The lion and the unicorn were fighting for the crown: on-pump versus off-pump coronary-artery bypass grafting
“…, in the middle of which the Lion and Unicorn were fighting.
…, that at first Alice could not make out which was which: but she soon managed to distinguish the Unicorn by his horn.”
Numerous studies [including randomized controlled trials (RCTs)] have compared outcomes following off-pump coronary-artery bypass grafting (CABG) with those following on-pump CABG, which appears that, as it were, “the Lion and the Unicorn were fighting for the crown” (Figure 1). Recently, the Randomized On/Off Bypass (ROOBY) Follow-up Study (ROOBY-FS) (1) reported 5-year clinical outcomes in 2,203 patients randomly assigned to off-pump (1,104 patients) or on-pump CABG (1,099 patients). At 5 years, off-pump CABG was inferior to on-pump CABG with regard to death from any cause [15.2% vs. 11.9%; relative risk (RR), 1.28; 95% confidence interval (CI), 1.03–1.58; P=0.02; hazard ratio (HR), 1.30; 95% CI, 1.04–1.64; P=0.02] and the primary composite major adverse cardiovascular events outcome (RR, 1.14; 95% CI, 1.00–1.30; P=0.046; HR, 1.18; 95% CI, 1.01–1.38; P=0.03). Has the Lion (on-pump CABG) beaten the Union (off-pump CABG)?

The 5-year rate of death from cardiac causes did not differ significantly between off- and on-pump CABG (6.3% vs. 5.3%; RR, 1.20; 95% CI, 0.86–1.68; P=0.29) in the ROOBY-FS (1). Accordingly, the significantly higher rate of death from any cause following off-pump (15.2%) than on-pump CABG (11.9%) was not correspondingly reflected in no significantly different rate of death from cardiac causes between treatments. The discrepancy between the significant difference of all-cause mortality and no difference of cardiac mortality in the ROOBY-FS (1) is in accordance with 5-year results of another RCT, i.e., the Best Bypass Surgery (BBS) trial (2). In the BBS trial (2), although all-cause mortality was significantly higher following off-pump than on-pump CABG (HR, 1.66; 95% CI, 1.02–2.73; P=0.04), cardiac mortality was similar between off-pump and on-pump CABG (10% vs. 7%; HR, 1.30; 95% CI, 0.64–2.66; P=0.47) (2). Because the cause of death may have several competitive factors in high-risk patients and death from cardiac causes is always challenging to adjudicate, the reliability of assessing cardiac causes of death has been much debated and all-cause mortality must be the most unbiased outcome (1,2).
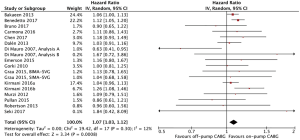
A number of meta-analyses (3-5) have confirmed the results of the ROOBY-FS (1). A meta-analysis (3) demonstrated that off-pump CABG increased short-term (≥1-year) [18 RCTs enrolling a total of 5,358 patients; pooled odds ratio (OR), 1.35; 95% CI, 1.07–1.70; P=0.01] and midterm (≥3-year) all-cause mortality (7 RCTs enrolling a total of 1,826 patients; pooled OR, 1.36; 95% CI, 1.02–1.80; P=0.01). Another meta-analysis (4) of 5 RCTs and 17 adjusted observational comparative studies enrolling a total of 104,306 patients also indicated that long-term (≥5-year) all-cause mortality was higher following off-pump CABG (pooled HR, 1.07; 95% CI, 1.03–1.11; P=0.0003). Furthermore, a recent meta-analysis (5) of 16 propensity score-matched observational comparative studies enrolling a total of 82,316 patients suggested that very long-term (≥10 years) all-cause mortality was higher in off-pump CABG (pooled HR, 1.07; 95% CI, 1.03–1.12; P=0.0008; Figure 2). Off-pump CABG should not be generally considered as the first choice for surgical revascularization, because the greatest clinical benefit for patients undergoing surgical coronary revascularization is surely a reduction in follow-up mortality.
Fewer numbers of distal anastomoses (6) and lower rates of graft patency (7) may explain higher follow-up mortality following off-pump than on-pump CABG, because complete revascularization is associated with lower mortality than incomplete revascularization in patients with multivessel disease (MVD) (8). A Cochrane meta-analysis (6) of 57 RCTs enrolling a total of 7,071 patients showed that fewer distal anastomoses were performed in off-pump CABG (pooled mean difference, −0.28; 95% CI, −0.40 to −0.16, P<0.00001). Another meta-analysis (7) of 12 RCTs (a total of 3,894 and 4,137 grafts in off- and on-pump CABG, respectively) found increases in occlusion of all grafts (pooled RR 1.35, 95% CI, 1.16–1.57, P<0.001) and saphenous vein grafts (pooled RR 1.41, 95% CI, 1.24–1.60, P<0.001) in the off-pump CABG. On the other hand, a meta-analysis (8) of adjusted HRs from 14 observational studies enrolling a total of 30,389 patients with MVD demonstrated that follow-up all-cause mortality was significantly lower following complete- than incomplete-revascularization CABG (pooled HR 0.63, 95% CI, 0.53–0.75, P<0.00001).
It may be time, however, to focus on identifying which patients benefit from which procedure, i.e., off-pump CABG is probably better for some patients and on-pump CABG for others (9). For example, off-pump CABG may be superior for elderly patients (10), octogenarians (11), and patients with chronic kidney disease (CKD) (12). First, in a meta-analysis (10) of 3 RCTs and 20 non-RCTs with a total of 12,697 ≥70-year patients, there was a reduced chance of overall mortality (from 30-day to 10-year follow-up) in patients who received off-pump CABG compared with on-pump CABG (pooled OR, 0.744; 95% CI, 0.587–0.944; P=0.015). Second, a meta-analysis (11) of 14 non-randomized retrospective observational studies involving 18,840 patients demonstrated that octogenarians undergoing off-pump CABG experienced lower in-hospital mortality (pooled OR, 0.64; 95% CI, 0.44–0.93; P=0.02). Third, a meta-analysis (12) of 16 retrospective observational studies and one RCT represented that short-term (30-day) mortality in CKD patients was significantly lower following off-pump CABG (15 studies enrolling a total of 196,522 patients; pooled OR, 0.88; 95% CI, 0.82–0.93; P<0.0001) as well as in end-stage renal disease patients (11 studies enrolling a total of 14,013 patients; pooled OR, 0.80; 95% CI, 0.70–0.93; P=0.003). The improved perioperative mortality (11,12) following off-pump CABG in these patients may translate to equivalent or more favorable (to or than on-pump CABG) survival in long-term follow-up.
“‘Does—the one—that wins—get the crown?’ she asked, ….
‘Dear me, no!’ said the King. ‘What an idea!’”
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Shroyer AL, Hattler B, Wagner TH, et al. Five-year outcomes after on-pump and off-pump coronary-artery bypass. N Engl J Med 2017;377:623-32. [Crossref] [PubMed]
- Møller CH, Perko MJ, Lund JT, et al. Three-year follow-up in a subset of high-risk patients randomly assigned to off-pump versus on-pump coronary artery bypass surgery: the Best Bypass Surgery trial. Heart 2011;97:907-13. [Crossref] [PubMed]
- Takagi H, Yamamoto H, Iwata K, et al. Ask not which can impair early morbidity--ask which can improve late survival: a meta-analysis of randomized trials of off-pump versus on-pump coronary artery bypass. Int J Cardiol 2012;158:435-8. [Crossref] [PubMed]
- Takagi H, Umemoto T. All-Literature Investigation of Cardiovascular Evidence (ALICE) Group. Worse long-term survival after off-pump than on-pump coronary artery bypass grafting. J Thorac Cardiovasc Surg 2014;148:1820-9. [Crossref] [PubMed]
- Takagi H, Ando T, Mitta S, et al. Meta-analysis comparing ≥10-year mortality of off-pump versus on-pump coronary artery bypass grafting. Am J Cardiol 2017;120:1933-8. [Crossref] [PubMed]
- Møller CH, Penninga L, Wetterslev J, et al. Off-pump versus on-pump coronary artery bypass grafting for ischaemic heart disease. Cochrane Database Syst Rev 2012.CD007224. [PubMed]
- Zhang B, Zhou J, Li H, et al. Comparison of graft patency between off-pump and on-pump coronary artery bypass grafting: an updated meta-analysis. Ann Thorac Surg 2014;97:1335-41. [Crossref] [PubMed]
- Takagi H, Watanabe T, Mizuno Y, et al. A meta-analysis of adjusted risk estimates for survival from observational studies of complete versus incomplete revascularization in patients with multivessel disease undergoing coronary artery bypass grafting. Interact Cardiovasc Thorac Surg 2014;18:679-82. [Crossref] [PubMed]
- Blackstone EH, Sabik JF 3rd. Changing the discussion about on-pump versus off-pump CABG. N Engl J Med 2017;377:692-3. [Crossref] [PubMed]
- Zhu ZG, Xiong W, Ding JL, et al. Comparison of outcomes between off-pump versus on-pump coronary artery bypass surgery in elderly patients: a meta-analysis. Braz J Med Biol Res 2017;50:e5711. [Crossref] [PubMed]
- Khan H, Uzzaman M, Benedetto U, et al. On- or off-pump coronary artery bypass grafting for octogenarians: A meta-analysis of comparative studies involving 27,623 patients. Int J Surg 2017;47:42-51. [Crossref] [PubMed]
- Wang Y, Zhu S, Gao P, et al. Off-pump versus on-pump coronary surgery in patients with chronic kidney disease: a meta-analysis. Clin Exp Nephrol 2017. [Epub ahead of print]. [Crossref] [PubMed]


