Completely thoracoscopic right upper lobectomy and mediastinal lymph node dissection
Introduction
Video-assisted thoracoscopic surgery (VATS) has been constantly used in the diagnosis and treatment of intrathoracic disease after Roviaro and his associates firstly reported anatomic lobectomy in completely thoracoscopic operation (1). Compared with conventional open thoracotomy, VATS has advantages of minimal invasiveness, improved recovery times, short hospital stay, cosmetic appearance. But, minimally invasive procedure has to be converted to open thoracotomy due to massive hemorrhage, which increases the risk of operation and the injury to patient. Therefore, how to effectively control hemorrhage is becoming more and more important in VATS approach.
Single-direction lobectomy is a safe and feasible thoracoscopic lobectomy in minimally invasive approach (2,3). Single-direction lobectomy is defined as the operation mainly accomplished in hilar root with dissection along the only direction around the superficial structure of the hilum step by step. The operation is progressed to posterior in lobectomy of upper lobe and middle lobe, meanwhile progressed to superior in lobectomy of inferior lobe. There is no need of repeated overturn of the lobe during the operation.
Clinical information
A 60-year-old woman surnamed Huang was admitted to hospital due to physical examination revealing the tumor of the right upper lobe. She denied the smoking history. CT was performed after hospitalization and demonstrated there was strong possibility of lung cancer of right upper lobe. There was no evidence of pathological change by bronchoscopy. The remote metastases to brain, bone, liver and adrenal gland were excluded. There were no abnormalities in lung function and routine blood test. There was no contraindication for surgery.
Preoperative assessment
It is essential of preoperative assessment for patient. The patient had no history of hypertension and diabetes mellitus. Blood tests were normal including blood routine examination, biochemistry, coagulation item and screen for infectious disease. Pulmonary function tests showed mild ventilation impairment. Patient could climb five flights of stairs. Bone scanning and brain MRI showed no evidence of brain metastases and bone metastases. There was no metastatic evidence of liver and adrenal gland by color Doppler ultrasound. CT demonstrated the strong possibility of lung cancer of right upper lobe and no unequivocal enlargement of mediastinal node (Figures 1,2). Clinical diagnosis was considered lung cancer with clinical stage IA (cT1N0M0).
Anaesthesia and positioning
General anesthesia was induced via a double-lumen tube (32F) for one lung ventilation, which facilitated the handling.
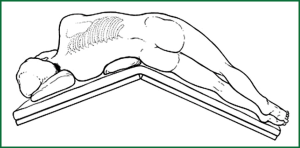
The patient was placed in the full lateral decubitus position and knife position (the bed was flexed to make the sides of head and foot bend downward approximately 15 degrees), which increased the intercostal space and reduced pressure on intercostal nerves (Figure 3). It achieved reduction in postoperative pain and enhanced the handling.
Surgical technique
The operation (Video 1) was accomplished under the condition of general anesthesia and double-lumen endotracheal intubation and one-lung ventilation. The camera port (1.2 cm in length) was placed at the seventh interspace along the right middle axillary line. The utility incision (3 cm in length) was placed at the third interspace along the right anterior axillary line; the posterior port (2 cm in length) was placed at the ninth interspace between right posterior axillary line and scapular line. Surgical instruments including ultrasonic scalpel, aspirator with holes, double-joint oval forceps, electrocoagulation hook and so on could meet the demand of operation. Tumor was not directly discovered due to absence of invasion to the pleura. We finally localized the tumor after using the oval forceps to clamp the segment in which tumor was situated. Lung parenchyma including tumor was sent for pathologic examination. Single-direction thoracoscopic lobectomy was performed when frozen section examination revealed the adenocarcinoma of right upper lobe (2,3). The operation was dissected along the only direction without more overturn and retraction of the lobe. From the front to the back, we successively manipulated the artery, vein and bronchus of the right upper lobe. Dissections of fissure and lymph nodes were finally manipulated. Details as followed.
Firstly, the mediastinal pleura over the anterior aspect of the right hilum was incised by electrocoagulation hook to provide exposure to the anatomic structure. The mediastinal pleura was incised posterior to the phrenic nerve which was protected. Further dissection of right hilum exposed the veins of the upper lobe and middle lobe, which avoided the mistaken ligation of the vein of the middle lobe occasionally due to common vein between the upper and middle lobe. From our experience, full exposure can be obtained by dissection in intravascular sheath. In addition, the vein of the right upper lobe was lifted by silk suture number 7, which provided access for ETHICON Endo-GIA stapler because of the exposure of the vascular space. The camera lens was sheltered from the bleeding of apical segment for the over tension to the artery dissected. Meanwhile, the surgeon swiftly used the aspirator to compress the bleeding spot. The bleeding was controlled when the lens was wiped clearly. Titanium clip was used to clamp the artery for hemostasis. The right upper bronchus was then exposed posteriorly, and clamped by ETHICON Endo-GIA stapler. Before the excision of the right upper bronchus, care must be taken to expand retained lung so as to avoid mistaken ligation. Fissure was opened along the atelectatic lung by ETHICON Endo-GIA stapler and the right upper lobectomy ensued. The advantage of the procedure is that it does not necessitate dissection of the incomplete fissure and reduces difficulty of the operation.
After the completion of lobectomy, the right upper lobe was retrieved in a specimen bag (surgical glove) through the utility incision to avoid possible tumor cell implant.
Mediastinal lymph node dissection as followed: Subcarinal node was first dissected, and then mediastinal pleura was opened from posterior to superior vena cava by electrocoagulation hook in order to dissect 2R, 4R lymph nodes. The bleeding spot was seen at the posterolateral wall of superior vena cava, and similarly compressed by the aspirator. We continued dissection of 2R, 4R lymph nodes after the bleeding spot was sutured for hemostasis. Our experience is that an aspirator is used to elevate the azygos vein, and the lymph nodes are removed superiorly by ultrasonic scalpel, and then the lymph nodes are resected with En Bloc removal.
We cleaned the thoracic cavity with sterile normal saline after complete hemostasis and placed a chest tube of number 32 through camera hole. The incision was closed after we confirmed the expansion of remained lung.
Postoperative management
Intravenous analgesic pump was administered in order to alleviate the pain which induced the pulmonary infection because of the fear of cough. Semiliquid diet was permitted six hours after operation and meanwhile antibiotics, nebulization and support therapy were administered. Attention was paid to the speed of fluid infusion in order to avoid pulmonary edema. The plain chest radiograph was made to understand the lung reexpansion on the first day postoperatively. The patient was encouraged to breathe deeply and conducted to cough effectively to decrease the incidence rate of pulmonary infection. If atelectasis occurs in senile patients because of inability to cough, flexible bronchoscopy may be advantageous to provide a route for tracheal and bronchial suction in favor of lung reexpansion. The patient was pathologically confirmed as adenocarcinoma of right upper lobe with negative bronchial margin. Pathological demonstration of lymph nodes as followed: right level 2 lymph nodes: 1/3, right level 4 lymph nodes: 0/5, level 7 lymph nodes: 0/5, level 8 and, level 10 lymph nodes: 0/5. Pathological staging was pT1N2M0 (IIIA stage).
Discussion
Compared with conventional open thoracotomy with anatomic dissection, single-direction thoracoscopic lobectomy of the video had more advantages as follows: first, make it easier to be understood and handled for novice; second, reduce the lung injury due to repeated overturn of the lobe; third, lower the difficulty of operation owing to finally handling the incomplete fissure which could increase the difficulty of operation; fourth, save the operation time; fifth, lower rate of air leakage after operation.
Previously, thoracoscopic lobectomy was often converted to open thoracotomy due to incomplete fissure and bleeding. Vessels and bronchus was taken precedence over fissure via handling dissection in the single-direction thoracoscopic lobectomy, which averted the difficulty of operation. In the meantime, the success rate of thoracoscopic lobectomy further increased through the skillful hemostasis. Aspirator was confined to suction in the past. Arterial bleeding happened due to the over tension to the artery that was dissected. But the surgeon immediately used the “side compression for hemostasis with the aspirator” to effectively stop bleeding and used Titanium clip to clamp the artery for hemostasis (4). In the same way, an endoscopic aspirator was used to control bleeding when bleeding spot was seen at the posterolateral wall of superior vena cava. Then angiorrhaphy was made to avoid more injury to the patient due to conversion to open thoracotomy.
In the video of the thoracoscopic handling, aspirator was used not only for suctioning but also compression of bleeding spot along with separation and retraction of the tissue. The more replacement and insertion of surgical instruments can be avoided, which makes the operation field clear and facilitates the operation and shortens operation time. In my opinion, skillful manipulation of aspirator is operational highlight of the video.
Acknowledgements
Informed consent of “assignment of copyright” was made and the patient was confirmed to sign the informed consent.
Disclosure: The authors declare no conflict of interest.
References
- Roviaro G, Rebuffat C, Varoli F, et al. Videoendoscopic pulmonary lobectomy for cancer. Surg Laparosc Endosc 1992;2:244-7. [PubMed]
- Liu L, Che G, Pu Q, et al. A new concept of endoscopic lung cancer resection: Single-direction thoracoscopic lobectomy. Surg Oncol 2010;19:e71-7. [PubMed]
- Liu LX, Che GW, Pu Q, et al. Completely single-direciton thoracoscopic lobectomy. Chin J Thorac Cardiovasc Surg 2008;24:156-8.
- Mei J, Pu Q, Liao H, et al. A novel method for troubleshooting vascular injury during anatomic thoracoscopic pulmonary resection without conversion to thoracotomy. Surg Endosc 2013;27:530-7. [PubMed]