Ectopic thymoma managed by neck dissection & video-assisted thoracoscopic thymectomy
Introduction
Thymomas are uncommon epithelial neoplasms of thymic origin, usually arising in the anterosuperior mediastinum, and are classically associated with myasthenia gravis (MG) (1). Ectopic thymoma in the neck is a rare phenomenon, likely a result of aberrant tissue migration during embryonic development, and comprises fewer than 2% of all thymoma cases (2). Ectopic cervical thymoma has been reported in 19 cases worldwide, with the bulk of this literature addressing the challenge of accurate diagnosis in an atypical neck mass.
The low index of suspicion and relatively asymptomatic clinical presentation makes ectopic cervical thymoma difficult to diagnose. The unique clinical features of this rare condition necessitate alternate approaches to diagnosis and management. However, in the existing reported cases of ectopic cervical thymoma, treatment plans have been extrapolated from data available for mediastinal thymoma management (2). Here we present a case of ectopic cervical thymoma, and suggest a diagnostic and therapeutic approach for this rare but important presentation.
Case presentation
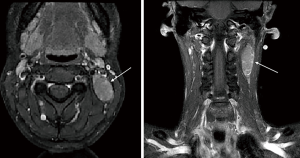
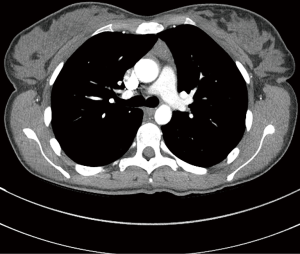
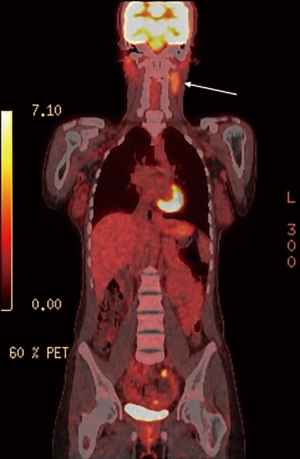
The patient was a 31-year-old, previously well, Afghan female first seen by her primary care physician for a newly identified, slow-growing left neck mass. Written informed consent was obtained from the patient for publication of this case report and any accompanying images. A fine needle aspiration (FNA) biopsy of the lesion was conducted, revealing thymoma. Computed tomography (CT) and magnetic resonance imaging (MRI) of the neck and chest revealed a 5 cm ectopic cervical thymoma, with concomitant mediastinal thymic enlargement concerning for thymic hyperplasia (Figures 1,2). FDG-PET demonstrated FDG-avidity of the left sided neck mass (Figure 3).
A multidisciplinary tumor board conference with thoracic as well as head and neck surgeons, medical oncologists, radiation oncologists, radiologists and pathologists was conducted, with concomitant review of the literature to direct management. Tumor board consensus recommendations involved a definitive combined otolaryngology and thoracic surgical approach.
The operation involved unilateral left neck dissection and excision of the suspected ectopic cervical thymoma, as well as a three-port video-assisted thoracoscopic surgery (VATS) complete thymectomy. The rationale for VATS thymectomy was that, given the finding of thymic enlargement concerning for hyperplasia on imaging, a mediastinal thymic primary with metastatic spread to the left cervical lymph node chain could not be excluded.
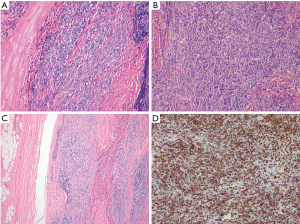
Pathology demonstrated a type AB thymoma composed of lymphocyte-poor spindle cell (type A) component (Figure 4A) and a lymphocyte-rich (type B2) component (Figure 4B), with a significant population of immature T cells. Extensive sampling and histologic examination of the capsule showed focal areas of microscopic invasion within the capsule, although no areas of transcapsular invasion were identified (Figure 4C). Immunohistochemistry is supportive of the histologic findings, with EMA positivity in the type A component and CK5 positivity in the type B2 component. TdT staining also highlights the immature T cells in the B2 component (Figure 4D). The lesion was completely excised, with no gross or microscopic involvement of the surgical margins. Based on these features, a modified Masaoka stage I was assigned. The mediastinal VATS thymectomy showed only thymic hyperplasia with no evidence of dysplasia on final surgical pathology.
Comments
The most frequently documented presentation of ectopic cervical thymoma has been that of an asymptomatic neck mass. MG is a common presentation in classical thymoma, affecting 30–50% of patients. MG is often an important clinical syndrome that demands CT chest screening in all patients on diagnosis to rule out associated thymoma, and may therefore be the first clinical sign of mediastinal thymoma. However, MG is not reliably associated with ectopic cervical thymoma, with the two having been reported together in only three cases in the literature (3-6). In the setting of ectopic cervical thymoma and typically diagnostic investigation is initiated because the lesion is allowed to reach a size that it becomes symptomatic by mass effect. Kondo et al. [2005] report the absence of MG in mediastinal thymoma to be associated with poor overall prognosis, concerning for outcomes in ectopic cervical thymoma (7). Asymptomatic non-resolving neck masses require prompt investigations, as delays in care may allow for progression of disease. Since thymomas tend to have limited response to chemotherapy or radiotherapy, neoadjuvant down-staging prior to surgery is not a viable option (1). Prompt excision is recommended, with delays increasing the risk of unrespectable tumor bulk and poor outcomes (1).
Histologic diagnosis of ectopic cervical thymoma may be challenging, especially if the pathologist is not considering this diagnosis. Many of the reported cases are in the pathology literature and describe the histologic features that distinguish ectopic cervical thymoma from epithelial or lymphomatous malignancies in the neck. FNA is the most commonly reported diagnostic technique in the reported cases of ectopic cervical thymoma. FNA is the recommended diagnostic approach of an asymptomatic neck mass, helping to narrow the broad differential (1,8).
The mainstay of therapy for thymoma is complete surgical excision, as effective cure from chemoradiation has not been reliably demonstrated. In ectopic thymoma the approach for surgical excision is described on a case-by-case basis given its rarity, and should be discussed at a multidisciplinary tumour board to ensure optimal patient care. While multiple surgical techniques have been reported, they range widely in approach and extent. Our minimally invasive approach involving unilateral neck dissection and VATS thymectomy has not yet been described in the available literature. Yokoyama et al. [2015] recently published a similar case of ectopic cervical thymoma, which was treated with an open neck dissection and a single-port VATS mediastinal thymectomy via trans-cervical approach, taking advantage of their extensive neck dissection (9). Wu et al. [2011] described an open trans-cervical thymomectomy with trans-sternal thymectomy for a case of ectopic cervical thymoma (3). Thymectomy is not routinely described in ectopic thymoma management, though (5,6). The choice to perform a neck dissection and a separate VATS thymectomy, rather than the combined open approach described by Yokoyama et al. [2015], was made to use as minimally invasive an approach as possible, while ensuring complete excision of all thymic tissue (9). We encourage that cases for ectopic thymoma employ a minimally-invasive approach and undergo a VATS thymectomy plus local excision of the ectopic thymoma.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this manuscript with accompanying images.
References
- Tomaszek S, Wigle DA, Keshavjee S, et al. Thymomas: review of current clinical practice. Ann Thorac Surg 2009;87:1973-80. [Crossref] [PubMed]
- Weissferdt A, Moran CA. The spectrum of ectopic thymomas. Virchows Arch 2016;469:245-54. [Crossref] [PubMed]
- Wu TH, Jin JS, Huang TW, et al. Ectopic cervical thymoma in a patient with myasthenia gravis. J Cardiothorac Surg 2011;6:89. [Crossref] [PubMed]
- Mineo TC, Biancari F, D'Andrea V. Myasthenia gravis, psychiatric disturbances, idiopathic thrombocytopenic purpura, and lichen planus associated with cervical thymoma. J Thorac Cardiovasc Surg 1996;111:486-7. [Crossref] [PubMed]
- Choi H, Koh SH, Park MH, et al. Myasthenia gravis associated with ectopic cervical thymoma. J Clin Neurosci 2008;15:1393-5. [Crossref] [PubMed]
- Milde P, Sidawy MK. Thymoma presenting as a palpable thyroid nodule: a pitfall in fine needle aspiration (FNA) of the neck. Cytopathology 1999;10:415-9. [Crossref] [PubMed]
- Kondo K, Monden Y. Thymoma and myasthenia gravis: a clinical study of 1,089 patients from Japan. Ann Thorac Surg 2005;79:219-24. [Crossref] [PubMed]
- Haynes J, Arnold KR, Aguirre-Oskins C, et al. Evaluation of neck masses in adults. Am Fam Physician 2015;91:698-706. [PubMed]
- Yokoyama S, Hayashida R, Yoshiyama K, et al. Ectopic cervical thymoma excised through a transcervical approach combined with video-assisted thoracoscopic surgery: a case report. Ann Thorac Cardiovasc Surg 2015;21:293-7. [Crossref] [PubMed]


