Correlation of bispectral index and Richmond agitation sedation scale for evaluating sedation depth: a retrospective study
Introduction
With continuous improvement of flexible fiberoptic bronchoscopy (FFB) technique, FFB has been increasingly applied in intensive care unit (ICU) patients, which is considered to be a novel and ideal diagnostic and therapeutic method in a variety of lung diseases (1,2). FFB had become a routine and safe operation with low mortality about 0.019% (3), which was considered as the gold standard for observing airway diseases (4). However, along with increasing number of critically ill, elderly and high-risk patients undergoing FFB, safety issues have become more and more concerned. Meanwhile, the proportion of bronchoalveolar lavage and complicated treatment of FFB is getting higher and higher than simple diagnosis, which makes safety issues more prominent. Noxious stimulation from FFB, which could cause adverse influence and be life-threatening condition occasionally, made sedation to be a requisite for a satisfactory condition, except when there are contraindications. Therefore, appropriate sedation is necessary to attenuate physiologic response, prevent complications and improve security, patients’ tolerance and comfort (4-7).
Assessing and adjusting the depth of sedation play crucial roles in sedation management (8).
Richmond agitation sedation scale (RASS), as a conventional clinical subjective sedation scale based on patient response to stimulation, has been proven to be valid and reliable assessment tool in adult ICU patients for more than ten years (9,10). Given the limitations of RASS to monitor sedation level, a new method was required. bispectral index (BIS) is an objective and non-invasive indicator based on electroencephalographic (EEG) analysis (11,12) to evaluate sedation level and aid in achieving optimal titration of sedatives, which quantifies the depth of sedation by dimensionless numerical parameter between 0 (isoelectric EEG activity) and 100 (fully awake). Applying BIS to monitor the depth of anesthesia had been widely accepted and gained popularity. Several researches have reported that BIS values are significantly correlated with RASS scores for evaluating sedation in ICU patients (13-16). However, supportive evidence in application of BIS during FFB are still lacking. Thus, current study aimed to assess the correlation of BIS with RASS for evaluating sedation in ICU patients undergoing FFB and explore the possibility of replacing RASS with BIS.
Methods
Study population
Seventy-four patients were collected from the third ICU ward of the Second Affiliated Hospital of Harbin Medical University between May 2012 and June 2015. The inclusion criteria included: (I) ICU patients who receive invasive mechanical ventilation and require FFB; (II) monitoring BIS using BIS module of BeneView T8Mindray monitoring device; (III) aged >18 years; (IV) with stable hemodynamics, while the exclusion criteria included: data not competed. Patients were divided into two groups according to the sedatives used, and sedation levels were evaluated using the 10-grade RASS and were monitored continuously with a BIS monitor throughout the procedure every 5 minutes. The study was approved by the Ethics Committee of the Institutional Research Board of Harbin Medical University, and all clinical data were collected with the patients’ and the healthy control group’ s informed consent.
Medical team
An experienced bronchoscopist, assisted by a respiratory therapist (RT) and a senior nurse, performed FFB who were in charge of operation, assessing sedation level (all participants were trained on how to assess sedation level) and adjust sedatives and record data, drug administration and technical assistance, respectively. All participants were familiar with sedation protocol, operating processes and symptomatic treatment.
Sedation protocol
Drug selection
Fentanyl citrate injection [2 mL (0.1 mg)/ampoule, Renfu Pharmaceutical Co., Ltd., Yichang, China] was used as the analgesia and following drugs were used for sedation: dexmedetomidine hydrochloride injection [2 mL (200 µg)/ampoule, Hengrui Pharmaceutical Co., Ltd., Jiangsu, China]; midazolam injection [2 mL (10 mg)/ampoule, Enhua Pharmaceutical Co., Ltd., China]; and propofol injection [50 mL (1 g)/ampoule, Fresenius Kabi pharmaceutical Co., Ltd., Beijing, China].
Sedation protocol
All drugs were administered after consciousness recovery of patients or RASS score reaching zero. Endoscopic dripping of 2% lidocaine (3–5 mg/kg) was performed for topical anesthesia, and then intravenous injection of fentanyl citrate (2.0 µg/kg) was administered. The patients received a standard sedation protocol consisting of intravenous pumping a loading dose of dexmedetomidine 0.8 µg/kg or midazolam 0.05 mg/kg for 10 min followed by maintenance dose of dexmedetomidine or midazolam ranging from 0.2–0.7 µg/kg/h or 0.02–0.2 mg/kg/h, respectively to a require target score between RASS-3 (subject is moderately sedated, with some movement or eye opening. no eye contact.) and -4 (subject is deeply sedated, with no response to voice, but movement or eye opening to physical stimulation) as satisfactory deep sedation level. Bronchoscopists inserted bronchoscopy when reaching required sedation level. Propofol injection with a loading dose of 2.0 mg/kg could also be used for intravenous injection and can be switched to 0.5–4 mg/kg/h for remedial sedation if necessary. RASS scores were obtained every 5 minutes during FFB, and simultaneously BIS values were continuously assessed and documented, but not for sedation control. BIS was monitored using BIS module of BeneView T8 Mindray monitoring device (Mindray International Medical Co., Ltd., Shenzhen, China), BIS sensor and disposable electrode (Aspect Medical Systems Inc, Newton, Mass., USA). After clearing the frontal-temporal region with alcohol swab for skin preparation, a disposable BIS electrode was positioned on it and then connected to BIS sensor, module and monitoring device. The data and waveform of BIS were continuously recorded. BIS data were excluded if electromyogram (EMG) index was above 55 decibels and/or signal quality index was below 50%. After completion of FFB, further sedation and analgesia could be continued after patient’s conditions were evaluated. For patients with severe adverse reactions during FFB, procedure was discontinued and symptomatic treatment was provided. The therapeutic devices and drugs were easily available. Conditions were then evaluated to determine whether the procedure could be continued.
Vital signs monitoring and invasive mechanical ventilation
All patients received electrocardiogram, invasive artery blood pressure, respiratory rate (RR) and SpO2 monitoring (Mindray monitoring device, BeneView T8), and invasive mechanical ventilation prior to FFB. Ventilator parameters were set to keep SpO2 >90% during FFB, otherwise examinations were discontinued.
Bronchoscopy
A fiberoptic bronchoscope (Olympus LF-TP, Japan) was used in accordance with standardized procedures.
Data collection
Baseline data
Gender, age, height, weight, acute physiology and chronic health evaluation (APACHE) II score, and indications for FFB were obtained from patient medical records.
Sedative effects
RASS score, BIS value, heart rate (HR), invasive artery blood pressure, RR, and SpO2 were recorded every five minutes during FFB. Frequencies of remedial sedation by propofol, total sedation time, time of FFB, and incidence of adverse events (including cough, nausea, and bronchospasm) were collected. All measurements were terminated at the end of FFB. After completion of FFB, bronchoscopist sedation satisfaction scores were recorded for all patients (“0” indicated very unsatisfied and “10” indicated very satisfied). Complications including nausea, tachycardia, bradycardia, arrhythmia, SpO2 decrease, hypotension, hypertension and others were also recorded.
Statistical analyses
Data were analyzed using SPSS 22.0 (SPSS Inc., Chicago, USA). Quantitative and qualitative data were expressed as means ± standard deviations (SD) and numbers or percentages, respectively. Student’s t-test and Chi-squared test were used to compare quantitative and qualitative data between groups, respectively. Pearson correlation analysis was applied to correlate BIS value with RASS score, total sedation time, time of FFB and satisfaction score of the bronchoscopists, while Spearman correlation analysis was used to correlate BIS value with cough, bronchospasm and oxygen desaturation. P<0.05 was considered to be statistically significant.
Results
Patient characteristics
A total of 342 paired data of 74 patients were obtained. Patients were divided into dexmedetomidine (n=31) and midazolam (n=43) groups accordingly. The characteristics of study population are shown in Table 1.
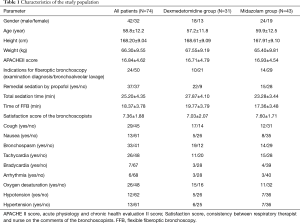
Full table
Correlation between BIS value and RASS score
A correlation existed between BIS values and RASS scores in all patients undergoing FFB in dexmedetomidine and midazolam groups at different time points (P<0.05, respectively). Correlation coefficients were higher in the midazolam group compared with dexmedetomidine group at different time points. Correlation coefficients between BIS values and RASS scores are shown in Table 2.
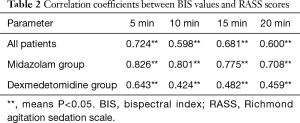
Full table
Discussion
RASS, a 10-level numerical rating scale, is one of the most commonly used conventional sedation agitation scales in clinical practice (17), deduced from the response to auditory and physical stimulation and observation of patients like other subjective tools. When application of subjective tools is impractical due to their above-mentioned disadvantages, objective indicators are essential to be an adjunctive or alternative method.
In present study, a statistically significant correlation existed between BIS values and RASS scores in all patients undergoing FFB and dexmedetomidine and midazolam groups at different time points. And it may indicate for the potential validity, reliability and practicability of BIS in the process of FFB. In addition, it may support the idea of replacing RASS with BIS due to its advantages including objectivity, continuity, non-invasion and simplicity. Correlation coefficients were higher in the midazolam group compared with dexmedetomidine group at different time points. There were no significant differences in terms of patient baseline characteristics between groups, whereas total sedation time and time of FFB were significantly shorter in the midazolam group, with a lower percentage of these patients requiring propofol for remedial sedation during FFB. In addition, the number of patients of detected data was significantly more in the dexmedetomidine group compared with the midazolam group at 20, 25 and 30 min. Furthermore, the incidence of cough, bronchospasm, and oxygen desaturation was significantly higher in the dexmedetomidine compared with midazolam group. All these mean that dexmedetomidine had a poorer sedation effect during FFB in agreement with our previous finding, which could lead to overestimated BIS values (18) and might be associated with lower correlation coefficients. Dexmedetomidine is more effective in conscious and light sedation (19), not in deep sedation. Although BIS values were merely documented, but not used for sedation control, it could still give operators hints to adjust sedation level, which might lead to no significant difference in terms of satisfaction score of the bronchoscopists between groups in contrast to our previous finding.
Also there are some limitations in the current study. First this study is a single-center retrospective study with relatively small sample size. Secondly, although no research has revealed the differences between special BIS monitor and BIS module of BeneView T8 Mindray monitoring device, lacking special BIS monitor may affect the accuracy of data. Thirdly, FFB was performed by different bronchoscopists, therefore the results could be affected by operator experience and tendentiousness, this could be improved in future study. Future studies comprising larger sample size are needed to verify our findings.
In addition, we should also pay attention to some factors, which can affect accuracy of the numerical BIS scale, including hepatic or renal failure with associated encephalopathy, inadequate sedation and analgesia, EMG interference, circulation inhibition, and blood glucose level (20-27). Under- or over-estimating BIS value can affect the correlation with clinical subjective sedation score, as shown in our study, which should be attached much weight to in clinical practices.
Conclusions
In summary, the present study showed that there was a correlation between BIS and RASS for evaluating depth of sedation in ICU patients undergoing FFB, which testified its validity, reliability and practicability in clinical setting. Our study demonstrates that BIS monitoring is a meaningful and objective tool, which can be applied as a adjunctive or alternative method to assess sedation, especially for high-risk patients who are prone to be under- or over-sedation.
Acknowledgements
We thank the participants and colleagues (X Zhang, R Huang, J Qu, S Wang, R Liu, J Liu) from the third ICU ward of the Second Affiliated Hospital of Harbin Medical University, and all the people who offer the advice and help to this study.
Funding: The present study was supported by a Heilongjiang Health Department project (2011-064).
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The study was approved by the Ethics Committee of the Institutional Research Board of Harbin Medical University (No. HMUIRB20170008), and all clinical data were collected with the patients’ and the healthy control group’ s informed consent.
References
- Fadaizadeh L, Hoseyni MS, Shajareh E, et al. Use of Bispectral Index Score for interventional bronchoscopy procedures. Tanaffos 2015;14:246-51. [PubMed]
- Sriratanaviriyakul N, Lam F, Morrissey BM, et al. Safety and clinical utility of flexible bronchoscopic cryoextraction in patients with non-neoplasm tracheobronchial obstruction: a retrospective chart review. J Bronchology Interv Pulmonol 2015;22:288-93. [Crossref] [PubMed]
- Barnett AM, Jones R, Simpson G. A survey of bronchoscopy practice in Australia and New Zealand. J Bronchology Interv Pulmonol 2016;23:22-8. [Crossref] [PubMed]
- Jose RJ, Shaefi S, Navani N. Sedation for flexible bronchoscopy: current and emerging evidence. Eur Respir Rev 2013;22:106-16. [Crossref] [PubMed]
- Kar Kurt O, Talay F, Kargi A, et al. Sedation for fiberoptic bronchoscopy: review of the literature. Tuberk Toraks 2015;63:42-7. [Crossref] [PubMed]
- Frade-Mera MJ, Regueiro-Diaz N, Diaz-Castellano L, et al. A first step towards safer sedation and analgesia: a systematic evaluation of outcomes and level of sedation and analgesia in the mechanically ventilated critically ill patient. Enferm Intensiva 2016;27:155-67. [Crossref] [PubMed]
- Pickles J, Jeffrey M, Datta A, et al. Is preparation for bronchoscopy optimal? Eur Respir J 2003;22:203-6. [Crossref] [PubMed]
- Rouche O, Wolak-Thierry A, Destoop Q, et al. Evaluation of the depth of sedation in an intensive care unit based on the photo motor reflex variations measured by video pupillometry. Ann Intensive Care 2013;3:5. [Crossref] [PubMed]
- Sessler CN, Gosnell MS, Grap MJ, et al. The Richmond Agitation-Sedation Scale: validity and reliability in adult intensive care unit patients. Am J Respir Crit Care Med 2002;166:1338-44. [Crossref] [PubMed]
- Yousefi H, Toghyani F, Yazdannik AR, et al. Effect of using Richmond Agitation Sedation Scale on duration of mechanical ventilation, type and dosage of sedation on hospitalized patients in intensive care units. Iran J Nurs Midwifery Res 2015;20:700-4. [Crossref] [PubMed]
- Avidan MS, Zhang L, Burnside BA, et al. Anesthesia awareness and the bispectral index. N Engl J Med 2008;358:1097-108. [Crossref] [PubMed]
- Myles PS, Leslie K, McNeil J, et al. Bispectral index monitoring to prevent awareness during anaesthesia: the B-Aware randomised controlled trial. Lancet 2004;363:1757-63. [Crossref] [PubMed]
- Prottengeier J, Moritz A, Heinrich S, et al. Sedation assessment in a mobile intensive care unit: a prospective pilot-study on the relation of clinical sedation scales and the bispectral index. Crit Care 2014;18:615. [Crossref] [PubMed]
- Jung YJ, Chung WY, Lee M, et al. The significance of sedation control in patients receiving mechanical ventilation. Tuberc Respir Dis (Seoul) 2012;73:151-61. [Crossref] [PubMed]
- Yaman F, Ozcan N, Ozcan A, et al. Assesment of correlation between bispectral index and four common sedation scales used in mechanically ventilated patients in ICU. Eur Rev Med Pharmacol Sci 2012;16:660-6. [PubMed]
- Karamchandani K, Rewari V, Trikha A, et al. Bispectral index correlates well with Richmond agitation sedation scale in mechanically ventilated critically ill patients. J Anesth 2010;24:394-8. [Crossref] [PubMed]
- Ely EW, Truman B, Shintani A, et al. Monitoring sedation status over time in ICU patients: reliability and validity of the Richmond Agitation-Sedation Scale (RASS). JAMA 2003;289:2983-91. [Crossref] [PubMed]
- Fraser GL, Riker RR. Bispectral index monitoring in the intensive care unit provides more signal than noise. Pharmacotherapy 2005;25:19s-27s. [Crossref] [PubMed]
- Mondal S, Ghosh S, Bhattacharya S, et al. Comparison between dexmedetomidine and fentanyl on intubation conditions during awake fiberoptic bronchoscopy: A randomized double-blind prospective study. J Anaesthesiol Clin Pharmacol 2015;31:212-6. [Crossref] [PubMed]
- Riker RR, Fraser GL, Simmons LE, et al. Validating the sedation-agitation scale with the Bispectral Index and Visual Analog Scale in adult ICU patients after cardiac surgery. Intensive Care Med 2001;27:853-8. [Crossref] [PubMed]
- Nasraway SS Jr, Wu EC, Kelleher RM, et al. How reliable is the Bispectral Index in critically ill patients? A prospective, comparative, single-blinded observer study. Crit Care Med 2002;30:1483-7. [Crossref] [PubMed]
- Vivien B, Di Maria S, Ouattara A, et al. Overestimation of Bispectral Index in sedated intensive care unit patients revealed by administration of muscle relaxant. Anesthesiology 2003;99:9-17. [Crossref] [PubMed]
- Brenner RP. The interpretation of the EEG in stupor and coma. Neurologist 2005;11:271-84. [Crossref] [PubMed]
- Mondello E, Siliotti R, Noto G, et al. Bispectral Index in ICU: correlation with Ramsay Score on assessment of sedation level. J Clin Monit Comput 2002;17:271-7. [Crossref] [PubMed]
- Liu N, Pruszkowski O, Leroy JE, et al. Automatic administration of propofol and remifentanil guided by the bispectral index during rigid bronchoscopic procedures: a randomized trial. Can J Anaesth 2013;60:881-7. [Crossref] [PubMed]
- Wu CC, Lin CS, Mok MS. Bispectral index monitoring during hypoglycemic coma. J Clin Anesth 2002;14:305-6. [Crossref] [PubMed]
- Azim N, Wang CY. The use of bispectral index during a cardiopulmonary arrest: a potential predictor of cerebral perfusion. Anaesthesia 2004;59:610-2. [Crossref] [PubMed]


