Neutrophil-to-lymphocyte ratio as a prognostic marker in acute respiratory distress syndrome patients: a retrospective study
Introduction
Acute respiratory distress syndrome (ARDS) is the leading cause of high mortality in intensive care units (ICUs) worldwide, affecting millions of people annually (1). Knowledge on epidemiological surveys of ARDS in China has been limited. Epidemiological surveys in Beijing, Shanghai, Chongqing and other regional cities found that the mortality from ARDS among ICU patients in China is variable (22–100%) (2). Although recent advances in intensive care models have been processed (3-4), mortality remains high (1). Therefore, ARDS remains a challenge to critical care medicine.
A prognostic marker for ARDS is particularly important given the absence of effective treatment strategies aside from small tidal volume ventilation. Acute Physiology and Chronic Health Evaluation II (APACHE II) scores and the Simplified Acute Physiology Score (SAPS) have been used to assess the prognosis for critically ill patients (5). However, these scores are not specific to ARDS. Zhang et al. (6) established a model to predict risk in ARDS patients. However, the application of this model requires many variables and complex formulas, and obtaining the required information is not convenient. Villar et al. (7) created a bedside score for ARDS called APPC, used only in patients with moderate/severe ARDS with protective mechanism ventilation. Moreover, several studies have been conducted to analyze biomarkers in ARDS patients (8-11). However, most current studies of biomarkers require special biological samples of patients, specific group of patients and integration with other clinical data. Thus, the complexity and heterogeneity of the disease makes this assessment very challenging.
Inflammation is known to play a significant role in the development of ARDS and has an impact on its prognosis and symptoms (12). The balance of cytokines and chemokines modulates ARDS pathogenesis. The neutrophil-to-lymphocyte ratio (NLR) is an indicator of systemic inflammation (13). High levels of neutrophil infiltration may be associated with cytotoxicity, vascular stasis and decreased inflammation in response to changes in the balance of pro-inflammatory and anti-inflammatory cytokines (12,14).
Several studies have reported that the NRL could be used in a variety of clinical conditions (15-17). Studies have shown a correlation between the NLR and the severity of the clinical course in ICU patients, and they have suggested that the NLR should be considered a prognostic indicator. Another study reported that the NLR is related to 28-day mortality in severe sepsis or septic shock patients (18). In addition, the NLR has merit due to its simplicity, low cost, and availability compared to other previously proposed biomarkers, making it practical and useful for prognostic indications.
Currently, no simple, routine, and reliable risk factors have been consistently identified to determine the prognosis of ARDS patients. To date, no studies have been reported regarding the relationship between the NLR and outcomes in ARDS patients. We conducted this retrospective study to investigate the potential prognostic value of the NLR in patients with ARDS.
Methods
Patient population
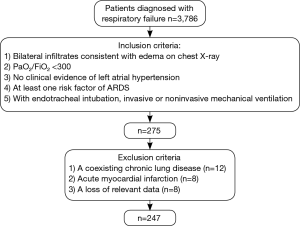
This study was approved by the Clinical Research Ethics Committee of Zhongshan Hospital, Fudan University (Shanghai, China) (B2016-039R). Between January 24, 2008, and July 24, 2015, 3,786 patients were diagnosed with respiratory failure in Zhongshan Hospital, Fudan University. Three medical doctors in the respiratory department at Zhongshan Hospital reviewed the medical records of all patients. A total of 275 patients who met the inclusion criteria were retrospectively enrolled in the study. Ultimately, 28 patients were excluded according to the exclusion criteria, and 247 patients (age 17–93 years) with ARDS were analyzed.
The inclusion criteria are shown in Figure 1. American-European Consensus Conference (AECC) criteria (19) were used in this study, and positive end expiratory pressure (PEEP) was not included in the inclusion criteria. The patient exclusion criteria are listed in Figure 1. Infiltrates on chest radiographs were evaluated by two independent medical doctors in the imaging department in Zhongshan Hospital.
Data collection and outcome measurements
Baseline data, including age, gender, APACHE II score, risk factors for ARDS, past medical history, ventilation status and experimental examination, were retrospectively collected from medical records and electronic databases. Data on survival were also retrospectively obtained from the medical records. The risk factors studied included pneumonia, non-pulmonary sepsis, aspiration of gastric contents and trauma. The past medical history obtained included surgical history, smoking history, and medical history, including malignant tumors, liver cirrhosis, hypertension and diabetes. The experimental examination included the following: PaO2, hematocrit (HCT), white blood cell (WBC) counts, neutrophil counts, lymphocyte counts, platelets counts, and levels of sodium (Na), potassium (K), blood urea nitrogen (BUN), creatinine (Cr) and albumin. These experimental examinations were recorded at 24 hours after the ARDS diagnosis. The NLR was determined from the blood cytology by dividing the neutrophil count by the lymphocyte count. Patients were categorized into two groups according to the median result of the initial NLR.
Statistical analysis
Data were analyzed using SPSS software version 22.0 (SPSS, Chicago, IL, USA) and GraphPad Prism 6 (GraphPad Software Inc., La Jolla, CA, USA). The difference between the two groups was tested using a two-tailed independent Student’s t-tests for normally distributed variables and the Wilcoxon rank sum test for non-normally distributed data. The associations between the NLR and patient baseline characteristics for non-parametrically distributed variables were assessed using the χ2 test, Fisher’s exact method, or the Cochran-Mantel-Haenszel χ2 test. Univariate and multivariate analyses were completed with Cox proportional hazards regression tests. The cut-off point for the definition of the NLR was based on the median data. The primary outcome and overall survival (OS) were defined as the time from the diagnosis of ARDS to death from any cause. Kaplan-Meier survival analysis was performed to compare the difference in the survival between higher and lower median NLR values. P<0.05 was considered statistically significant.
Results
Baseline patient characteristics
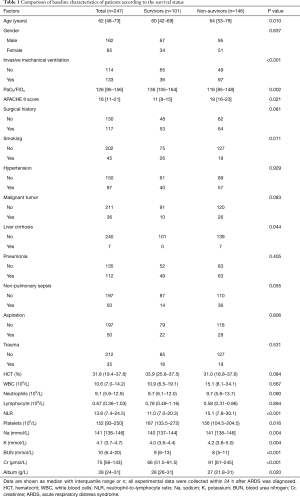
The baseline characteristics of the patients are shown in Table 1. The patients in our study consisted of 162 males and 85 females with a median age of 62 years (IQR 48–73 years), and the overall mortality rate was 59.1%. There was a history of smoking in 18.2% of the patients. Invasive mechanical ventilation was available for 133 patients. The most common underlying diagnosis was pulmonary infection (45.3%). Aspiration (20.2%) and non-pulmonary sepsis (20.2%) were the next most common diagnoses. The median value of the initial NLR was 13.8 (IQR, 7.4–24.5) for the overall group. The baseline median APACHE II score was 16 (IQR, 11–21). The baseline characteristics of the surviving and non-surviving patients in the hospital are also shown in Table 1. There was a significant difference between the groups in terms of age (P=0.010), invasive mechanical ventilation (P<0.001), PaO2/FiO2 (P=0.002), APACHE II score (P=0.021), smoking history (P=0.011) and liver cirrhosis (P=0.044). There were also significant differences in laboratory values, including the NLR (P<0.001), platelet count (P=0.016), and levels of Na (P=0.004), K (P=0.004), BUN (P<0.001), Cr (P<0.001) and albumin (P=0.020).
Full table
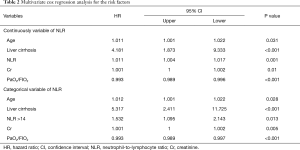
Independent risk factors of mortality in ARDS
In the multivariate Cox proportional hazard regression survival model, the factors with a P value less than 0.20 in Table 1 were added into the final model. In the multivariate proportional hazard Cox regression analysis, survival, age, liver cirrhosis, NLR, Cr and PaO2/FIO2 were statistically significant (Table 2). We concluded that the risk factors were age, liver cirrhosis and Cr. Meanwhile, only the PaO2/FIO2 was a protective factor. We also found that the NLR was an independent risk factor for each 1% increase in the ratio [hazard ratio (HR) 1.011; 95% CI, 1.004–1.017; P=0.03].
Full table
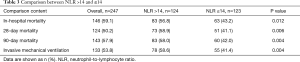
Characteristics of patients with an NLR >14
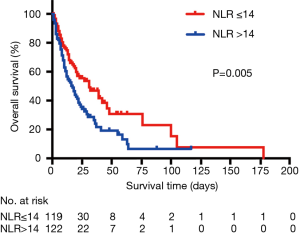
As the NLR was an independent risk factor for mortality in ARDS patients, we used the median value as the cut-off value to divide the patients into two groups (NLR >14 and ≤14). The influence of the NLR on mortality in ARDS patients was analyzed using the hospital mortality, 28-, 90-day mortality and invasive mechanical ventilation as outcomes (Table 3). The analysis showed that an NLR >14 was significantly associated with the outcomes for each variable. The Kaplan-Meier curve also demonstrated that an NLR >14 influenced the survival time of ARDS patients (Figure 2).
Full table
Stratified analysis of the NLR
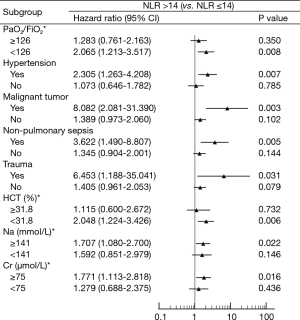
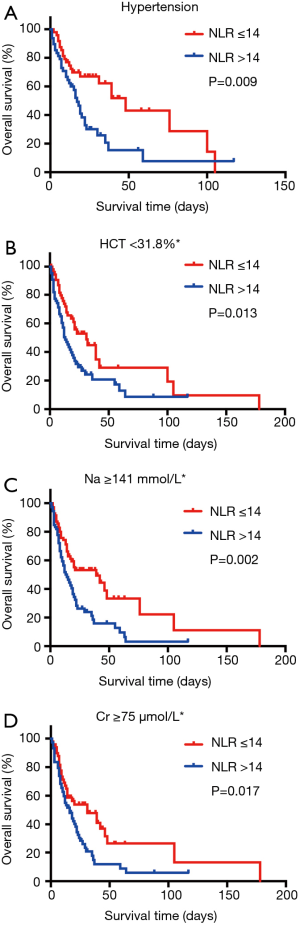
Figure 3 shows the comparison of clinical parameters for patients with an NLR >14. There was a significant difference between patients with a high NLR (NLR >14) and patients with a low NLR (NLR ≤14) in several subgroups. These subgroups were divided according to their median values. Multivariate Cox analysis identified an NLR >14 as an independent predictive factor for ARDS mortality (HR 1.532, 95% CI, 1.095–2.143, P=0.013) (Table 2). Upon stratified analysis, this trend was still observed in certain subgroups, such as the low PaO2/FIO2 (PaO2/FIO2 <126) (P=0.008), hypertension (P=0.007), malignant tumor (P=0.003), non-pulmonary sepsis (P=0.005), trauma (P=0.031), low HCT (HCT <31.8%) (P=0.006), high sodium (Na ≥141 mmol/L) (P=0.022) and high creatinine (Cr ≥75 µmol/L) (P=0.016) groups (Figure 3). Kaplan-Meier analyses also showed the predictive value of an NLR >14 in patients with hypertension (P=0.009), low HCT (P=0.013), high sodium (P=0.002) and high creatinine (P=0.017) (Figure 4).
Discussion
Our retrospective study revealed that an NLR measured at 24 hours after ARDS diagnosis was an independent risk factor of mortality in patients with ARDS. The NLR was higher in the group of non-survivors than in the survivors. The baseline NLR value could predict mortality independent of age, liver cirrhosis, NLR, Cr and PaO2/FiO2. In addition, NLR >14 was used as the cut-off threshold for predicting the mortality of ARDS. Prior to our study, data on ARDS in Chinese patients had not been well described, and the present study is the first to examine the prognostic role of the NLR in patients with ARDS.
Recent studies showed the role of the NLR as an independent predictor of mortality in various diseases, including in critical care medicine. In a prospective study of critically ill patients, a high NLR measured in the emergency department (ED) was independently associated with in-hospital mortality (20). In addition, a high NLR was also related to risk of multi-organ failure and the development of sepsis (18). More recently, Riché et al. also identified an association between NLR and risk of death in patients with septic shock (17). In a study conducted by Salciccioli et al. (20), NLR measured at the time of ICU admission was associated with 28-day mortality in unselected critically ill patients. Hwang et al. (18) also found that the initial NLR measured at ED admission was independently associated with 28-day mortality in patients with severe sepsis or septic shock in the ED. However, no study has explored the association between NLR and mortality in ARDS patients.
An increase in the NLR is due to an increase in the neutrophil count and a decrease in the lymphocyte count. The NLR represents the balance between the neutrophil and lymphocyte levels in the body, and it is an indicator of systemic inflammation (13). In this case, a high NLR may indicate that a patient has severe inflammatory progression. Studies have shown that extensive activation of the immune system and immune dysfunction can explain the changes in the neutrophil and lymphocyte counts (17,18). On the other hand, the release of various anti-inflammatory cytokines induces immunosuppression and apoptosis in many lymphocytes (21,22). In this case, neutrophils are continuously released from the bone marrow, resulting in many immature neutrophils recruited into the cycle. Lymphopenia has been found to be an indication of immunosuppression in sepsis (23) and may be a predictor of mortality in ARDS patients.
ARDS is the out-of-control progression of the innate immune-mediated inflammatory response in the context of various risk factors. A variety of inflammatory factors promote the permeability of the alveolar epithelium and vascular endothelial boundary (24). New mechanisms of the innate immune response have been found, such as neutrophils forming extracellular traps (25) in response to endothelial injury and the release of histones, which may cause alveolar damage. The recruitment of neutrophils is mediated by a step-by-step response to inflammatory factors released from endothelial cells, which is further enhanced in ARDS (25). The innate immune recognition process is considered a potential driver of acute lung injury. Neutrophil-dependent lung injury is the key pathway. Neutrophils respond rapidly to inflammation, resulting in a dramatic increase in the number of neutrophils migrating to the lungs (12). Severe and uncontrolled activation of the immune system can lead to lung injury, which is followed by multiple organ failure or death.
Our study revealed the relationship between the NLR and prognosis in ARDS patients. We observed that there were significant differences in the NLR between the survival and non-survival groups (P<0.001). As a high NLR was more likely to indicate a higher mortality, we used a median value as the cut-off value to divide the patients into two groups: NLR >14 and ≤14. The influence of an NLR >14 on the mortality of ARDS patients was analyzed using hospital mortality, 28-, 90-day mortality and mechanical ventilation as outcomes. The Kaplan-Meier curve also demonstrated that an NLR >14 was associated with a reduced OS (P=0.005). These results might imply that an NLR >14 could be associated with a more effective relative prognosis in ARDS. Multivariate analysis identified an NLR >14 as an independent prognostic factor of OS (P=0.029). Subgroup analysis confirmed that the NLR was a prognostic factor of OS in patients with hypertension (P=0.009), HCT <31.8% (P=0.013), Na ≥141 mmol/L (P=0.002) and Cr ≥75 µmol/L (P=0.017). Therefore, we advocate for the use of the NLR in the risk stratification of ARDS patients.
Although many studies have evaluated the prognosis of ARDS (10), no biomarker is considered perfect. The NLR is an extremely common laboratory test, and the initial NLR values can be used to identify high-risk patients with adverse outcomes. These values may also help to assess the host immune response. However, further clinical studies are needed to evaluate the benefit of the NLR in ARDS.
The major limitations of our study are its retrospective design and relatively small sample size. This is a single institution study with a single ethnicity study population, and it remains to be seen whether these results are generalizable to other ethnicities. Future studies on this consideration as well as prospective external validation are required. Additionally, we separated the patients into two groups based on the percentage of the initial NLR. However, the baseline characteristics of the patients were heterogeneous and unbalanced. Moreover, the new definition of ARDS in the context of the Berlin definition was not implemented in this study (26).
Conclusions
Our study showed that a high NLR (>14) at 24 hours after an ARDS diagnosis independently predicted a poor prognosis in ARDS patients. This marker could potentially be used in clinical practice due to its convenience. However, further studies in different ethnicities and larger populations of ARDS patients are required to confirm the current findings.
Acknowledgements
Thanks are due to Wenhai Jiang of Information Department in Zhongshan hospital Fudan university for assistance with the collection of information.
Funding: This research was supported by the National Natural Science Foundation of China [81500026, 81490533, 81570028, 81400018, 81400002, 81400043, 81300055] and Shanghai Science and Technology Committee (15DZ1930602). Dr. Y Song was supported by the State Key Basic Research Program [973] project (2015CB553404) and Doctoral Fund of Ministry of Education of China (20130071110044).
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: This study was approved by the Clinical Research Ethics Committee of Zhongshan Hospital, Fudan University (Shanghai, China) (B2016-039R).
References
- Li G, Malinchoc M, Cartin-Ceba R, et al. Eight-year trend of acute respiratory distress syndrome: a population-based study in Olmsted County, Minnesota. Am J Respir Crit Care Med 2011;183:59-66. [Crossref] [PubMed]
- Song Y, Xu F, Seeley EJ, et al. Acute respiratory distress syndrome: emerging research in China. Am J Respir Crit Care Med 2014;190:1090-3. [Crossref] [PubMed]
- Needham DM, Yang T, Dinglas VD, et al. Timing of low tidal volume ventilation and intensive care unit mortality in acute respiratory distress syndrome. A prospective cohort study. Am J Respir Crit Care Med 2015;191:177-85. [Crossref] [PubMed]
- Sud S, Friedrich JO, Adhikari NK, et al. Effect of prone positioning during mechanical ventilation on mortality among patients with acute respiratory distress syndrome: a systematic review and meta-analysis. CMAJ 2014;186:E381-90. [Crossref] [PubMed]
- Bajwa EK, Malhotra CK, Thompson BT, et al. Statin therapy as prevention against development of acute respiratory distress syndrome: an observational study. Crit Care Med 2012;40:1470-7. [Crossref] [PubMed]
- Zhang Z, Ni H. Prediction model for critically ill patients with acute respiratory distress syndrome. PLoS One 2015;10:e0120641. [Crossref] [PubMed]
- Villar J, Ambros A, Soler JA, et al. Age, PaO2/FIO2, and Plateau Pressure Score: A Proposal for a Simple Outcome Score in Patients With the Acute Respiratory Distress Syndrome. Crit Care Med 2016;44:1361-9. [Crossref] [PubMed]
- Calfee CS, Ware LB, Glidden DV, et al. Use of risk reclassification with multiple biomarkers improves mortality prediction in acute lung injury. Crit Care Med 2011;39:711-7. [Crossref] [PubMed]
- Nakashima T, Yokoyama A, Inata J, et al. Mucins carrying selectin ligands as predictive biomarkers of disseminated intravascular coagulation complication in ARDS. Chest 2011;139:296-304. [Crossref] [PubMed]
- Binnie A, Tsang JL, dos Santos CC. Biomarkers in acute respiratory distress syndrome. Curr Opin Crit Care 2014;20:47-55. [Crossref] [PubMed]
- Ichikawa A, Kuba K, Morita M, et al. CXCL10-CXCR3 enhances the development of neutrophil-mediated fulminant lung injury of viral and nonviral origin. Am J Respir Crit Care Med 2013;187:65-77. [Crossref] [PubMed]
- Famous KR, Delucchi K, Ware LB, et al. Acute Respiratory Distress Syndrome Subphenotypes Respond Differently to Randomized Fluid Management Strategy. Am J Respir Crit Care Med 2017;195:331-8. [PubMed]
- Zahorec R. Ratio of neutrophil to lymphocyte counts--rapid and simple parameter of systemic inflammation and stress in critically ill. Bratisl Lek Listy 2001;102:5-14. [PubMed]
- Summers C, Singh NR, White JF, et al. Pulmonary retention of primed neutrophils: a novel protective host response, which is impaired in the acute respiratory distress syndrome. Thorax 2014;69:623-9. [Crossref] [PubMed]
- Benites-Zapata VA, Hernandez AV, Nagarajan V, et al. Usefulness of neutrophil-to-lymphocyte ratio in risk stratification of patients with advanced heart failure. Am J Cardiol 2015;115:57-61. [Crossref] [PubMed]
- Cannon NA, Meyer J, Iyengar P, et al. Neutrophil-lymphocyte and platelet-lymphocyte ratios as prognostic factors after stereotactic radiation therapy for early-stage non-small-cell lung cancer. J Thorac Oncol 2015;10:280-5. [Crossref] [PubMed]
- Riché F, Gayat E, Barthelemy R, et al. Reversal of neutrophil-to-lymphocyte count ratio in early versus late death from septic shock. Crit Care 2015;19:439. [Crossref] [PubMed]
- Hwang SY, Shin TG, Jo IJ, et al. Neutrophil-to-lymphocyte ratio as a prognostic marker in critically-ill septic patients. Am J Emerg Med 2017;35:234-9. [Crossref] [PubMed]
- Bordes J, Lacroix G, Esnault P, et al. Comparison of the Berlin definition with the American European consensus definition for acute respiratory distress syndrome in burn patients. Burns 2014;40:562-7. [Crossref] [PubMed]
- Salciccioli JD, Marshall DC, Pimentel MA, et al. The association between the neutrophil-to-lymphocyte ratio and mortality in critical illness: an observational cohort study. Crit Care 2015;19:13. [Crossref] [PubMed]
- Tian J, Avalos AM, Mao SY, et al. Toll-like receptor 9-dependent activation by DNA-containing immune complexes is mediated by HMGB1 and RAGE. Nat Immunol 2007;8:487-96. [Crossref] [PubMed]
- Adamzik M, Broll J, Steinmann J, et al. An increased alveolar CD4 + CD25 + Foxp3 + T-regulatory cell ratio in acute respiratory distress syndrome is associated with increased 30-day mortality. Intensive Care Med 2013;39:1743-51. [Crossref] [PubMed]
- Drewry AM, Samra N, Skrupky LP, et al. Persistent lymphopenia after diagnosis of sepsis predicts mortality. Shock 2014;42:383-91. [Crossref] [PubMed]
- Thille AW, Esteban A, Fernandez-Segoviano P, et al. Chronology of histological lesions in acute respiratory distress syndrome with diffuse alveolar damage: a prospective cohort study of clinical autopsies. Lancet Respir Med 2013;1:395-401. [Crossref] [PubMed]
- Mantovani A, Cassatella MA, Costantini C, et al. Neutrophils in the activation and regulation of innate and adaptive immunity. Nat Rev Immunol 2011;11:519-31. [Crossref] [PubMed]
- ARDS Definition Task Force, Ranieri VM, Rubenfeld GD, et al. Acute respiratory distress syndrome: the Berlin Definition. JAMA 2012;307:2526-33. [PubMed]