Manual aspiration in the biopsy-side down position to deal with delayed pneumothorax after lung biopsy
Introduction
Percutaneous computed tomography (CT)-guided transthoracic needle biopsies (TTNBs) is a reliable technique for the pathologic diagnosis of pulmonary lesions. Pneumothorax is the most common complication of TTNBs (1-3). Chest pain, shortness of breath, low oxygen saturation caused by pneumothorax may increase the need for hospitalization and consequently result in increased costs. Therefore, the treatment of pneumothorax is a matter of particular interest. A variety of approaches to the technique have been evaluated in an attempt to reduce the rate of TTNBs-related pneumothorax (4,5). Simple aspiration and tube thoracostomy were recommended to deal with the pneumothorax. As reported, tube thoracostomy is associated with more complications and resulted in a longer stay in hospital than simple aspiration (6). Many previous reports have shown that increasing delayed pneumothoraces often need chest tube placement. Patient positioning after biopsy has been studied but remains controversial, some study found that placing the patients biopsy-side down (from prone to supine or vice versa) after biopsy substantially reduced the rate of pneumothorax (5,7), while some other articles found no effect (8,9). Anecdotally, we noted in practice some satisfactory results were achieved by using aspiration in biopsy-side down position. We reported our preliminary experience using a modified manual aspiration in the biopsy-side down position in an attempt to deal with delayed pneumothorax caused by biopsy, thus reduce the application of tube thoracostomy significantly.
Methods
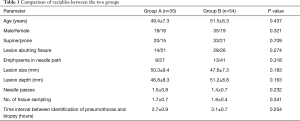
This retrospective study was approved by the Ethical Committee and Institutional Review Board of Affiliated Hospital of North Sichuan Medical College (No. NSMC1601-018). A retrospective review was performed of the clinical records and radiological findings of 1750 consecutive patients who underwent CT-guided TTNB for lung lesions from January 2011 to December 2015. A delayed pneumothorax was detected in 236 cases. Eighty-nine pneumothorax patients who underwent manual aspiration treatment, were included in our study. The average age was 50.5 years (range, 28–87 years). Patients were included into two groups according to the aspirate position. In the first half of the observation period, aspiration was done on the same side as the biopsy (group A), in a while we noticed that some aspiration results on the opposite side were encouraging and in the second half the opposite side aspiration was chosen for group B. The baseline patient clinical characteristics for two groups are shown in Table 1. Those who did not undergo an attempt at aspiration were not included into our study.
Full table
Procedures were performed by four radiologists experienced in CT-guided biopsies. All patients had prebiopsy scans of the chest available for biopsy planning using single slice helical CT scanner (X-vision, Toshiba, Tochigi, Japan). Patients were placed in prone or supine position according to their lesions. After the skin had been prepared and a local anaesthetic had been administered, TTNBs were performed using 19-gauge coaxial needle. Subsequently, the obtained material was prepared in smears and immersed in 10% formalin for pathologic examination. Follow up CT was performed using a chest CT with thin slices (3–5 mm) to detect the presence of possible complications.
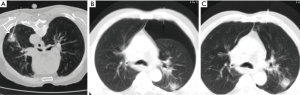
Delayed pneumothorax was defined as pneumothorax developed after the biopsy needle is removed. A pneumothorax was considered as minor pneumothorax if the distance (D) between parietal and visceral pleura was less than or equal to 1 cm, moderate if it was greater than 1 cm but less than or equal to 2 cm, or large if it was greater than 2 cm (10,11). For group A, aspiration treatment was conducted in the position same to biopsy. For group B, patients were turned to biopsy-side down position (from supine to prone or vice versa), and the aspiration performed. After needle insertion, accurate localization of the needle tip was confirmed with sequential CT images and aspiration was conducted. Oxygen was administered during and after the procedures. Patients with failed aspiration underwent insertion of a 7-F pigtail drainage catheter (BT-PD1-0730-W, Taipei, Taiwan) attached to an underwater seal placed by the radiologist.
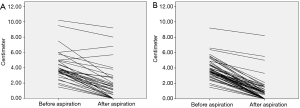
Patients were followed up with CT to check for pneumothorax and also for other complications. The maximum distance between parietal and visceral pleura was measured and compared to the distance before aspiration. The procedure was found to be effective when the distance reduced by more than or equal to half the distance before treatment and the aspiration was considered to be failed if the pneumothorax recurred to more than one-half the distance before treatment.
Statistical analysis was performed using statistical software (SPSS Inc., Chicago, IL) on a personal computer. Student’s t-test and chi-square test were used to assess the statistical significance of the differences between the two groups for continuous variables and categorized, respectively. P values less than 0.05 were considered to indicate a statistically significant difference.
Results
During the course of observation, 147 asymptomatic minimal pneumothorax patients (62.3%) of the 236 patients resolved without treatment. The remaining 89 patients were treated with an attempt manual aspiration, which included into two groups: in group A (35 patients), aspiration was performed in the same position as the biopsy, while in group B (54 patients), patients were turned to the biopsy-side down position. Distance between parietal and visceral pleura before and after aspiration were 4.24±1.87 and 1.93±2.33 cm for group A, 3.92±1.31 and 0.98±1.50 cm for group B, respectively. Volume of aspirated air in group A and group B were 735.4±231.8 and 434.8±320.3 mL, respectively. Complete lung expansion was detected in 28.6% (10/35) and 38.9% (21/54) for group A and group B. The overall effective rate and failure rate were 74.3% (26/35) and 25.7% (9/35) for group A, 92.6% (50/54) and 7.4% (4/54) for group B, respectively, with significant statistic difference (P<0.05).
Of the 54 delayed pneumothorax cases in group B, patients were turned to biopsy-side down position, and then manual aspiration conducted (Figure 1). Results of aspiration between two groups are list in Table 2. The comparison of treatment effect for two groups is provided in Figure 2.
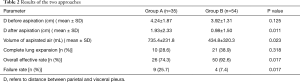
Full table
Tube thoracostomy were applied in the 25.7% (9/35) and 7.4% (4/54) patients for group A and B, respectively. For group A, aspiration were ineffective in seven patients with large tension pneumothorax and subcutaneous emphysema, other two patients suffered from severe dyspnea and hypoxemia. For group B, aspirations were unsuccessful in two patients with large tension pneumothorax, and in another two patients, pneumothorax decreased when aspiration applied, but recurrent in a short-term followed up by CT scan. We observed no serious side effects such as lung edema or hemorrhage after simple aspiration.
Discussion
It is essential to perform the TTNBs correctly in order to obtain a representative cytological sample from lung masses. Pneumothorax remains the most common and potentially serious adverse event of CT-guided lung biopsy, ranged from 8.2% to 54% (12,13). The pneumothorax rate caused by TTNBs may be affected by many factors, including the size and depth of the mass, age, emphysema in biopsy needle path, status of pulmonary function, the number of biopsies and biopsy technique (2,14,15). Pneumothorax severe enough to require tube thoracostomy is generally agreed upon to be a serious complication of TTNBs. The literature reveals the rate of tube thoracostomy varies from 7.3% to 15% (16,17). Treatment of post-biopsy pneumothorax remains a relevant clinical issue.
Thirty-five delayed patients in group A were treated with attempt simple manual aspiration in our study, which was succeed in 74.3% (26/35), similar to other reports range from 57% to 75%. While the other delayed 54 patients in group B, with puncture site in biopsy-side down position, succeed in 92.6% (50/54), significantly higher compared to other studies. Chest tube thoracostomy was applied only in 7.4% (4/54) of all delayed pneumothorax patients, which significantly lower than many other international reports.
The mainly three mechanisms which allow air to enter the pleural space are communication with the outside atmosphere, visceral pleural rupture and the presence of gas-producing organisms (18-21). And the first two factors may contribute to lung biopsy-induced pneumothorax. An unskilled biopsy may cause direct or indirect communication between the atmosphere and the pleural space, visceral pleural rupture is considered to be the most important contributing factor in lung biopsy-induced pneumothorax especially for pneumothorax in moderate to large in volume (21). The manual aspiration of a pneumothorax was initially reported by Yamagami et al. (22) as a method of preventing an increased pneumothorax that would require chest tube placement. But simple aspiration may be insufficient when the parenchymal tear is large enough and theoretically carries a high risk of short-term recurrence because (I) the aspiration in the region surrounding the leak may increase the alveolar-to-pleural pressure gradient, and (II) it does not promote pleural symphysis (23). Average volume of aspirated air in group A was significant higher than that of group B in our study. We believe that the above two contributing factors are important reasons. Furthermore, the failure rate of group A is higher than that of group B, so the therapeutic effect of aspiration in some patients were relatively poor, which leads to more gas extracted. In general, small and asymptomatic pneumothoraces often do not need any treatment, and resolve spontaneously. If the pneumothorax is moderate, or the patient is symptomatic, simple aspiration or tube thoracostomy is required (24). The attractiveness of simple aspiration is its potential for an outpatient treatment, its relative simplicity, and minimal invasiveness compared to tube thoracostomy.
Zidulka et al. (23) reported that placing dogs in the lateral decubitus position with the puncture site down stopped the progression of pneumothorax. The animal experiments hypothesized that placing the puncture site down may inhibit progression of pneumothorax by causing (I) a reduction in the size of alveoli as well as the alveolar-to-pleural pressure gradient surrounding the needle track, (II) the development of airway closure and an increased resistance to collateral ventilation, and (III) dependent accumulation of hemorrhagic fluid around the needle track. The current study demonstrates that manual aspiration in the biopsy-side down position has an encouraging result for biopsy-induced delayed pneumothorax. There were several contributing factors that might led to the high success rate in the present study. Firstly, parietal pleural rupture while not visceral pleural rupture occurred in the aspiration. This procedure does not cause increased pneumothorax further. Secondly, changing patients to biopsy-side down position may be beneficial for the visceral and parietal pleura symphysis, creating a physical barrier to further leakage of air. Finally, a different puncture site in the biopsy-side down position was selected for aspiration. This procedure did not increase the alveolar-to-pleural pressure gradient in the region surrounding the leak.
There were several limitations to our study. First, owing to the retrospective nature of our study, there may be associated with bias. For example, our study did not take into account some factors probably effect the incidence of pneumothorax such as operator experience, the presence of pulmonary hemorrhage, etc. It is also inevitable that there will be selection bias. Another limitation involved the relatively small sample sizes of patients, and further larger patient population studies are required to confirm our results.
In conclusion, the current study’s results demonstrate the safety and efficacy of aspiration in the biopsy-side down position in the treatment of delayed pneumothorax following CT-guided TTNBs. The advantage of this approach is its availability, low procedure-related morbidity, reduced pain, and lower hospitalisation rate, and significantly reduced the rate of pneumothorax requiring drainage catheter placement after CT-guided TTNBs. Therefore, the current authors recommend this procedure as an alternative treatment option to tube thoracostomy in the treatment of delayed pneumothorax after CT-guided TTNBs.
Acknowledgments
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: This retrospective study was approved by the Ethical Committee and Institutional Review Board of Affiliated Hospital of North Sichuan Medical College (No. NSMC1601-018).
References
- Boskovic T, Stanic J, Pena-Karan S, et al. Pneumothorax after transthoracic needle biopsy of lung lesions under CT guidance. J Thorac Dis 2014;6 Suppl 1:S99-107. [PubMed]
- Nakatani M, Tanigawa N, Kariya S, et al. Analysis of factors influencing accuracy and complications in CT-guided lung biopsy. Minim Invasive Ther Allied Technol 2012;21:415-22. [Crossref] [PubMed]
- Lima CD, Nunes RA, Saito EH, et al. Results and complications of CT-guided transthoracic fine-needle aspiration biopsy of pulmonary lesions. J Bras Pneumol 2011;37:209-16. [Crossref] [PubMed]
- Li Y, Du Y, Luo TY, et al. Usefulness of normal saline for sealing the needle track after CT-guided lung biopsy. Clin Radiol 2015;70:1192-7. [Crossref] [PubMed]
- Kim JI, Park CM, Lee SM, et al. Rapid needle-out patient-rollover approach after cone beam CT-guided lung biopsy: effect on pneumothorax rate in 1,191 consecutive patients. Eur Radiol 2015;25:1845-53. [Crossref] [PubMed]
- Ayed AK, Chandrasekaran C, Sukumar M. Aspiration versus tube drainage in primary spontaneous pneumothorax: a randomised study. Eur Respir J 2006;27:477-82. [Crossref] [PubMed]
- Yaffe D, Shitrit D, Gottfried M, et al. Ipsilateral opposite-side aspiration in resistant pneumothorax after CT image guided lung biopsy: complementary role after simple needle aspiration. Chest 2013;144:947-51. [Crossref] [PubMed]
- Collings CL, Westcott JL, Banson NL, et al. Pneumothorax and dependent versus nondependent patient position after needle biopsy of the lung. Radiology 1999;210:59-64. [Crossref] [PubMed]
- Masterson AV, Haslam P, Logan PM, et al. Patient positioning after lung biopsy: influence on the incidence of pneumothorax. Can Assoc Radiol J 2003;54:31-4. [PubMed]
- Billich C, Muche R, Brenner G, et al. CT-guided lung biopsy: incidence of pneumothorax after instillation of NaCl into the biopsy track. Eur Radiol 2008;18:1146-52. [Crossref] [PubMed]
- Yaffe D, Shitrit D, Gottfried M, et al. Ipsilateral opposite-side aspiration in resistant pneumothorax after CT image guided lung biopsy: complementary role after simple needle aspiration. Chest 2013;144:947-51. [Crossref] [PubMed]
- Klein JS, Salomon G, Stewart EA. Transthoracic needle biopsy with a coaxially placed 20-gauge automated cutting needle: results in 122 patients. Radiology 1996;198:715-20. [Crossref] [PubMed]
- Min L, Xu X, Song Y, et al. Breath-hold after forced expiration before removal of the biopsy needle decreased the rate of pneumothorax in CT-guided transthoracic lung biopsy. Eur J Radiol 2013;82:187-90. [Crossref] [PubMed]
- Chakrabarti B, Earis JE, Pandey R, et al. Risk assessment of pneumothorax and pulmonary haemorrhage complicating percutaneous co-axial cutting needle lung biopsy. Respir Med 2009;103:449-55. [Crossref] [PubMed]
- Boskovic T, Stojanovic M, Stanic J, et al. Pneumothorax after transbronchial needle biopsy. J Thorac Dis 2014;6:S427-34. [PubMed]
- Kuban JD, Tam AL, Huang SY, et al. The Effect of Needle Gauge on the Risk of Pneumothorax and Chest Tube Placement After Percutaneous Computed Tomographic (CT)-Guided Lung Biopsy. Cardiovasc Intervent Radiol 2015;38:1595-602. [Crossref] [PubMed]
- Asai N, Kawamura Y, Yamazaki I, et al. Is emphysema a risk factor for pneumothorax in CT-guided lung biopsy? Springerplus 2013;2:196. [Crossref] [PubMed]
- Noppen M, De Keukeleire T. Pneumothorax. Respiration 2008;76:121-7. [Crossref] [PubMed]
- Trump M, Gohar A. Diagnosis and treatment of pneumothorax. Hosp Pract (1995) 2013;41:28-39. [PubMed]
- Zarogoulidis P, Kioumis I, Pitsiou G, et al. Pneumothorax: from definition to diagnosis and treatment. J Thorac Dis 2014;6:S372-6. [PubMed]
- Zeng LC, Du Y, Yang HF, et al. Efficacy of an opposite position aspiration on resolution of pneumothorax following CT-guided lung biopsy. Br J Radiol 2015;88:20150227. [Crossref] [PubMed]
- Yamagami T, Kato T, Iida S, et al. Efficacy of manual aspiration immediately after complicated pneumothorax in CT-guided lung biopsy. J Vasc Interv Radiol 2005;16:477-83. [Crossref] [PubMed]
- Zidulka A, Braidy TF, Rizzi MC, et al. Position may stop pneumothorax progression in dogs. Am Rev Respir Dis 1982;126:51-3. [PubMed]
- Baumann MH, Strange C, Heffner JE, et al. Management of spontaneous pneumothorax: an American College of Chest Physicians Delphi consensus statement. Chest 2001;119:590-602. [Crossref] [PubMed]


