An adult case of plastic bronchitis: a rare and multifactorial disease
Introduction
Plastic bronchitis is a rare but serious disease. Mainly a disease of the pediatric age, its occurrence in adulthood should not be overlooked in particular in patients with chronic inflammatory disease and those undergone heart surgery. Diagnosis is clinical. Histology (Seear classification) serves as confirmation, and can offer valuables information regarding etiology and treatment.
Case presentation
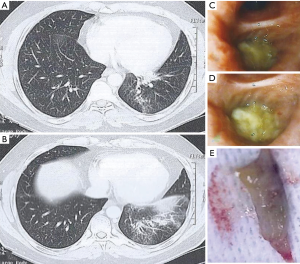
A 41-year-old non-smoker patient, born from consanguineous parents, was referred to the pneumology department for several episodes of acute dyspnea, productive cough with expectoration of mucous plugs, fever and chest pain for the past 2 years; these episodes were punctually treated with antibiotics and corticosteroids. Patient’s anamnesis was positive for allergic asthma, without criteria of allergic bronchopulmonary aspergillosis. Physical examination revealed wheezing and decreased breath sounds at the left posterior base of the lung. Chest high-resolution computed tomography (HRCT) demonstrated left lower lobe bronchial obstruction and partial atelectasis of the left lower lobe with ventilation defects (Figure 1A,B). Flexible bronchoscopy showed bronchial obstruction (Figure 1C,D) from a dense plug that was removed en bloc (Figure 1E).
Histology revealed a cast of necrotic cells with florid eosinophilic infiltration (Figure 2). Gram, Periodic Acid Schiff (PAS) and Grocott’s stains were negative, and cultures of bronchoalveolar lavage sterile. The patient underwent three more flexible bronchoscopies for removal of recurrent left lower lobe plugs. Finally, persistence of left lower lobe atelectasis on HRCT, as well as patient’s clinical deterioration prompted left lower lobectomy. Histologic examination revealed squamous (Malpighian) metaplasia of the bronchial mucous membrane with intense inflammation. Despite postoperative respiratory kinesiotherapy, the patient presented another episode of acute dyspnea and underwent flexible bronchoscopy with removal of plug from the right lower lobe bronchus. The patient was referred to our department for a second medical opinion. Etiologic work-up showed normal hemoglobin electrophoresis as well as the absence of cardiac or lymphatic disorders. Moreover, no cystic fibrosis transmembrane conductance regulator (CFTR) gene mutations were identified, thus excluding cystic fibrosis as a possible cause.

Patient’s clinical history and histology led us to the diagnosis of plastic bronchitis with type 1 casts in the context of chronic allergic airway inflammation. Treatment with oral corticosteroid was started, with no recurrence of respiratory symptoms so far.
Comments
Plastic bronchitis is a rare but serious disease (mortality range from 6% to 60% depending on the underlying cause) often leading to multiple hospitalizations and invasive procedures; moreover, extensive casts can obstruct the main airways eventually provoking fatal asphyxia (1). Diagnosis is essentially clinical, while histology (cast analysis) serves as confirmation. Patients with plastic bronchitis most commonly present cough with solid expectoration, wheezing, chest pain and fever. Decreased breath sound and dullness to percussion are typical on physical examination, while partial lung atelectasis is a usual finding on chest X-ray and CT. Plastic bronchitis can be classified according to cast composition and etiology. The widely accepted classification of Seear divides casts into two types. Type 1 casts are rich in inflammatory cells (mainly eosinophils), fibrin and Charcot-Leyden crystals, and are commonly associated to inflammatory conditions (asthma, cystic fibrosis, acute chest syndrome in sickle cell disease). Type 2 casts are devoid of inflammation, scarcely cellular and mainly mucinous; they are associated with congenital heart diseases, lymphatic abnormalities (i.e., lymphatic plastic bronchitis) and, albeit rarely, heart surgery (2,3). Abnormal pulmonary lymphatic vessels and drainage are often the underlying cause. Interestingly, although plastic bronchitis is typically associated with Fontan procedure for children with univentricular hearts (4), three cases of plastic bronchitis after cardiopulmonary bypass have been described (5-7). Management is still debated. Symptomatic treatment consists in bronchoscopic mucus plug removal; in this regard, cryoextraction (cryotherapy) seems a promising technique for en bloc removal of the frozen bronchial casts (8). Etiological treatment depends on cast type. For type 1 casts inhaled or systemic corticosteroids and N-acetylcysteine can be useful; the use of antibiotics, recombinant human deoxyribonuclease, unfractionated heparin, urokinase or tissue plasminogen activator has also been described (9). For type 2 casts, treatment of the underlying condition is needed to prevent recurrence. However, type 2 casts associated with congenital heart disease are often treated akin to type 1 casts, i.e., with mucolytic and fibrinolytic agents; yet, mechanical disruption is a mainstay (10).
In case of lymphatic abnormalities (e.g., leaking), MRI (dynamic contrast-enhanced magnetic resonance lymphangiogram)-guided selective lymphatic embolization is a safe and effective interventional strategy. In difficult cases, occlusion of the thoracic duct can be considered (10).
Effective for vascular anomalies, the mTOR inhibitor Sirolimus (rapamycin) seems a promising therapeutic agent for lymphatic plastic bronchitis given its capacity in reducing lymphatic leakage (11,12).
Plastic bronchitis is mainly a disease of the pediatric age, with few adult cases described. Nevertheless, we believe that its occurrence in adulthood should not be overlooked. Clinicians, and in particular pneumologists, cardiologists, heart and thoracic surgeons, must be aware of this condition when dealing with patients with history of heart surgery or in those with chronic inflammatory lung disease.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: We have obtained the informed written consent (in French) form the patient.
References
- Madsen P, Shah SA, Rubin BK. Plastic bronchitis: new insights and a classification scheme. Paediatr Respir Rev 2005;6:292-300. [Crossref] [PubMed]
- Seear M, Hui H, Magee F, et al. Bronchial casts in children: a proposed classification based on nine cases and a review of the literature. Am J Respir Crit Care Med 1997;155:364-70. [Crossref] [PubMed]
- Rubin BK. Plastic Bronchitis. Clin Chest Med 2016;37:405-8. [Crossref] [PubMed]
- Tzifa A, Robards M, Simpson JM. Plastic bronchitis; a serious complication of the Fontan operation. Int J Cardiol 2005;101:513-4. [Crossref] [PubMed]
- Schmitz LM, Rihawi M. Plastic bronchitis: a complication of myocardial revascularization. Am J Respir Crit Care Med 2012;185:896-7. [Crossref] [PubMed]
- Eberlein M, Parekh K, Hansdottir S, et al. Plastic bronchitis complicating primary graft dysfunction after lung transplantation. Ann Thorac Surg 2014;98:1849. [Crossref] [PubMed]
- Sheikh AY, Ahmadi-Kashani M, Mohindra V, et al. A Rare Case of Plastic Bronchitis in an Adult Patient After Cardiopulmonary Bypass. Ann Thorac Surg 2016;101:1176-8. [Crossref] [PubMed]
- Sriratanaviriyakul N, Lam F, Morrissey BM, et al. Safety and Clinical Utility of Flexible Bronchoscopic Cryoextraction in Patients With Non-neoplasm Tracheobronchial Obstruction: A Retrospective Chart Review. J Bronchology Interv Pulmonol 2015;22:288-93. [Crossref] [PubMed]
- Do P, Randhawa I, Chin T, et al. Successful management of plastic bronchitis in a child post Fontan: case report and literature review. Lung 2012;190:463-8. [Crossref] [PubMed]
- Kunder R, Kunder C, Sun HY, et al. Pediatric plastic bronchitis: case report and retrospective comparative analysis of epidemiology and pathology. Case Rep Pulmonol 2013;2013:649365. [Crossref] [PubMed]
- Itkin M. Interventional Treatment of Pulmonary Lymphatic Anomalies. Tech Vasc Interv Radiol 2016;19:299-304. [Crossref] [PubMed]
- Nadal M, Giraudeau B, Tavernier E, et al. Efficacy and safety of mammalian target of rapamycin inhibitors in vascular anomalies: a systematic review. Acta Derm Venereol 2016;96:448-52. [Crossref] [PubMed]


