Clinical applications of virtual navigation bronchial intervention
Introduction
The usefulness of a high-speed 3-dimensional (3D) image analysis system, Synapse Vincent (Fuji Photo Film Co., Ltd., Tokyo, Japan) has been reported previously to determine the preoperative simulation of lung segmentectomy and video-assisted thoracic surgery (VATS) (1-4), as well as the best positioning of robot assisted thoracic surgery (5). An overview of these studies shows the effectiveness of preoperative simulation and intraoperative navigation using the Synapse Vincent. This system detects not only the tumor but also the thorax, mediastinum, lung, veins and airway which enables rapid enhanced computed tomography (CT) accurately, and safely.
In patients with endobronchial tumors, endoscopic treatment is frequently regarded as the first treatment of choice, but the indications and decisions regarding the method require careful consideration (6-9). In previous study we reported (10) a variety of interventional therapies for patients compromised by advanced age or poor general status. It is important to strictly adhere to the indications of each technique including high-power laser irradiation with a neodymium-yttrium-aluminum-garnet laser (Nd-YAG) laser, microwave (MW), argon plasma coagulation (APC) and high radiofrequency (HRF) snares. Rarely, bronchoscopic interventions may have fatal complications (11).
To select safer and more precise approach for patients with bronchial tumors, we evaluated virtual navigation bronchial intervention using a high-speed 3D image analysis system in two cases employing Synapse Vincent. We report the indications and efficacy of virtual navigation intervention for the treatment of these two tumors.
Methods
We retrospectively examined the efficacy of virtual navigation bronchial intervention using a high-speed 3D image analysis system, Synapse Vincent, for two patients with bronchial tumors.
All patients provided written informed consent to the procedures, all of which were performed as part of the regular preoperative workup. All patients were anonymised and our Institutional Review Board approved all data collection and analyses (2016-075). We set out to clarify, based on retrospective evaluation of routine work-up data in our charts and patient treatment data, the efficacy and most appropriate indications for various specifically selected conditions. These were representative of the spectrum of conditions we encountered, with bronchial tumors in order to provide a guide to techniques available for interventional bronchology in various obstructive lesions.
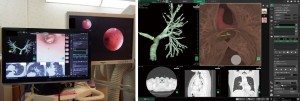
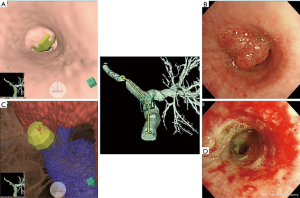
All CT findings had to satisfy several conditions necessary to analyze images by Synapse Vincent. First, all images were to be taken by multi-slice CT at more than 64 lines; secondly, all images were taken at slice interval thicknesses of 1.25 mm; third, all image data were saved as digital imaging and communication in medicine (DICOM) image files; and fourth, all images were taken using contrast media. Synapse Vincent also provided more detailed information not only concerning anatomical structure and tumor size, shape and vessel involvement. It also indicated whether the tumor invaded surrounding tissue including vessels and airways with translucent 3D images (Figure 1) (3). For cases 1 and 2, we employed local anesthesia of approximately 10 mL of 2% xylocaine given by a Jackson spray in synchrony with the patient’s inhalation, before inserting the flexible bronchoscope and giving additional xylocaine via the working channel as needed. Both the rigid and flexible instruments can be used in combination with a variety of ancillary therapeutic methods as we reported previously (10).
Results
In the representative cases in which we applied virtual navigation bronchial intervention, tumors were located in the left main bronchus, in cases 1 and 2. We selected the most suitable and safe techniques using virtual navigation bronchial intervention to achieve complete tumor resection according to the location and tumor characteristics. Both patients were weaned from artificial respiration.
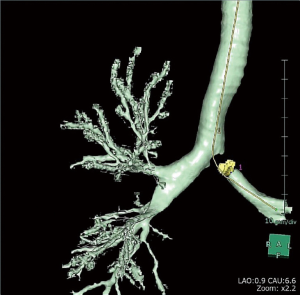
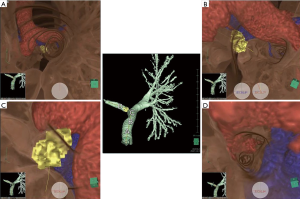
Case 1 was a 65-year-old woman with history of adenocarcinoma of the right lower lung lobe (clinical stage IV; T2a N3M1b) treated with chemotherapy since 2010. Chest multiple detector CT, virtual bronchoscope simulated images analyzed with Synapse Vincent and real bronchofiberscope (BF) images revealed almost complete obstruction of the left main bronchus by tumor recurrence (Figures 2-4). The BF findings revealed a smooth lesion occupying more than 90% of the left main bronchial lumen. The left main bronchial tumor appeared to be a pedunculated polypoid lesion with a smooth, red mucosal surface. The pedunculated tumor in the left main bronchus on the left side of the carina moved on respiration. Bronchial simulation by Synapse Vincent confirmed that no blood vessels were present outside the bronchial wall, indicating the safety (Figures 3C,4C), and then we resected the distal root of the tumor with electrocautery snaring and removed the tumor surgically. The surgical margin was not cauterized by MW coagulation.
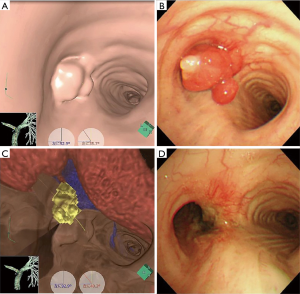
Case 2 was 64-year-old man with a history of squamous cell carcinoma of the middle mediastinum treated with surgery and adjuvant chemoradiotherapy in 2008.Metastasis of the right upper lung was revealed in 2010, and right upper lobectomy was performed after induction chemotherapy. In 2012, metastasis was recognized in the trachea and left main bronchus again, and the same physician treated the patient by bronchial intervention. Finally, enlargement of the tumor in the left main bronchus, accompanied by severe dyspnea required transfer to our hospital for bronchial intervention including airway stenting. Chest multiple detector CT, virtual bronchoscopic simulated images analyzed with Synapse Vincent and real BF images revealed almost complete obstruction of the left main bronchus caused by tumor recurrence (Figures 5,6). Chest CT and BF findings showed a tumor with an irregular smooth surface protruding from the left main bronchus. The half-skeleton mode in the bronchial simulator of Synapse Vincent identified a blood vessel connected to the tumor from beyond the bronchus wall (Figure 6C). Therefore, tumorectomy was performed with an HRF snare via BF under local anesthesia safely, and the base of the lesion was carefully coagulated with APC.

Discussion
Mochizuki et al. reported the feasibility and safety of Synapse Vincent in performing preoperative simulation and navigation of surgical procedures (12). The recent development of Synapse Vincent raises the question of whether it can yield comparable results in terms of speed and precision. Our previous study demonstrated that preoperative simulation using Synapse Vincent for the assessment of pulmonary vessel branching patterns appear to be beneficial for the safe and efficient performance of VATS anatomical resection and for further understanding of the surgical anatomy related to general thoracic surgery (1-4). It is safer, more precise, and less invasive for the patient. It is also easy to construct an image, depending on the purpose, within 5–10 minutes using the Synapse Vincent. The Synapse Vincent can separate blood vessels and bronchi based on color and can grasp an anatomical structure based on the semi-transparent image. It is possible to comprehend the 3D position of the structure based on this function. Our previous report (3) showed a total of 97.8% of pulmonary artery branches were precisely identified and all anomalous or irregular pulmonary vessel branching patterns were accurately confirmed by 3D imaging. Another useful function is the free rotary image, the route selection being possible from any point in addition to the recommended route, and moreover any other approach is possible from any random bronchus. Moreover, Synapse Vincent is able to simultaneously determine the target of many points, and this function is effective for endobronchial ultrasound-guided transbronchial needle aspiration (EBUS-TBNA). The 3D CT and simulated images created with Synapse Vincent which can display minute details can confirm the tumor position, size, and surface appearance. Pretherapeutically, it is particularly necessary to accurately grasp the extramural vascular anatomy. While endoscopic treatment is frequently the best choice, careful consideration concerning the choice and application of therapeutic implements is essential before treatment or in cases in which fatal hemorrhage might be caused by bronchial wall perforation. We set out to identify the effectiveness of simulation with Synapse Vincent which shows real images for pre-interventional assessment and navigation during manipulation of fiberoptic bronchoscopy. An additional option of Synapse Vincent can visualize the semi-skeleton structure under the bronchi. This function is extremely useful in grasping the extra-bronchial (sub-mucosal) anatomical structure. Virtual bronchial navigation (VBN) has many merits, including simple rapid and precise lesion-identification, endoscopic rotation and screen automatic rotary function. This helps synchronize the display function evaluating the distance to a lesion, as well as safety intervention and semi-transparency display by visualization of the external bronchial wall. Moreover, if the lesion is in the parenchyma, it helps to perform simulation with virtual skeletal subtraction, estimating potential lesion movement. Since the angle of the 3D-image created by the Synapse Vincent can be altered freely on a personal computer, an angle image similar to the operation field in the surgical procedure can be obtained in the format of a simulation image. Constructed images are displayed on a monitor, which can be utilized for deciding interventional strategy and for navigation during bronchoscopical manipulation.
Finally, the semi-transparent display of the external bronchial wall can assist preventive measures to perform interventional safety and this system also allows precise pre-interventional simulation and educational use.
Conclusions
Pre-interventional simulation and navigation during bronchoscopical manipulation using the Synapse Vincent system reduces the risk for patient’s and the stress level of operators. This is particularly so when the tumor is located in a highly risk area, such as very close to pulmonary vessels which cannot be seen by the fiberoptic bronchoscope. The patients recovered and were weaned from artificial respiration. This information, including both pre-interventional simulation and intra-interventional navigation, provides greater safety and precision in the airway intervention. These instruments promote safer and more effective educational use.
Acknowledgements
The authors are grateful to Emeritus Professor J. Patrick Barron of the Department of International Medical Communications, Tokyo Medical University, and Adjunct Professor of Seoul National University Bundang Hospital, for reviewing this manuscript pro bono.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: Our Institutional Review Board approved all data collection and analyses (2016-075) and all patients provided written informed consent to the procedures.
References
- Ikeda N, Yoshimura A, Hagiwara M, et al. Three dimensional computed tomography lung modeling is useful in simulation and navigation of lung cancer surgery. Ann Thorac Cardiovasc Surg 2013;19:1-5. [Crossref] [PubMed]
- Saji H, Inoue T, Kato Y, et al. Virtual segmentectomy based on high-quality three-dimensional lung modelling from computed tomography images. Interact CardioVasc Thorac Surg 2013;17:227-32. [Crossref] [PubMed]
- Hagiwara M, Shimada Y, Kato Y, et al. High-quality 3-dimensional image simulation for pulmonary lobectomy and segmentectomy: results of preoperative assessment of pulmonary vessels and short-term surgical outcomes in consecutive patients undergoing video-assisted thoracic surgery. Eur J Cardiothorac Surg 2014;46:e120-6. [Crossref] [PubMed]
- Fukuta K, Shimada Y, Hagiwara M, et al. High-quality 3-dimensional imaging for patients with anomalous pulmonary veins. Asian Cardiovasc Thorac Ann 2015;23:585-7. [Crossref] [PubMed]
- Kajiwara N, Akata S, Hagiwara M, et al. High-speed 3-dimensional imaging in robot-assisted thoracic surgical procedures. Ann Thorac Surg 2014;97:2182-4. [Crossref] [PubMed]
- Hespanhol V, Magalhães A, Marques A. Neoplastic severe central airways obstruction, interventional bronchoscopy: a decision-making analysis. J Thorac Cardiovasc Surg 2013;145:926-32. [Crossref] [PubMed]
- Colt HG, Harrell JH. Therapeutic rigid bronchoscopy allows level of care changes in patients with acute respiratory failure from central airways obstruction. Chest 1997;112:202-6. [Crossref] [PubMed]
- Beamis JF Jr. Interventional pulmonology techniques for treating malignant large airway obstruction: an update. Curr Opin Pulm Med 2005;11:292-5. [Crossref] [PubMed]
- Wahidi MM, Herth FJ, Ernst A. State of the art: interventional pulmonology. Chest 2007;131:261-74. [Crossref] [PubMed]
- Kajiwara N, Kakihana M, Usuda J, et al. Interventional management for benign airway tumors in relation to location, size, character and morphology. J Thorac Dis 2011;3:221-30. [PubMed]
- Zhou GW, Zhang W, Dong YC, et al. Flexible bronchoscopy-induced massive bleeding: A 12-year multicentre retrospective cohort study. Respirology 2016;21:927-31. [Crossref] [PubMed]
- Mochizuki K, Takatsuki M, Soyama A, et al. The usefulness of a high-speed 3D-image analysis system in pediatric living donor liver transplantation. Ann Transplant 2012;17:31-4. [Crossref] [PubMed]