Management of partial anomalous pulmonary venous connections in patients requiring pulmonary resection: a case report and systematic review
Background
Partial anomalous pulmonary venous connections (PAPVCs) are a heterogeneous group of rare vascular malformations that describe incomplete connections from the pulmonary venous system to the systemic venous system or right heart. PAPVCs are encountered in approximately 0.5% of the pediatric population, where they are commonly associated with atrial septal defects (ASDs) (1). Within this cohort, treatment often requires operative repair (1). In the adult population, PAPVCs are exceedingly rare, thus disease-specific epidemiology and treatment protocols are undefined. Management of PAPVCs becomes a therapeutic dilemma when circulatory physiology may be rapidly altered, for example, during pulmonary resection. In this report, we highlight physiologic considerations of PAPVCs in the adult population by documenting our experiences involving a patient who presented with a suspicious pulmonary nodule and PAPVC. In addition to these comments, we provide a systematic review consisting of all contemporary reports describing management of PAPVCs in the patient undergoing resection for suspicious pulmonary lesions.
Case report
A 70-year-old male former smoker presented to our clinic for evaluation of an incidentally discovered 1.9 cm ground-glass opacity (GGO) of the right upper lobe (Figure 1A). Upon interview, the patient denied associated symptomatology. A preoperative PET-CT was obtained and revealed a standardized uptake value (SUV) of 4.9 (Figure 1B), and no suspicious lymph node involvement. The lesion was not amenable to transthoracic or endobronchial biopsy, thus the patient was consented for a video-assisted thoracic surgery (VATS) wedge biopsy. During initial dissection, an anomalous vein arising from the right superior pulmonary vein and draining into the superior vena cava was identified (Figure 1C). Intraoperative review of a previous contrast enhanced chest CT confirmed partial anomalous pulmonary vein (Figure 1D,E,F), and revealed no other cardiopulmonary abnormalities.
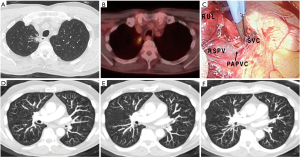
Because the anomalous vein was associated with the lobe harboring the preoperatively identified GGO, the decision was made to proceed with resection without additional cardiopulmonary evaluation. A right upper lobectomy was performed, with ligation of the anomalous vein near the vena cava. After sampling lymph nodes for staging, the case was concluded in standard fashion. A postoperative echocardiogram was obtained, and ruled out septal defects. The patient is now 6 months from his procedure without evidence of cardiopulmonary compromise or disease recurrence.
Discussion
PAPVCs are rare congenital anomalies found in 0.4–0.7% of the population at autopsy (2). These anomalies are most frequently identified in children, where they are typically right sided and are associated with ASDs in 80–90% of cases (1,2). In the pediatric population, repair is indicated when pulmonary-to-systemic flow ratio (Qp/Qs) approaches 1.5 (2,3).
In contrast, PAPVCs in adults, particularly when associated with pulmonary nodules, are far less common with only 24 cases being reported to date (data summarized in Table 1). Given the rare presentation of PAPVCs in adults requiring pulmonary resection, treatment approaches are not established. Despite a small sample size, epidemiologic and therapeutic trends may be ascertained from systematic analysis of adult reports.
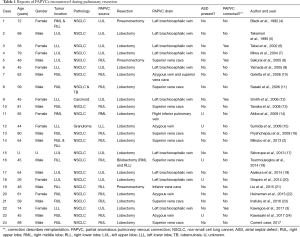
Full table
Upon review, the mean age of presentation of patients with PAPVCs and pulmonary nodules was found to be 59 years (SD 14 years). There appears to be no gender predominance (44% female, 56% male) nor laterality predisposition (46% are left-sided, 54% are right-sided). Approximately half of PAPVCs are found preoperatively with the other half found intraoperatively (3). The most common drainage patterns in adults involve connections from the left superior pulmonary vein to the innominate vein (41.6%) and the right superior pulmonary vein to the superior vena cava (29.1%). Perhaps most interestingly, although PAPVCs are highly associated with ASDs in the pediatric population, there are no reports of adult patients with a PAPVC and lung nodules who have been found to have an ASD. These data may suggest that additional studies aimed at assessing septal abnormalities are of little added utility.
Management of PAPVCs in the setting of pulmonary resection requires careful consideration of several factors including PAPVC anatomy, preoperative cardiopulmonary physiology (as assessed by Qp/Qs), and the extent of planned pulmonary resection. For PAPVCs that arise from a pulmonary segment that will be included in the resection specimen, simple ligation is adequate. In fact, some reports suggest that resection may result in improvements of pulmonary hypertension (19).
When a PAPVC arises from an anatomic segment which will not be included in the resection, the management approach is more challenging and requires a pre-resection assessment of Qp/Qs and consideration of resection extent. These factors are important as significant pulmonary resections in patients with elevated Qp/Qs ratios can result in fulminant right-heart failure due to acute increases in shunt fraction through the PAPVC and elevated pulmonary arterial pressures (3,4). Although a clear Qp/Qs cut-off is unknown, patients with Qp/Qs greater than 1.5 or symptomatic PAPVCs are at high risk for post-operative complications, and thus should undergo PAPVC repair. Successful PAPVC repair has been described both prior to and during pulmonary resection with good success (3,6,8,12). For patients with asymptomatic PAPVCs and normal Qp/Qs, standard pulmonary resection is likely sufficient. Finally, in patients with lesser resections and borderline Qp/Qs (ranging from 1.0 to 1.5), it remains unclear if PAPVC correction is necessary with reports demonstrating success with both approaches (9,12,18). A summary of this treatment algorithm is provided in Figure 2.

Although these data provide a basic blueprint for both diagnostic and therapeutic approaches for the rare patient presenting with PAPVCs and resectable pulmonary nodules, some potential limitations should be noted. First, the compiled data is based almost exclusively on single case reports from a variety of centers across the world. This methodology introduces heterogeneity in the treatment approach and limits interpretation of long term follow-up data. Second, there is no randomization or control group which can complicate outcome interpretation. Finally, the prevalence of PAPVCs is likely underestimated as nearly half of these anomalies were found only intraoperatively during resection. Evaluation of the contralateral hemithorax is thus impossible during resection. Nevertheless, these results represent the first formal review characterizing trends and provides an applicable treatment algorithm for this challenging cohort.
In summary, management of PAPVCs during resection is an uncommon clinical scenario that requires careful consideration of venous anatomy, preoperative cardiopulmonary physiology, and resection extent. For patients with PAPVCs arising from the pulmonary segment to be included in the resection specimen, simple vein ligation is appropriate. For those patients with PAPVCs arising from pulmonary segments which will not be included in the resection, consideration of preoperative Qp/Qs and resection extent is essential when determining the need for PAPVC correction.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
References
- Said SM, Burkhart HM, Schaff HV, et al. Single-patch, 2-patch, and caval division techniques for repair of partial anomalous pulmonary venous connections: does it matter? J Thorac Cardiovasc Surg 2012;143:896-903. [Crossref] [PubMed]
- Mikubo M, Ikeda S, Hoshino T, et al. Pulmonary resection of lung cancer in a patient with partial anomalous pulmonary venous connection. Ann Thorac Surg 2013;95:1799-801. [Crossref] [PubMed]
- Kawagoe I, Hayashida M, Nozumi Y, et al. A combination of a partial anomalous pulmonary venous connection (PAPVC) and a lung tumor requiring pulmonary resection. J Cardiothorac Vasc Anesth 2017;31:274-8. [Crossref] [PubMed]
- Black MD, Shamji FM, Goldstein W, et al. Pulmonary resection and contralateral anomalous venous drainage: a lethal combination. Ann Thorac Surg 1992;53:689-91. [Crossref] [PubMed]
- Takamori S, Hayashi A, Nagamatsu Y, et al. Left partial anomalous pulmonary venous connection found during a lobectomy for lung cancer: report of a case. Surg Today 1995;25:982-3. [Crossref] [PubMed]
- Takei H, Suzuki K, Asamura H, et al. Successful pulmonary resection of lung cancer in a patient with partial anomalous pulmonary venous connection: report of a case. Surg Today 2002;32:899-901. [Crossref] [PubMed]
- Miwa K, Takamori S, Hayashi A, et al. Incidental partial anomalous pulmonary venous connection in left lung cancer. Jpn J Thorac Cardiovasc Surg 2004;52:189-90. [Crossref] [PubMed]
- Sakurai H, Kondo H, Sekiguchi A, et al. Left pneumonectomy for lung cancer after correction of contralateral partial anomalous pulmonary venous return. Ann Thorac Surg 2005;79:1778-80. [Crossref] [PubMed]
- Yamada M, Koshika M, Goto S, et al. Lung cancer which accompanies anomalous venous connections, pulmonary and systemic-partial anomalous pulmonary venous connection and persistent left superior vena cava: report of 2 cases. Kyobu Geka 2005;58:399-402. [PubMed]
- Galetta D, Veronesi G, Leo F, et al. Anomalous right upper lobe venous drainage. Ann Thorac Surg 2006;82:2272-4. [Crossref] [PubMed]
- Sasaki H, Naka N, Kitahara N, et al. Right partial anomalous pulmonary venous connection found during lobectomy for coexisting lung cancer and tuberculosis: report of a case. Clin Lung Cancer 2006;7:350-2. [Crossref] [PubMed]
- Smith RL 2nd, Zorn GL 3rd, Peeler BB, et al. Combined bronchial sleeve resection and repair of partial anomalous pulmonary venous return. J Thorac Cardiovasc Surg 2006;132:982-3. [Crossref] [PubMed]
- Tanaka R, Nakazato Y, Fukura H, et al. Partial anomalous pulmonary venous connection in right lung cancer: report of a case. Surg Today 2008;38:147-9. [Crossref] [PubMed]
- Akiba T, Marushima H, Harada J, et al. Anomalous pulmonary vein detected using three-dimensional computed tomography in a patient with lung cancer undergoing thoracoscopic lobectomy. Gen Thorac Cardiovasc Surg 2008;56:413-6. [Crossref] [PubMed]
- Sumida K, Kohno T, Mun M, et al. A lung granuloma with partial anomalous pulmonary venous connection and bronchial atresia. J Thorac Cardiovasc Surg 2008;135:449-50. [Crossref] [PubMed]
- Pryshchepau M, Gossot D, Strauss C, et al. Anomalous partial pulmonary venous drainage. Eur J Cardiothorac Surg 2009;36:933. [Crossref] [PubMed]
- Szkorupa M, Bohanes T, Chudáček J, et al. Anomalous venous drainage of the lung to the brachiocephalic vein. Eur J Cardiothorac Surg 2013;44:768. [Crossref] [PubMed]
- Tourmousoglou C, Kalogeropoulou C, Koletsis E, et al. Right upper lobe partial anomalous pulmonary venous connection. Case Rep Vasc Med 2014;2014:249896. [Crossref] [PubMed]
- Asakura K, Izumi Y, Kohno M, et al. Partial anomalous pulmonary venous connection associated with lung cancer in the same lobe: report of a case. Ann Thorac Cardiovasc Surg 2014;20:457-60. [Crossref] [PubMed]
- Shapiro M, Bittermann C, Flores RM. Anomalous pulmonary vein drainage is not a contraindication for VATS lobectomy. Thorac Cardiovasc Surg 2014;62:255-7; discussion 257. [Crossref] [PubMed]
- Liu Z, Yang R, Shao F, et al. Ipsilateral partial anomalous pulmonary venous connection in right lung cancer with absent right upper lobe. World J Surg Oncol 2015;13:104. [Crossref] [PubMed]
- Heineman DJ, van den Aardweg JG, Schreurs WH. A rare case of anomalous venous drainage of the right upper lobe. J Thorac Dis 2015;7:E502-4. [PubMed]
- Inafuku K, Morohoshi T, Adachi H, et al. Thoracoscopic lobectomy for lung cancer in a patient with a partial anomalous pulmonary venous connection: a case report. J Cardiothorac Surg 2016;11:113. [Crossref] [PubMed]
- Kawasaki H, Oshiro Y, Taira N, et al. Partial anomalous pulmonary venous connection coexisting with lung cancer: a case report and review of relevant cases from the literature. Ann Thorac Cardiovasc Surg 2017;23:31-5. [Crossref] [PubMed]


