Chest drainage systems and management of air leaks after a pulmonary resection
Introduction
The most frequent complication following a pulmonary resection is an alveolar air leak (1). Approximately 30–50% of patients present with one postoperatively and are the most important determinant of length of hospital stay (LOS) (1,2). A few hours postoperatively, some air leaks spontaneously resolve but others can last for many days. In approximately 8–15% of patients, an air leak can last longer than 5 days which is considered a prolonged air leak (PAL) by definition of the Society of Thoracic Surgeons Database (1-3). A PAL complicates postoperative recovery with associated poorer outcomes and increased morbidity (1,3). Factors associated with increased hospital costs and length of stay after a pulmonary resection are PALs, inadequate pain management and postoperative chest tube duration (2). There is increased pressure by hospitals and insurance companies to standardize care and optimize post-operative recovery. Digital chest drainage systems provide continuous monitoring of air leak flow that provides quantifiable, reproducible and objective data (2). Evaluating the air leak flow can allow clinicians to more rapidly differentiate between patients with indications of a PAL and those who may benefit from fast-tracked care (2,4). In contrast, the traditional chest drainage system air leak assessment is instantaneous and subjective by observing the water seal column for bubbling. In the traditional system, suction is obtained from the wall and the degree of negative pressure may vary from the set level due to the fluid in the tubing and where the drainage system is placed in relation to the patient (5). The aim of this paper is to evaluate two different chest drainage systems with air leak management after pulmonary resections and identify gaps in the research that could help standardize postoperative care.
Methods
Five databases were used in this search: PubMed, Cochrane Central Register of Controlled Trials, European Journal of Cardiothoracic Surgery, Interactive CardioVascular and Thoracic Surgery Journals and U.S. National Library of Medicine. The search terms used were: air leak, digital and thoracic surgery. These three words were used in each of the databases searched. There was no modification necessary for the individual databases.
Articles were included if they addressed air leak evaluation with the different chest drainage systems. Either independently evaluating the air leak with one drainage system or comparing the two devices was allowed. The drainage systems had to be evaluated on post-operative thoracic surgical patients. The articles were peer-reviewed, in English and published from 2002 to 2017.
Articles were excluded if they were review, commentary or editorial articles. Air leaks due to medical reasons such as: tracheobronchial stenosis, bronchopleural fistula and spontaneous pneumothorax were left out. Air leak evaluation using different intra-operative tissue sealants, suction versus water seal, endobronchial valve implantation, how many chest tubes used after surgery and evaluation of postoperative air leaks that did not include the chest drainage systems were discarded. Different types of surgical technique (video-assisted thoracoscopic surgery vs. open lobectomies) used to evaluate air leaks were also excluded.
Search results
Database searches returned 277 articles, and all were screened to determine their relevancy. Thirteen were duplicates and removed. Another 225 articles were excluded after abstract review revealed they did not meet inclusion or met exclusion criteria. Full review was completed on 39 articles and 18 of those were included in the final analysis.
Synthesis of the research
Chest drainage systems differ with regard to the information produced for clinicians. Management of air leaks after pulmonary resections can vary depending on physician preference and scientific data. Many factors influence the decision to remove chest tubes and how PALs are evaluated and managed. These factors greatly influence hospital length of stay, postoperative pain and number of chest tube days.
Apical spaces and PALs after a pulmonary resection
After a pulmonary lobectomy, an expected finding is a postresection apical space. This residual space does not have clinical significance unless the patient is symptomatic (1). Upper lobectomies have a higher incidence of air space problems than other lobar resections. Initially after surgery, the remaining lung tissue does not fill the pleural space volume and match the hemithorax shape (1,6). Physiological changes that occur to fill the space are shift of the mediastinum, diaphragm elevation, ipsilateral lung hyperinflation and narrowing of the intercostal spaces (1,6).
Many factors contribute to the size of an air leak such as the condition of the lung parenchyma and position of the chest tube (7). Risk factors for a PAL include: chronic obstructive pulmonary disease (COPD), bilobectomy, upper lobectomy, diffusing capacity of carbon monoxide (DLCO) less than 80% predicted and steroid use (3,8). Postoperative air leaks are not just an annoyance that prolongs hospitalization; they can be a surrogate marker for increased morbidity and complications like postoperative atrial fibrillation and pneumonia (9).
The LOS averages 5 to 13 days with a PAL since most patients remain in the hospital until the air leak resolves (8,10). Only a small percentage of patients can be discharged from the hospital and go home with a portable chest drainage system (10). The potential complications from a PAL include pneumonia, atelectasis, empyema and longer chest tube days (2,8,11).
Digital chest drainage systems
Digital chest drainage systems have also provided a much more accurate air leak reading. These systems provide quantifiable information and continuous monitoring of postoperative air leak flow rates (5,10,11). Digital systems provide reproducible data, eliminate subjective interpretation, decrease interobserver variability, and increase observer agreement rates for chest tube removal (5,10,11).
The digital system works by maintaining the intrapleural pressure at a steady level within 0.1 cmH2O. Maintaining a consistent pressure with minimal oscillations, may promote the sealing of air leaks (5). The regulated suction adjusts according to the condition or need in the pleural cavity. The device will apply suction to keep the pleural cavity at the present level. If the patient does have an air leak with suction, the device will intermittently apply suction to restabilize the pleural space according to the degree of the air leak (12). Thopaz (Medela®, Baar, Switzerland), a digital chest drainage system recommends removal of the chest tube when air leak flow is less than 50 mm/min without large variation for the prior 6–12 hours.
Interobserver variability
The digital system has demonstrated decreased interobserver variability when deciding to remove chest tubes. It objectifies much of the subjective information and can be replicated among several observers (9). The level of agreement significantly increased in nurses, surgeons and residents (11,13-15). This system enables the health care team, regardless of their experience or level of education, to accurately report the status a patient’s air leak (9,14).
There is interobserver variability and assessment with a traditional system can be error prone (9,14). With differing opinions among clinicians and the inability to accurately ascertain an improving air leak, can lead to longer chest tube days and increased LOS. If chest tubes are removed prematurely because of an inaccurate reading, there may be a subsequent need for chest tube reinsertion (14).
Gap analysis
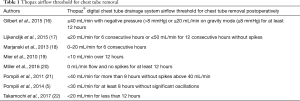
In the majority of the research studies there were inconsistent airflow rates in the digital drainage system or a dedicated number of hours before chest tubes were removed. Table 1 provides eight studies and their flow threshold for chest tube removal with the Thopaz® digital system after a pulmonary resection which shows wide variation when chest tubes are removed.
Full table
After a pulmonary resection, there is no agreement in the number of chest tubes, whether suction should or should not be used or if chest tubes should be clamped before removal (10,13,14). Variation in clinical practice is an important determinant that can lengthen hospital stay. Improving and maintaining consistency in air leak assessment can lead to a more timely removal of chest tubes with a shorter LOS. The wide variation in air leak flow in the digital systems before removal adds to the complication of chest tube management.
Currently there have been no studies evaluating robotic-assisted pulmonary resections and air leak assessment with the digital or traditional chest drainage systems. Robotic surgery uses 3-dimensional, high-definition visualization allowing surgeons to intuitively perform complex resections (23). The accuracy and advanced imaging provided by the daVinci® robot offsets the reduced tactile feedback missing in robotic surgery (23). Evaluating the traditional and digital chest drainage systems with robotic surgery would provide more information for the thoracic surgery team, using a different surgical approach, to assist in patient care postoperatively.
In the digital drainage system, implementing a consistent and reliable flow level for a specified time that could be used by all surgeons would remove all the variations that currently exist. These recommendations could only be implemented if surgeons removed their opinions and supported the scientific research.
Future research
There has been a lot of research with the new technology in chest drainage systems. There is much more to be examined to translate the research into practice and incorporate new standards of care.
Practice
- Standardizing chest tube management based on scientific data versus clinician preference;
- Educating clinical staff on air leak assessment with digital and traditional systems to decrease variability of findings;
- Evaluating patients early postoperatively for signs of a PAL to assist with discharge planning.
Research
- Clinical trials to evaluate safe air leak flow thresholds to remove chest tubes;
- Satisfaction evaluation and learning curves with clinical staff using new technology;
- Evaluation of chest drainage systems with robotic-assisted pulmonary resections.
Once this research is complete, chest tube management will have less variation with either the digital or traditional chest drainage systems. Clinicians will be more educated on air leaks and how to efficiently and safely care for patients postoperatively.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Mueller MR, Marzluf BA. The anticipation and management of air leaks and residual spaces post lung resection. J Thorac Dis 2014;6:271-84. [PubMed]
- Brunelli A, Cassivi SD, Halgren L. Risk factors for prolonged air leak after pulmonary resection. Thorac Surg Clin 2010;20:359-64. [Crossref] [PubMed]
- Burt BM, Shrager JB. The prevention and management of air leaks following pulmonary resection. Thorac Surg Clin 2015;25:411-9. [Crossref] [PubMed]
- Bryant AS, Cerfolio RJ. The influence of preoperative risk stratification on fast-tracking patients after a pulmonary resection. Thorac Surg Clin 2008;18:113-8. [Crossref] [PubMed]
- Pompili C, Detterbeck F, Papagiannopoulos K, et al. Multicenter international randomized comparison of objective and subjective outcomes between electronic and traditional chest drainage systems. Ann Thorac Surg 2014;98:490-6. [Crossref] [PubMed]
- Okur E, Kir A, Halezeroglu S, et al. Pleural tenting following upper lobectomies or bilobectomies of the lung to prevent residual air space and prolonged air leak. Eur J Cardiothorac Surg 2001;20:1012-5. [Crossref] [PubMed]
- Brunelli A, Salati M, Refai M, et al. Evaluation of a new chest tube removal protocol using digital air leak monitoring after lobectomy: a prospective randomised trial. Eur J Cardiothorac Surg 2010;37:56-60. [Crossref] [PubMed]
- Liang S, Ivanovic J, Gilbert S, et al. Quantifying the incidence and impact of postoperative prolonged alveolar air leak after pulmonary resection. J Thorac Cardiovasc Surg 2013;145:948-54. [Crossref] [PubMed]
- Cerfolio RJ, Varela G, Brunelli A. Digital and smart chest drainage systems to monitor air leaks: the birth of a new era? Thorac Surg Clin 2010;20:413-20. [Crossref] [PubMed]
- Brunelli A, Cassivi SD, Salati M, et al. Digital measurements of air leak flow and intrapleural pressures in the immediate postoperative period predict risk of prolonged air leak after pulmonary lobectomy. Eur J Cardiothorac Surg 2011;39:584-8. [Crossref] [PubMed]
- Cerfolio RJ, Bryant AS. The benefits of continuous and digital air leak assessment after elective pulmonary resection: a prospective study. Ann Thorac Surg 2008;86:396-401. [Crossref] [PubMed]
- Thopaz Digital Chest Drainage System. Medela, 2011. Available online: http://www.medela-healthcare.us/healthcare/products/cardiothoracic-drainage/thopaz
- Filosso PL, Ruffini E, Solidoro P, et al. Digital air leak monitoring after lobectomy for primary lung cancer in patients with moderate COPD: can a fast-tracking algorithm reduce postoperative costs and complications? J Cardiovasc Surg (Torino) 2010;51:429-33. [PubMed]
- McGuire AL, Petrcich W, Maziak DE, et al. Digital versus analogue pleural drainage phase 1: prospective evaluation of interobserver reliability in the assessment of pulmonary air leaks. Interact Cardiovasc Thorac Surg 2015;21:403-7. [Crossref] [PubMed]
- Varela G, Jiménez MF, Novoa NM, et al. Postoperative chest tube management: measuring air leak using an electronic device decreases variability in the clinical practice. Eur J Cardiothorac Surg 2009;35:28-31. [Crossref] [PubMed]
- Gilbert S, McGuire AL, Maghera S, et al. Randomized trial of digital versus analog pleural drainage in patients with or without a pulmonary air leak after lung resection. J Thorac Cardiovasc Surg 2015;150:1243-9. [Crossref] [PubMed]
- Lijkendijk M, Licht PB, Neckelmann K. Electronic versus traditional chest tube drainage following lobectomy: a randomized trial. Eur J Cardiothorac Surg 2015;48:893-8; discussion 898. [Crossref] [PubMed]
- Marjanski T, Sternau A, Rzyman W. The implementation of a digital chest drainage system significantly reduces complication rates after lobectomy-a randomized clinical trial. Pol J Thorac Cardiovasc Surg 2013;10:133-8.
- Mier JM, Molins L, Fibla JJ. The benefits of digital air leak assessment after pulmonary resection: prospective and comparative study. Cir Esp 2010;87:385-9. [Crossref] [PubMed]
- Miller DL, Helms GA, Mayfield WR. Digital drainage system reduces hospitalization after video-assisted thoracoscopic surgery lung resection. Ann Thorac Surg 2016;102:955-61. [Crossref] [PubMed]
- Pompili C, Brunelli A, Salati M, et al. Impact of the learning curve in the use of a novel electronic chest drainage system after pulmonary lobectomy: a case-matched analysis on the duration of chest tube usage. Interact Cardiovasc Thorac Surg 2011;13:490-3; discussion 493. [Crossref] [PubMed]
- Takamochi K, Nojiri S, Oh S, et al. Comparison of a digital with a traditional thoracic drainage system for postoperative chest tube management after pulmonary resection: a prospective randomized trial. J Thorac Cardiovasc Surg 2017. In press. [Crossref]
- Dylewski MR, Ohaeto AC, Pereira JF. Pulmonary resection using a total endoscopic robotic video-assisted approach. Semin Thorac Cardiovasc Surg 2011;23:36-42. [Crossref] [PubMed]


