Asthma combined with Hodgkin’s lymphoma: a case report and review of the literature
Introduction
Both asthma and hematological malignancies are influenced by genetic and environmental factors. The previous studies have revealed that a slight excess of cases of Hodgkin’s disease (HD) was found among atopic men, and a slight excess of non-Hodgkin’s lymphoma (NHL) among atopic women (1). However, the relationship between asthma and Hodgkin’s lymphoma has not been well recognized. Here we report a case of asthma combined with Hodgkin’s lymphoma and review the related literature.
Case report
A 53-year-old male patient presented with the complaint of cough, progressive wheezing and exertional dyspnea accompanied by full-body rash for three months. He was diagnosed as asthma four years ago with a normal chest X-ray. The patient had been exposed to paint for three months before diagnosis of asthma. He was treated with inhaled glucocorticosteroids and a long-acting bronchodilator for threee years. Asthma symptoms had been under control until three months ago.
Physical examination: skin rash can be seen scattered in the whole body, raised above the surface, with irregular border, and itching. Enlarged lymph nodes could be felt in neck bilaterally, and those in the left were integrated, 3 cm × 5 cm, rigid, fixation, without tenderness.
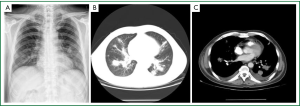
Chest X-ray and CT scan (Figure 1) showed several large masses involving bilateral lung field and hilum.
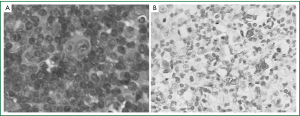
Laboratory examination showed: raised C-reactive protein concentration (24.10 mg/dL), elevated erythrocyte sedimentation rate (98 mm/h) and increased serum immunoglobulin E concentrations (279 IU/L). Biopsy pathology of the enlarged lymph node in the right side of the neck (Figure 2): Hodgkin’s lymphoma, nodular sclerosis type. Immunohistochemical and special staining: CD30+, CD15+, Fascin+, EBV-/+, CD20-, LCA-, EMA-, CD3-, ALK-1 -, ALCL-. PET/CT: nodes with slightly higher metabolism at the right side of the neck and the right hilar (SUV max 2.1) were considered infiltration of lymphoma.
Diagnosis: Hodgkin’s lymphoma (nodular sclerosis type); asthma
Treatment and follow-up: The patient received six-time chemotherapy of ABVD (doxorubicin, bleomycin, vinblastine, and darcarbacine). During the process, ICS was not used, coughing, wheezing and dyspnea were improved, and no acute exacerbation of asthma occurred. Chest CT follow-up revealed that nodules in bilateral lung fields were reduced significantly.
Discussion
A study has revealed that a slight excess of cases of HD and NHL among atopic person (1). As we know, both asthma and haematological malignancies are influenced by genetic and environmental factors, and asthma was associated with a T helper 2 dominant lymphocyte (Th2) response. Also HD has been found to be associated with a Th2 response similar to asthma (2). Allergens with high molecular weight can stimulate the immune system through an IgE-mediated pathway, which was associated with risk for HD. The mechanism may be directly related to the nature of Th2 responses providing a favorable environment for the growth and survival of Reed-Sternberg cells (3). In this index case, the patient had been exposed to paint for three months. Then he suffered asthma, several months later, he was diagnosis as HD. Maybe paint stimulated the Th2 response and increased serum immunoglobulin E concentrations, so that induced the asthma attack and HD as well. On the other hand, CD30 is a member of the TNF/NGF receptor super-family and a marker for Th2 phenotype. It is revealed that raised serum levels of sCD30 are found in atopic asthmatics. Also serum levels of soluble CD30 (sCD30) have been already used as prognostic markers in HD. In this case, immunohistochemical staining of the lymph node specimen shows that CD30 is positive. So we hypothesis that the conditions altering normal immune system function may not only result in an impaired ability to suppress activation of autoimmune cells, but also influence elimination of malignant hematological cells. In conclusion, asthma and Hodgkin’s lymphoma maybe can coexist.
Initially, this patient was diagnosed with asthma while chest X-ray was normal. But months later, it was found several mass located in bilateral lung field and hilum. Biopsy pathology showed that is Hodgkin’s lymphoma. Vajdic and his colleagues (4) observed that the risk of haematological malignancies from pesticide exposures was higher among asthmatics than the risk among non-asthmatics. Whether asthma will increase susceptibility to Hodgkin’s lymphoma or not? As we know, the deviation in asthma toward a shift in the T-lymphocyte response away from the Th1 to Th2 dominated activity, with elevated IL-4, IL-5 and IL-13, might inhibit Th1 responses that could protect against cancer. This skewing of the immune response could also exacerbate the effects of carcinogens, some of which inhibit some aspects of the immune system, acting synergistically with the asthma. In addition, because of asthmatics’ impaired mucociliary system and pulmonary function, they are more susceptible to carcinogens. Therefore we suspected that patient in this case suffered from asthma which could increase susceptibility to Hodgkin’s lymphoma.
Furthermore, glucocorticoids which are taken for asthma may facilitate development of HD due to their cellular and humoral immunosuppression (5). CD4+CD25+T cell is a new type of suppressor cell, which plays an important role in the tumor immune suppression. Li and colleagues found increased percentage of CD4+CD25+ regulatory T cells on asthma mice model after 24 hours of glucocorticoid treatment, compared with the control group (6). Therefore, the therapeutic drug for asthma, may also increase one’s susceptibility to Hodgkin’s lymphoma.
On the other hand, some special HD, such as: mediastinal enlarged lymph node oppress the trachea and bronchial; primary pulmonary Hodgkin’s lymphoma (PPHL); endobronchial Hodgkin’s lymphoma (7,8) presents with respiratory symptoms at the early stage. In 2005, the National Institute for Health and Clinical Excellence guidelines for referral for suspected cancer (NICE) clearly stated that “shortness of breath is a symptom that can indicate chest involvement but may be confused with conditions such as asthma (9).” So O’Carroll and his colleagues thought that those asthma patients who were non-responsive to standard treatment in primary care or who had other symptoms, should have a chest radiography test performed (10). So that we should appeal clinicians to be aware that hematologic malignacy can present with respiratory symptom.
In all, patient in this case had a four-year history of asthma, and later was diagnosed with Hodgkin’s lymphoma. After chemotherapy, both HD and asthma of this patient were well-controlled. The study implies that the common cause and progression of the two diseases relates to the imbalance of the immune system. There exists cross-promotion and the symptoms overlap between the two diseases, which should arouse the clinician’s attention to further studies.
References
- Eriksson NE, Mikoczy Z, Hagmar L. Cancer incidence in 13811 patients skin tested for allergy. J Investig Allergol Clin Immunol 2005;15:161-6. [PubMed]
- Skinnider BF, Mak TW. The role of cytokines in classical Hodgkin lymphoma. Blood 2002;99:4283-97. [PubMed]
- Kogevinas M, Zock JP, Alvaro T, et al. Occupational exposure to immunologically active agents and risk for lymphoma. Cancer Epidemiol Biomarkers Prev 2004;13:1814-8. [PubMed]
- Vajdic CM, Fritschi L, Grulich AE, et al. Atopy, exposure to pesticides and risk of non-Hodgkin lymphoma. Int J Cancer 2007;120:2271-4. [PubMed]
- Oehling AG, Akdis CA, Schapowal A, et al. Suppression of the immune system by oral glucocorticoid therapy in bronchial asthma. Allergy 1997;52:144-54. [PubMed]
- Li M, Song L, Zhang JB, et al. Effect of glucocorticoid on CD4+CD25+ T regulatory cells in asthmatic mice. Zhongguo Dang Dai Er Ke Za Zhi 2008;10:527-30. [PubMed]
- Ahmed S, Kussick SJ, Siddiqui AK, et al. Bronchial-associated lymphoid tissue lymphoma: a clinical study of a rare disease. Eur J Cancer 2004;40:1320-26. [PubMed]
- Kumar R, Sidhu H, Mistry R, et al. Primary pulmonary Hodgkin’s lymphoma: a rare pitfall in transthoracic fine needle aspiration cytology. Diagn Cytopathol 2008;36:666-9. [PubMed]
- National Institute for Health and Clinical Excellence [Internet]. Referral guidelines for suspected cancer in adults and children. c2011. Available from: www.nice.org.uk/guidance/
- O’Carroll N, Fitzsimons J, Carr S. Asthma unresponsive to simple treatment in a child. BMJ 2008;336:447. [PubMed]


