Intra-Thoracic Chemo-Hyperthermia for pleural recurrence of thymomas
Thymomas are rare thymic epithelial tumors (TETs) with favorable long-term prognosis after R0 resection surgery: 5-year overall disease-free survival is reported to range from 71% to 92% (1,2). Meanwhile, pleural relapse is a hallmark of thymoma (75% of recurrences) (3). Re-resection is a major predictor of favorable outcome in this setting and is recommend by the European Society for Medical Oncology (ESMO) and the National Comprehensive Cancer Network (NCCN). However, there is still no formal consensus on the surgical practice. Some authors advocate debulking surgery, complete re-resection, or extra pleural pneumonectomy (EPP) in selected patients associated with variable morbidity and mortality. Given indolent progression and specific localization of those recurrence, some authors advocate a new concept of radical cytoreductive surgery associated with Intra-Thoracic Chemo-Hyperthermia (ITCH) based on previous studies realized in mesothelioma.
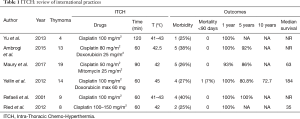
In 2017, we published our results of ITCH in 19 patients with pleural relapse of thymoma (4). These patients underwent surgical cytoreduction: sub-total pleurectomy associated with lung wedge resection (74%; N=14), EPP (5%; N=1). Our ITCH protocol included a 90-min at 42 °C perfusion of Cisplatin (50 mg/m2) and Mitomycin (25 mg/m2). There was no peri-operative death, 5 (26%) patients had post-operative complications. Two related with classical thoracic surgery and 3 related to systemic effects of chemotherapy (2 reversible acute kidney and 1 reversible bone marrow aplasia). The median disease-free interval and the five-year survival were respectively 42 months and 86%. Seven patients (37%) presented recurrence in pleura, mediastinal lymph nodes or pericardium. These results are fully compatible with the other published studies Table 1 (4-9).
Full table
Some point has to be discussed. First, this is a single institution retrospective study based on a small cohort with intrinsic selection bias. Inclusion criteria’s excluded ITCH for thymic carcinomas (TC) known to be more aggressive with poorer outcomes and with a trend to developed aggressive and systemic relapse on lymph nodes and solids organs. As TETs are rare tumor, an international multicentric study should be conducted to evaluate the real benefits of such therapy (surgery alone vs. surgery + ITCH). ITCH has to be done in expert centers involved in TET management. That is why, in France, a nationwide network for thymic malignancies was appointed in 2012 by the French National Cancer Institute, as part of its rare cancer program: RYTHMIC (Réseau tumeurs THYMiques et Cancer). Since then, all patients with a diagnosis of TETs have been discussed on real-time basis with a national multidisciplinary expert tumor board. This favors multi-team discussion for innovative surgery techniques, including ITCH. Second, the analysis of adverse effect of chemotherapy is challenging on small series. Our study pointed three adverse effects of local chemotherapy without possibilities to determinate risk factors. One of the 3 patients had one year before ITCH surgery of a large thymoma with innominate vein and pericardium removal (by mean of median sternotomy). During the ITCH procedure, given post-operative adherences, a right atrium wound was done, and repaired with classical stiches, which may facilitate systemic passage of anti-mitotic drugs. All publications referenced on ITCH relates classical complications of thoracic surgery such as prolonged air leak, hemorrhage wound complications, sepsis or cardiac atrial fibrillation. Compared to EPP, ITCH is less aggressive but cannot replace EPP which have to be discussed in high selected patients (10). Third, there is no consensus on the choice of drugs used in ITCH. A synergistic effect has been previously demonstrated with cisplatin and hyperthermia in pharmacokinetics studies. However, if cisplatin has been used by all centers involved in ITCH, the choice of a second drug was, in our study, based on the previous experiences in the treatment of peritoneal and pleural malignancies (11,12). Others authors used, doxorubicin or mitomycin. It is clear that laboratory investigations are needed to prove drug’s efficacy and it’s rational. TETs needs multidisciplinary approaches for the development of individualized treatment strategies (13,14).
Ultimately, the question is the value of outcomes after ITCH with thymoma relapse. It is well known that the metastatic course of thymoma is frequently indolent and patient could have long disease survival. Median local disease-free interval were respectively 63 and 53 months in Ambrogi et al. (5) and in our report (4), and median overall-survival were not reached in this two studies. However, after re-relapse, all patients were treated by systemic chemotherapy, or radiotherapy, which allowed long disease control. On a total of 67 patients reported in Table 1, 17 patients died: 6 from pneumonia or sepsis, 6 from related disease, 2 from second neoplasm, 1 secondary to systemic chemotherapy toxicity, 1 from pulmonary embolism and 1 from heart failure which confirm the specific indolent evolution of metastatic thymoma. Less than 50% of patients died from metastatic thymoma.
In our opinion, ITCH is a valuable therapy in well-selected patients, and shouldn’t be considered as standard but as one option that must be discussed on a multidisciplinary board in expert centers. Given the rarity of the disease, institutional experiences cannot determine the real impact of ITCH on survival and morbidity. The only consideration is that re-surgery is better than no surgery.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Demirci S, Turhan K, Ozsan N, et al. Prognostic factors for survival in patients with thymic epithelial tumors. Thorac Cardiovasc Surg 2011;59:153-7. [Crossref] [PubMed]
- Wilkins KB, Sheikh E, Green R, et al. Clinical and pathologic predictors of survival in patients with thymoma. Ann Surg 1999;230:562-72; discussion 572-4. [Crossref] [PubMed]
- Modh A, Rimner A, Allen PK, et al. Treatment Modalities and Outcomes in Patients With Advanced Invasive Thymoma or Thymic Carcinoma: A Retrospective Multicenter Study. Am J Clin Oncol 2016;39:120-5. [Crossref] [PubMed]
- Maury JM, Girard N, Tabutin M, et al. Intra-Thoracic Chemo-Hyperthermia for pleural recurrence of thymoma. Lung Cancer 2017;108:1-6. [Crossref] [PubMed]
- Ambrogi MC, Korasidis S, Lucchi M, et al. Pleural recurrence of thymoma: surgical resection followed by hyperthermic intrathoracic perfusion chemotherapydagger. Eur J Cardiothorac Surg 2016;49:321-6. [Crossref] [PubMed]
- Refaely Y, Simansky DA, Paley M, et al. Resection and perfusion thermochemotherapy: a new approach for the treatment of thymic malignancies with pleural spread. Ann Thorac Surg 2001;72:366-70. [Crossref] [PubMed]
- Ried M, Potzger T, Braune N, et al. Cytoreductive surgery and hyperthermic intrathoracic chemotherapy perfusion for malignant pleural tumours: perioperative management and clinical experience. Eur J Cardiothorac Surg 2013;43:801-7. [Crossref] [PubMed]
- Yellin A, Simansky DA, Ben-Avi R, et al. Resection and heated pleural chemoperfusion in patients with thymic epithelial malignant disease and pleural spread: a single-institution experience. J Thorac Cardiovasc Surg 2013;145:83-7; discussion 87-9. [Crossref] [PubMed]
- Yu L, Jing Y, Ma S, et al. Cytoreductive surgery combined with hyperthermic intrapleural chemotherapy to treat thymoma or thymic carcinoma with pleural dissemination. Onco Targets Ther 2013;6:517-21. [Crossref] [PubMed]
- Fabre D, Fadel E, Mussot S, et al. Long-term outcome of pleuropneumonectomy for Masaoka stage IVa thymoma. Eur J Cardiothorac Surg 2011;39:e133-8. [Crossref] [PubMed]
- Monneuse O, Beaujard AC, Guibert B, et al. Long-term results of intrathoracic chemohyperthermia (ITCH) for the treatment of pleural malignancies. Br J Cancer 2003;88:1839-43. [Crossref] [PubMed]
- Passot G, Vaudoyer D, Villeneuve L, et al. What made hyperthermic intraperitoneal chemotherapy an effective curative treatment for peritoneal surface malignancy: A 25-year experience with 1,125 procedures. J Surg Oncol 2016;113:796-803. [Crossref] [PubMed]
- Girard N, Merveilleux du Vignaux C. How large databases may impact clinical practices for rare tumors-postoperative chemotherapy in thymic malignancies. J Thorac Dis 2016;8:1863-4. [Crossref] [PubMed]
- Girard N, Ruffini E, Marx A, et al. Thymic epithelial tumours: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol 2015;26 Suppl 5:v40-55. [Crossref] [PubMed]


