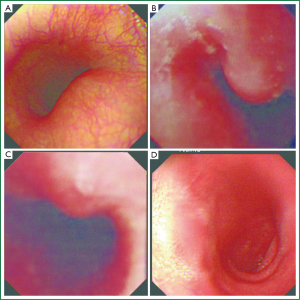
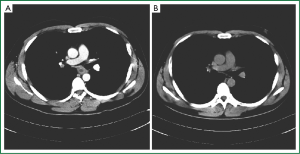
At upper endoscopy, a protruding lesion covered by normal mucosa was seen at 26 cm from the upper incisor (Figure 1). His barium swallow showed visible external compressive stricture on the middle-lower esophagus with normal mucosal pattern (Figure 2). Chest computed tomography (CT) scan showed a subcarinal mass adjacent to the esophageal wall in posterior mediastinum (Figure 3). An endoscopic ultrasonography (EUS) revealed a hypoechoic lesion suspected of esophageal stromal tumor in the fourth layer (Figure 4). A grey-white tissue was obtained by ultrasound-guided fine-needle aspiration (EUS-FNA), but cytopathology, bacilliculture and PCR test had no special findings.
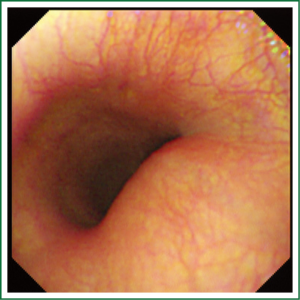
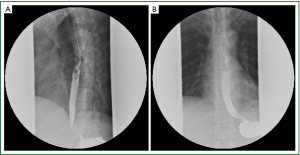
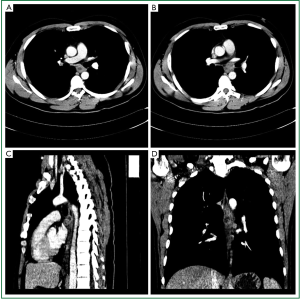
Though multiple examinations had been conducted, the diagnosis was still a mystery. The patient required experimental antituberculous treatment according to the positive skin test. After the first month of careful treatment, an enhanced CT scan showed the reduced node had central low attenuation and peripheral rim enhancement, with some cystic low density formed. The radiological feature as response to antituberculous therapy supported for the diagnosis of tuberculosis. The patient checked regularly CT, barium swallow and endoscopy. The size of the protruding lesion reduced gradually during therapy period (Figures 5,6). He received antituberculous treatment for 12 months and did not have obviously adverse reactions except hyperuricemia of 700 μmol/L (normal, 90-420 μmo1/L) which disappeared after stopped pyrazinamide in the second month of treatment. The symptoms of purpura also disappeared in the second month.
Discussion
Dysphagia with esophageal mechanical obstruction usually results from stricture caused by intramural or extrinsic lesions. Esophageal neoplasm is the most frequent cause and considered first in the clinic. Conventional endoscopy is an established method for diagnosing gastrointestinal tract diseases, however it usually can not appropriately evaluate the endoluminal protrusions with normal mucosa alone (3). EUS can distinguish between extrinsic compression and submucosal tumor with 95% to 100% accuracy (4-6), which is superior to endoscopy and radiological examination (7). It separates the digestive wall into five layers and reveals the exact origin of a lesion. In fact, the EUS did not define the exact origin in our case. The inflammatory adhesion between the esophagus and lymphonodus might cause the confusion of the stricture. EUS also helps to differentiate diagnosis between benign and malignant submucosal tumors (8) and improves the diagnostic accuracy (9) according to the characteristics of echo. But Hwang et al. (6) found that EUS imaging alone is insufficient to accurately diagnose 3rd and 4th layer hypoechoic masses which agreed with the histologic diagnosis in only 10 of 23 cases. So he advised to obtain histologic confirmation whenever possible.
MTL can cause dysphagia by compressing the thoracic esophagus. The enlarged lymph nodes mainly locate in the upper and middle zone of the mediastinum and more in the right side than in the left side (10,11). The tuberculin skin test is a screening measure for tuberculosis. Although the skin test has false-positive and false-negative rate, it also can provide some reference for tuberculosis (12,13). The imageological technique is of great help to diagnosis of MTL. The classical CT findings are nodes with central low attenuation and peripheral rim enhancement, frequently with a multilocular appearance (10,11,14,15). But when lymph nodes have tuberculous hyperplasia with no caseous necrosis, its enhancement is homogeneous without a central low density area (10). In our case, the CT features conformed to the typical imaging manifestation of lymphoid tuberculosis after 1-month antituberculous treatment, but the anatomic relationship between the mass and esophageal wall could not be still clarified. The most common MRI imaging appearance of MTL is as inhomogeneous nodes with marked hyperintensity on T2-weighted images and peripheral enhancement (16). Some studies on the EUS features of MTL have been done in recent years. Fritscher-Ravens et al. (17) reported that inhomogeneous, hyperechoic areas with or without shadowing were seen within the tuberculosis nodes. The acoustic shadowing might represent gas produced by the bacteria within or calcifications of former inactive tuberculosis. Rana et al. (18) summarized that patchy anechoic or hypoechoic areas or hyperechoic foci in the mediastinal lymph nodes on EUS were important signs of mediastinal tubercular lymphadenopathy.
Biopsy is always a good tool in the diagnosis of disease. Cytopathology and bacilliculture can be carried out on samples directly collected from the infection site. Fourther, when histopathology and culture are negative, PCR test can be performed as a diagnostic method for extrapulmonary tuberculosis (19,20). As a minimally invasive tool, EUS-FNA can aid cytological evaluation to diagnosis gastrointestinal diseases and mediastinal diseases if sufficient material has been obtained. The diagnostic accuracy is not associated with mass location, mass size, needle size, but 3.0 or more needle passes and combined cytologic-histologic analysis enhance the accuracy (21). For MTL, Fritscher-Ravens et al. (17) reported the sensitivity, specificity, and positive and negative predictive values of EUS-FNA were 86%, 100%, 100%, and 91%, respectively. In our case, a grey-white tissue was obtained by EUS-FNA, but all of cytopathology, bacilliculture and PCR test had no special findings. A new biopsy was refused. The overall risk of complications from EUS-FNA is relatively low (1.6%) (22) with perforation, aspiration pneumonia, bleeding. But a case of mediastinal-esophageal fistulae after EUS-FNA of tuberculosis of the mediastinum reported by Von Bartheld et al. (23) is worth our attention. Furthermore, EUS also can apply to the lesions in locations that are difficult to access (e.g., posterior mediastinum) (24). Mediastinoscopy (25,26) and thoracoscopy (27) can obtain diagnostic material from a mediastinal mass safety and easily. Mediastinoscopy has been shown to have the best diagnosis yield (100%) (28) in MTL. But they are invasive procedures and done under general anesthesia. The CT scan (Figure 3) showed that the mass was between the atrium and tracheal carina, meanwhile prior to the esophagus. The special location made that both of the mediastinoscopy and thoracoscopy could not be conducted.
Other rare mediastinal disease such as sarcoidosis, lymphoma, or distant metastases should be included in the differential diagnosis of MTL. Some laboratory tests such as tumor makers, serum adenosine deaminase (29-31), angiotensin converting enzyme (32,33) and radiological examinations are helpful to identify these diseases. The CT scan of sarcoidosis usually shows that symmetrical and homogeneous enlargement of bilateral hilar lymph nodes (11), which can be used to differentiate it from tuberculosis. Homogeneous enhancement is more commonly seen in lymphoma than in tuberculosis (34). For most metastases, it will be not difficult to be diagnosed after the primary disease has emerged.
At the initial stage of the disease, our patient was advised to undergo surgery because of misdiagnosis of esophageal cancer and other mechanical tumors by other hospitals. Although the radiological, endoscopic and EUS-FNA did not provide evidence to establish tuberculosis infection, the positive skin test gave a prompting to the diagnosis of MTL. The CT scan and endoscopy response to antituberculous therapy supported for the diagnosis of tuberculosis. The allergic purpura may be the extra-pulmonary manifestation of tuberculosis caused by abnormal immunity.
The prognosis of MTL with an adequate treatment is well, but surgery be prepared, when necessary, to resolve the symptoms of esophageal compression. In conclusion, we could not ignore the diagnosis of MTL facing posterior mediastinal mass with dysphagia. Analyzing and evaluating test results comprehensively is the key to make correct diagnosis and timely treatment. The experimental antituberculous treatment should be used if MTL is highly suspected.
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- Venkateswaran RV, Barron DJ, Brawn WJ, et al. A forgotten old disease: mediastinal tuberculous lymphadenitis in children. Eur J Cardiothorac Surg 2005;27:401-4. [PubMed]
- Amorosa JK, Smith PR, Cohen JR, et al. Tuberculous mediastinal lymphadenitis in the adult. Radiology 1978;126:365-8. [PubMed]
- Argüello L. Endoscopic ultrasonography in submucosal lesions and extrinsic compressions of the gastrointestinal tract. Minerva Med 2007;98:389-93. [PubMed]
- Motoo Y, Okai T, Ohta H, et al. Endoscopic ultrasonography in the diagnosis of extraluminal compressions mimicking gastric submucosal tumors. Endoscopy 1994;26:239-42. [PubMed]
- Rösch T. Endoscopic ultrasonography in upper gastrointestinal submucosal tumors: a literature review. Gastrointest Endosc Clin N Am 1995;5:609-14. [PubMed]
- Hwang JH, Saunders MD, Rulyak SJ, et al. A prospective study comparing endoscopy and EUS in the evaluation of GI subepithelial masses. Gastrointest Endosc 2005;62:202-8. [PubMed]
- Shen EF, Arnott ID, Plevris J, et al. Endoscopic ultrasonography in the diagnosis and management of suspected upper gastrointestinal submucosal tumours. Br J Surg 2002;89:231-5. [PubMed]
- Martínez-Ares D, Souto-Ruzo J, Yanez LJ, et al. Usefulness of endoscopic ultrasonography in the preoperative diagnosis of submucosal digestive tumours. Rev Esp Enferm Dig 2005;97:416-26. [PubMed]
- Nikolić M, Boban M, Ljubicic N, et al. Evaluation of upper gastrointestinal submucosal lesions by endoscopic ultrasonography. Acta Med Croatica 2009;63 Suppl 3:29-37. [PubMed]
- Luo MY, Liu L, Lai LS, et al. Deepgoing study on intrathoracic tuberculous lymphadenitis in adults using multidetector CT. Chin Med J (Engl) 2010;123:1283-8. [PubMed]
- Tang SS, Yang ZG, Deng W, et al. Differentiation between tuberculosis and lymphoma in mediastinal lymph nodes: Evaluation with contrast-enhanced MDCT. Clin Radiol 2012;67:877-83. [PubMed]
- King AB. Accurately interpreting PPD skin test results. Nurse Pract 1999;24:144-7. [PubMed]
- Orsi GB, Antoniozzi T, Ortis M, et al. Skin test screening for tuberculosis among healthcare students: a retrospective cohort study. Ann Ig 2013;25:311-5. [PubMed]
- Im JG, Song KS, Kang HS, et al. Mediastinal tuberculous lymphadenitis: CT manifestations. Radiology 1987;164:115-9. [PubMed]
- Moon WK, Im JG, Yeon KM, et al. Mediastinal tuberculous lymphadenitis: CT findings of active and inactive disease. AJR Am J Roentgenol 1998;170:715-8. [PubMed]
- Moon WK, Im JG, Yu IK, et al. Mediastinal tuberculous lymphadenitis: MR imaging appearance with clinicopathologic correlation. AJR Am J Roentgenol 1996;166:21-5. [PubMed]
- Fritscher-Ravens A, Ghanbari A, Topalidis T, et al. Granulomatous mediastinal adenopathy: can endoscopic ultrasound-guided fine-needle aspiration differentiate between tuberculosis and sarcoidosis? Endoscopy 2011;43:955-61. [PubMed]
- Rana SS, Bhasin DK, Srinivasan R, et al. Endoscopic ultrasound (EUS) features of mediastinal tubercular lymphadenopathy. Hepatogastroenterology 2011;58:819-23. [PubMed]
- Mehta PK, Raj A, Singh N, et al. Diagnosis of extrapulmonary tuberculosis by PCR. FEMS Immunol Med Microbiol 2012;66:20-36. [PubMed]
- Ajantha GS, Shetty PC, Kulkarni RD, et al. PCR as a diagnostic tool for extra-pulmonary tuberculosis. J Clin Diagn Res 2013;7:1012-5. [PubMed]
- Rong L, Kida M, Yamauchi H, et al. Factors affecting the diagnostic accuracy of endoscopic ultrasonography-guided fine-needle aspiration (EUS-FNA) for upper gastrointestinal submucosal or extraluminal solid mass lesions. Dig Endosc 2012;24:358-63. [PubMed]
- Bardales RH, Stelow EB, Mallery S, et al. Review of endoscopic ultrasound-guided fine-needle aspiration cytology. Diagn Cytopathol 2006;34:140-75. [PubMed]
- von Bartheld MB, van Kralingen KW, Veenendaal RA, et al. Mediastinal-esophageal fistulae after EUS-FNA of tuberculosis of the mediastinum. Gastrointest Endosc 2010;71:210-2. [PubMed]
- Südhoff T, Hollerbach S, Wilhelms I, et al. Clinical utility of EUS-FNA in upper gastrointestinal and mediastinal disease. Dtsch Med Wochenschr 2004;129:2227-32. [PubMed]
- Nalladaru ZM, Wessels A. The role of mediastinoscopy for diagnosis of isolated mediastinal lymphadenopathy. Indian J Surg 2011;73:284-6. [PubMed]
- Jacob B, Parsa R, Frizzell R, et al. Mediastinal tuberculosis in Bradford, United Kingdom: the role of mediastinoscopy. Int J Tuberc Lung Dis 2011;15:240-5. [PubMed]
- Kitami A, Suzuki T, Usuda R, et al. Diagnostic and therapeutic thoracoscopy for mediastinal disease. Ann Thorac Cardiovasc Surg 2004;10:14-8. [PubMed]
- Ayed AK, Behbehani NA. Diagnosis and treatment of isolated tuberculous mediastinal lymphadenopathy in adults. Eur J Surg 2001;167:334-8. [PubMed]
- Wetzel E, Müller-Quernheim J, Lorenz J. Serum adenosine deaminase as a parameter for activity in sarcoidosis. Pneumologie 1999;53:323-8. [PubMed]
- Aghaei M, Karami-Tehrani F, Salami S, et al. Adenosine deaminase activity in the serum and malignant tumors of breast cancer: the assessment of isoenzyme ADA1 and ADA2 activities. Clin Biochem 2005;38:887-91. [PubMed]
- Tarhan G, Gümüşlü F, Yilmaz N, et al. Serum adenosine deaminase enzyme and plasma platelet factor 4 activities in active pulmonary tuberculosis, HIV-seropositive subjects and cancer patients. J Infect 2006;52:264-8. [PubMed]
- Linssen N. Increased serum activity of angiotensin-converting enzyme (ACE): indication of sarcoidosis? A ‘Bayesian’ approach. Ned Tijdschr Geneeskd 2003;147:1292-3. [PubMed]
- Tasaki M, Hattori N, Ihara D, et al. Case report: A case of Hodgkin lymphoma required a differential diagnosis from sarcoidosis due to elevated serum level of angiotensin converting enzyme (ACE). Nihon Naika Gakkai Zasshi 2012;101:1401-3. [PubMed]
- Tang SS, Yang ZG, Deng W, et al. Differentiation between tuberculosis and lymphoma in mediastinal lymph nodes: Evaluation with contrast-enhanced MDCT. Clin Radiol 2012;67:877-83. [PubMed]


