Clinical care for patients with recurrent myocardial ischemia in Germany—the VOICES trial
Introduction
Chronic ischemic heart disease is the most common cause of death in western countries including Germany (1). In 2010, more than 255,000 patients were admitted to hospital for angina pectoris (AP). Typically, in patients with coronary artery disease (CAD) significant stenoses can be found in coronary angiography. However, in daily practice many patients suffer from recurrent AP despite a lack of significant stenoses (2-5). Moreover, patients with AP and documented myocardial ischemia without obstructive CAD have been shown to have a poor outcome in a large-scale clinical registry (6).
In the THINK-trial 2,500 patients with suspected CAD were analysed in Germany (7). Most patients suffered from typical AP, reporting a median of 3.75 episodes per week, and in 45% of the patients dyspnoea was the leading symptom. By means of coronary angiography in 62% of the patients with AP significant coronary stenoses could be excluded (7). In the ACOVA-trial only 50% of 300 patients with suspected CAD had relevant and treatable stenoses (8). In more than 60% of patients without significant stenoses epicardial spasms or microvascular disturbances were found. Furthermore, typical causes leading to AP apart from obstructive CAD are small vessel disease, diastolic dysfunction, and ventricular hypertrophy. Those changes result in increased wall tension and reduced microvascular function (9-16).
In consideration of these different aspects, there is a need for improvement of health care apart from percutaneous coronary intervention to achieve a better life quality for patients suffering from AP. An important step therefore is to define a patient’s current situation and health care status in outpatient care. Interviewing experts in this field—cardiologists in an ambulatory set-up—helps to understand the current care of patients with recurrent myocardial ischemia.
Health services research is the scientific analysis of the health service of the individual and of the population under terms of everyday live. The aim is the identification of deficiencies, the development of new concepts, and the evaluation of their efficacy (17).
The aim of this trial was to collect data of patients after coronary angiography excluding relevant stenoses referring to patients’ medical history, symptoms, and the diagnostic process. Further, the collected data should identify common classification of discomfort by recurrent ischemia as well as suitable diagnostic tests for verification of myocardial ischemia.
Methods
Data were acquired by structured interviews of cardiologists in outpatient care. The interviews were performed in selected medical (cardiological) offices all over Germany. By means of a structured interview questionnaire comprehensive data were obtained about the group of patients after diagnostic coronary angiography, their medical history and subsequent treatments, completed by case examples. A selection for special attributes was not performed, assuming that a sufficiently broad sample would produce a random distribution.
Contents of the interviews were patients after diagnostic coronary angiography, their management, and the resulting treatment. The interviews were documented by structured questionnaires. Questions were asked in the form of multiple choice answers or rating scales (scales from 1 to 10). The interview questions included the following topics:
- Patient management, communication;
- Medical history (extent, quality);
- Assessment of AP severity (CCS classification);
- Status of AP during the last 4 weeks;
- Diagnostic tools for verification of myocardial ischemia;
- Causes of AP;
- Course of action concerning persisting AP/dyspnoea;
- Drug treatment in patients with chronic myocardial ischemia;
- Monitoring of treatment success;
- Classification and prioritisation of therapeutic goals;
Evaluation of eligible drug treatments according to case studies.
To assure a suitable quality of the data acquisition including completeness of data and identification as well as correction (revision) of shortcomings, an independent institute (Statistisches Institut für Marketing und Wissenschaft; SIMW GmbH) performed a continuous support and supervision of the expert interviews. All interview sheets were transferred into digital database systems including continuous check of the plausibility and consistency of the data.
Statistics
Only completed data sheets were included into the analysis. Rating scales [1–10] were analysed by means of descriptive methods (number, mean, median, minimum, maximum, standard deviation). Absolute and relative frequency distribution was calculated for the characterisation of qualitative data and multiple-choice questions. Statistical analyses were performed with the certified program STATISTICA (Stat-Soft™ Inc.) by an independent institute (Statistisches Institut für Marketing und Wissenschaft; SIMW GmbH).
Results
In total 731 interviews were performed and could be analyzed in detail. A distinct separation in interventional vs. non-interventional cardiologists was possible in 717 of the cardiologists (249 vs. 468 respectively). Data are presented in the following paragraphs divided into the topics medical history, diagnostic work-up, and therapy.
Medical history
Data on typical recording of the patients’ history are shown in Table 1. Only a minority of patients describes their symptoms in detail spontaneously. In about 73% of the patients an intensified and structured interrogation is necessary to get a detailed picture of the patient’s problems and discomfort. 88.1% of the cardiologists perform a detailed and structured investigation of the medical history including quality of AP, cardiovascular risk factors, limitations in daily life, depressive symptoms, and comorbidities whereas nearly 12% of the interviewed experts only inquire the quality of AP.

Full table
The classification of the Canadian Cardiovascular Society (CCS classification) is used to describe the degree of symptoms in patients with stable AP (18). Whereas 646 of 731 experts (88.4%) in this trial claim that the CCS classification should be used to categorize the patient’s symptoms only 67.7% of the interviewed cardiologists use the CCS classification in patients with recurrent AP on a regular basis. The importance of the CCS classification was rated as 7.09±2.43 on a scale from 1 (no relevance) to 10 (great relevance). Other important factors included in history taking were the assessment of previous findings (92.3%), current medication (98.2%), and the efficiency of the current drug treatment on amelioration of symptoms (88.8%). In the cases, where no CCS classification is used in 92.6% the disorders are documented without using any classification. In only 2.8% the NYHA classification (classification of the New York Heart Association) is used. Another 2.8% of the interviewed doctors admit that the extent of disorders is not documented in written form.
Diagnostic work-up
The rating of suitable diagnostic procedures for the verification of myocardial ischemia is shown in Table 2. Furthermore, the experts were asked to answer in how many cases they could diagnose coronary heart disease only on a clinical basis i.e. without coronary angiography or cardiac computed tomography. Coronary heart disease is diagnosed based on clinical characteristics in about 36%. About 12% answered that they never diagnosed coronary heart disease without coronary angiography or cardiac computer tomography whereas 13% do so in more than 80% of the cases. The frequency of patients with AP symptoms and without significant stenoses in the coronary angiography was rated with a mean of 4.6±1.8 on a scale from 1 (rarely) to 10 (often).
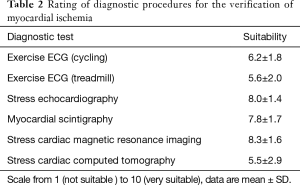
Full table
Moreover, the experts were asked whether extra-cardiac causes for AP symptoms are typically ruled out before a coronary angiography is performed. 81.4% of the cardiologists claimed to check the indication for this invasive diagnostic procedure and rule out extra-cardiac causes prior to coronary angiography. In 7.5% the general practitioner rules out extra-cardiac causes for the chest discomfort before transferring patients to the cardiologists for further work-up. 10.7% experts perform a coronary angiography first and consider extra-cardiac causes only in second line.
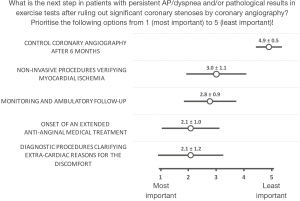
The experts were asked for subsequent diagnostic approaches after ruling out significant coronary stenoses. The results are shown in Figure 1. As the most important point the experts rated the fact of ruling out extra cardiac disorders (2.1±1.2, on a scale from 1 (most important) to 5 (least important)) and, respectively, then initiating an adequate anti-ischemic medical treatment (2.1±1.0). Furthermore, the cardiologists were asked for reasons for AP symptoms or pathological exercise testing results despite exclusion of significant coronary stenoses. On a scale from 1 (rarely) to 10 (often) they mentioned as most common causes diastolic dysfunction (6.3±2.2), small vessel disease (6.1±2.1), and endothelial dysfunction (5.7±2.2). A detailed overview is given in Table 3.
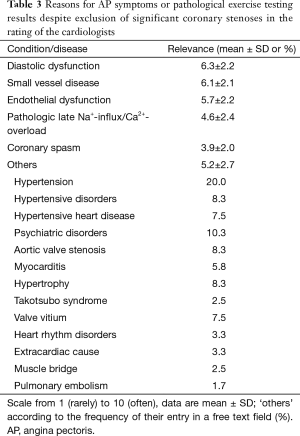
Full table
Therapy
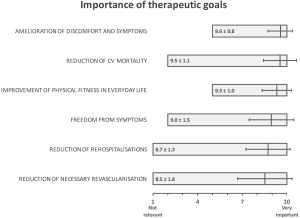
The assessment of the importance of different therapeutic goals is depicted in Figure 2. The great range of answers is remarkable—only “Amelioration of discomfort and symptoms” and “Improvement of physical fitness in everyday life” were never rated as not relevant. On a scale from 1 (I fully disagree) to 10 (I fully agree) the question was raised for the individual estimation of the significance of the late sodium influx: with a mean of 5.81±2.67 this topic was rated as of practical relevance. Moreover, the late sodium influx was seen as a cause of typical AP after percutaneous coronary intervention (6.66±2.29) and besides in patients without coronary heart disease (6.53±2.23). A need for considering this aspect by general practitioners was rated as 3.64±2.60.
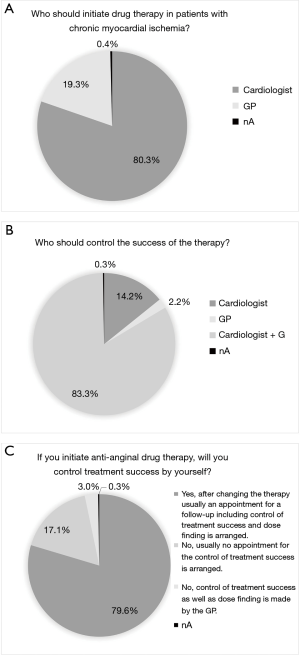
An important question for the care of patients was: who should initiate drug treatment of patients with chronic myocardial ischemia without significant stenoses? The results concerning the initiation of therapy and the control of its success are depicted in Figure 3A,B,C. In summary, most of the interviewed cardiologists initiate the therapy (80.3%) and control the success of the therapy (79.6%) themselves; even though most cardiologist see the latter as a task for the cardiologist and GP (83.3%).
Discussion
Chronic ischemic heart disease is frequent and the leading cause of death in western countries including Germany. It is one of the most common causes of hospitalisation and therefore an enormous economic burden (1). AP is the most prevalent symptom of chronic ischemic heart disease. Furthermore, the existence of AP was shown to be an important prognostic factor (6,19).
In 2010 Patel et al. published an analysis of more than 390,000 patients with AP and/or a pathologic exercise test. Coronary angiography excluded obstructive coronary heart disease in >62% (2). Obstructive coronary heart disease was defined as a stenosis of more than 50% in the left main branch and/or a stenosis of more than 70% in any other coronary vessel with a diameter of above 2 mm (2). The THINK trial recently performed in Germany confirmed those data (7). Furthermore, in patients with AP but without prior known coronary artery disease only 21% were diagnosed with obstructive coronary heart disease during coronary angiography (7).
The main conclusions that could be drawn from the THINK trial were that many patients suffer from recurrent AP and the discomfort in daily life is high, most of them being in CCS class 2 or 3 with a mean of 3 attacks per week. One of the most striking results was that in 57.8% of the cases no therapeutic consequences or changes in treatment were drawn after coronary angiography (7).
The current study aims to give an overview of the daily-life situation of patients with (chronic) AP—especially after ruling-out relevant coronary stenoses. The results of the VOICES trial point out some deficiencies in the daily practice in outpatients:
It is noticeable that most of the patients do not report on their chest discomfort in detail by themselves and especially problems in daily life also are not reported in most of the cases as shown in Table 1. In the recently published APPEARS study the authors showed a wide discrepancy between patient-reported and cardiologist-estimated burden of angina (20). The fact that patients with AP often do not express their discomfort in detail underlines the need for a proper investigation of the patient’s history including detailed questions on the quality of AP and the limitations in daily life on a regular basis. In this context it is striking that more than 10% of the asked experts admit that they do not record a detailed medical history of patients with recurrent AP. Medical history taking is of central importance in diagnosing and should be the basic step in every doctor-patient-relationship. Furthermore, this diagnostic tool is crucial for the prevention of expensive and avoidable examinations. The previously mentioned fact that patients frequently do not report their discomfort on their own strengthens this need. As the existence of AP symptoms has been recognized as an important prognostic factor (6,19) the meaning of a proper and clear registration of the patient’s discomfort is crucial. The CCS classification (18) is one tool to objectify patient’s AP symptoms. As the CCS classification is one of the basic criteria that helps to identify the therapeutic possibilities for a patient based on the current guidelines [e.g., 2013 ESC guidelines on the management of stable coronary artery disease (21)] this classification should be used in every patient with AP. In this context the divergence between interviewed cardiologists emphasising this classification and those using it on a daily base is striking.
In 10.7% of the cases coronary angiography is performed before extra-cardiac causes of disorders are ruled out. As stated by the current guidelines “it is necessary to differentiate this pain from non-cardiac chest pain” (21). This again underlines the need of a proper taking of the medical history.
Approximately 20% of the interviewed experts do not consider the initiation of a specific, antianginal medical treatment as their objective. Similarly the course of the disease and the control of the success of the therapy are not seen as only cardiologist’s tasks in 16% respectively 20%. AP is the consequence of an oxygen under-supply of the myocardium. Ischemic areas can be confirmed in exercise tests. This leads to the finding that apart from the typical coronary heart disease other reasons play a role for the mismatch of supply and demand in the heart muscle (11-13,22) and strengthens the need for a sophisticated medical treatment (21). Besides, finding the optimal stress test for this cohort of patients in matters of diagnosing ischemia is a challenge and still under debate (21). According to the guidelines there is still uncertainty whether contrast stress echocardiography or cardiac magnetic resonance are adequate instruments for reliably quantifying perfusion abnormalities whereas the availability of positron emission tomography is limited (21).
The interviews were performed before the latest version of the guidelines for the management of patients with stable coronary artery disease have been published. They contain a chapter dealing with patients with AP symptoms after ruling out obstructive coronary artery disease (21). Apart from revascularization the treatment is similar to the treatment of the “classical” coronary artery disease. The fact that the presence and extent of AP symptoms is related to a worse prognosis (6,19) strengthens the need for a sufficient drug treatment beyond the improvement in the quality of life.
Limitation
The study represents the situation of patients in a routine clinical setting. Data were collected by means of a structured interview in an open, not-blinded fashion which might result in a too optimistic presentation.
Conclusions
The VOICES trial was designed to characterize the situation of patients with angina pectoris after exclusion of significant coronary stenosis. The trial revealed deficiencies in the history taking, the proper classification of the symptoms, and the initiation of an adequate drug therapy in those patients. The main conclusions that can be drawn from the VOICES trial are summarized in Table 4.

Full table
Acknowledgements
This work was supported by Berlin-Chemie.
Footnote
Conflicts of Interest: LS Maier: Honoraria and Advisory Board for Berlin-Chemie and Gilead, grants and trials with Menarini and Gilead; U Wollenberg formerly was and R Limberg actually is employee at Berlin-Chemie; D Westermann: Honoraria by AstraZeneca, Berlin-Chemie, Bayer, Boeringer, Novartis; J Bauersachs: Honoraria by Berlin-Chemie. D Berliner and JD Schmitto have no conflicts of interest to declare.
References
- Federal Statistical Office of Germany. Health - Causes of death in Germany 2012. Wiesbaden, Germany: Federal Statistical Office of Germany, 2013:53.
- Patel MR, Peterson ED, Dai D, et al. Low diagnostic yield of elective coronary angiography. N Engl J Med 2010;362:886-95. [Crossref] [PubMed]
- Jespersen L, Abildstrom SZ, Hvelplund A, et al. Persistent angina: highly prevalent and associated with long-term anxiety, depression, low physical functioning, and quality of life in stable angina pectoris. Clin Res Cardiol 2013;102:571-81. [Crossref] [PubMed]
- Jespersen L, Abildstrom SZ, Hvelplund A, et al. Burden of hospital admission and repeat angiography in angina pectoris patients with and without coronary artery disease: a registry-based cohort study. PLoS One 2014;9:e93170. [Crossref] [PubMed]
- Humphries KH, Pu A, Gao M, et al. Angina with "normal" coronary arteries: sex differences in outcomes. Am Heart J 2008;155:375-81. [Crossref] [PubMed]
- Jespersen L, Hvelplund A, Abildstrom SZ, et al. Stable angina pectoris with no obstructive coronary artery disease is associated with increased risks of major adverse cardiovascular events. Eur Heart J 2012;33:734-44. [Crossref] [PubMed]
- Westermann D, Savvatis K, Wollenberg U, et al. Prevalence of obstructive coronary artery disease in patients with stable angina pectoris in Germany. J Clin Exp Cardiolog 2015;6:387.
- Ong P, Athanasiadis A, Borgulya G, et al. High prevalence of a pathological response to acetylcholine testing in patients with stable angina pectoris and unobstructed coronary arteries. The ACOVA Study (Abnormal COronary VAsomotion in patients with stable angina and unobstructed coronary arteries). J Am Coll Cardiol 2012;59:655-62. [Crossref] [PubMed]
- Camici PG, Crea F. Coronary microvascular dysfunction. N Engl J Med 2007;356:830-40. [Crossref] [PubMed]
- Knaapen P, Germans T, Camici PG, et al. Determinants of coronary microvascular dysfunction in symptomatic hypertrophic cardiomyopathy. Am J Physiol Heart Circ Physiol 2008;294:H986-93. [Crossref] [PubMed]
- Mohri M, Koyanagi M, Egashira K, et al. Angina pectoris caused by coronary microvascular spasm. Lancet 1998;351:1165-9. [Crossref] [PubMed]
- Monti LD, Piatti PM. Role of endothelial dysfunction and insulin resistance in angina pectoris and normal coronary angiogram. Herz 2005;30:48-54. [Crossref] [PubMed]
- Opherk D, Mall G, Zebe H, et al. Reduction of coronary reserve: a mechanism for angina pectoris in patients with arterial hypertension and normal coronary arteries. Circulation 1984;69:1-7. [Crossref] [PubMed]
- Rajappan K, Rimoldi OE, Camici PG, et al. Functional changes in coronary microcirculation after valve replacement in patients with aortic stenosis. Circulation 2003;107:3170-5. [Crossref] [PubMed]
- Lee BK, Lim HS, Fearon WF, et al. Invasive evaluation of patients with angina in the absence of obstructive coronary artery disease. Circulation 2015;131:1054-60. [Crossref] [PubMed]
- Halcox JP, Schenke WH, Zalos G, et al. Prognostic value of coronary vascular endothelial dysfunction. Circulation 2002;106:653-8. [Crossref] [PubMed]
- Working Committee for Health Services Research of the German Medical Association. Definition of Health Services Research. Berlin, Germany: The Working Committee, 2004:5.
- Campeau L.. Letter: Grading of angina pectoris. Circulation 1976;54:522-3. [PubMed]
- Mozaffarian D, Bryson CL, Spertus JA, et al. Anginal symptoms consistently predict total mortality among outpatients with coronary artery disease. Am Heart J 2003;146:1015-22. [Crossref] [PubMed]
- Shafiq A, Arnold SV, Gosch K, et al. Patient and physician discordance in reporting symptoms of angina among stable coronary artery disease patients: Insights from the Angina Prevalence and Provider Evaluation of Angina Relief (APPEAR) study. Am Heart J 2016;175:94-100. [Crossref] [PubMed]
- Montalescot G, Sechtem U, Achenbach S, et al. 2013 ESC guidelines on the management of stable coronary artery disease: the Task Force on the management of stable coronary artery disease of the European Society of Cardiology. Eur Heart J 2013;34:2949-3003. [Crossref] [PubMed]
- De Caterina AR, Galiuto L, Fedele E, et al. Microvascular dysfunction in the spectrum of coronary instability. Am J Cardiol 2011;108:1513-6. [Crossref] [PubMed]


