Video-assisted thoracolaparoscopic esophagectomy: the experience of Shanghai Chest Hospital
Introduction
China is one of the countries with high incidence of esophageal squamous carcinoma, and its morbidity remains the fifth in malignant tumors in China. Surgery is the first choice of esophageal carcinoma treatment, and subtotal esophagectomy with systematic lymphadenectomy is gradually well accepted. But the traditional Ivor-Lewis surgery or Mckeown procedure is associated with wider range of operation wound and higher morbidity. A mortality rate reported from experienced centers is in the range of 6-7% (1), and in low-volume centers, the rate is as high as 23%. Since the improvements in surgical instruments have been made, advanced minimally invasive surgical procedures in thoracic surgery are performed more frequently in recent years.
Operative techniques
The patient is placed in the prone-decubitus position, leaning at a 60-degree angle in the thoracoscopic procedure. The surgeon is standing in front of the patient. The prone-decubitus position could facilitate the lung leaning forward to provide a better exposure of posterior mediastinum, therefore in this procedure, the assistant is not necessary, and surgeon could perform the extraction of lung independently. We adopt “four ports” approach, the observation port lies at the midaxillary line in the seventh intercostal space, main working port is located at the midaxillary line in the third/fourth intercostal space (A), secondary working ports is lying at the scapular line in the seventh (B) and ninth (C) intercostal space. Management of upper/middle segment of esophagus is performed with left hand in B/C and right hand in A; and management of lower segment is performed with left hand in C and right hand in B. 5 mm trocar is used in secondary port, while 10 mm trocar is used in the other ports. All the trocars are gas proof for establishing the artificial pneumothorax (APT) (Video 1).
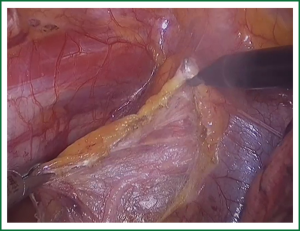
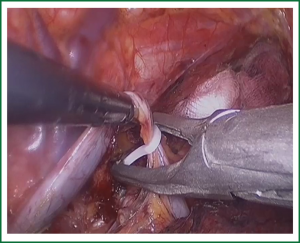
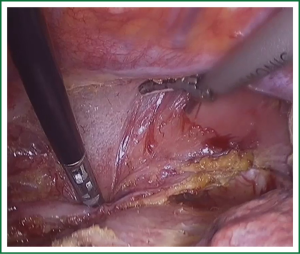
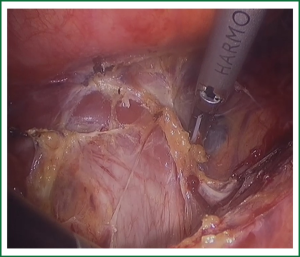
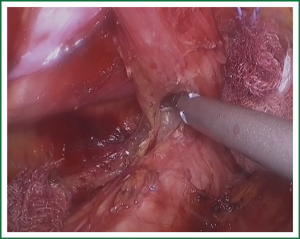
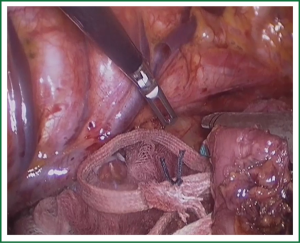
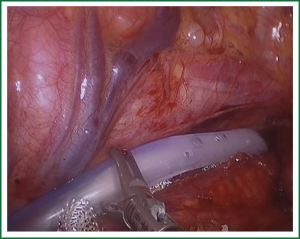
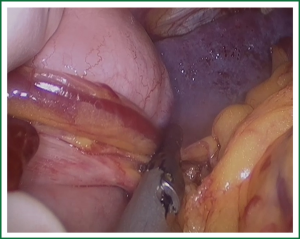
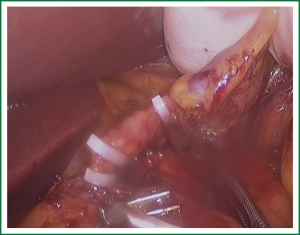
In the laparoscopic procedure, “hand assistant technique” is employed, which is a “hand” incision lie under the xiphoid. There are additional three ports: one is observing port lying on the left of the navel; one is the primary port lying on the right of the navel; and the assistant port is lying below the left costal arch with 5 mm trocar. The first thing in the procedure is to explore the esophageal carcinoma, if it is resectable, sequential operation will be performed. The first step is the dissection of right recurrent laryngeal never lymph node, upper mediastinal pleural is cut to expose the vagus never and right subclavical artery (showed in Figure 1), then the right recurrent laryngeal never follow the artery is anatomized. When finding the never, the lymph nodes among the never, esophagus and trachea are dissected. The second step is the division of the azygos vein arch with Hem-o-lok (Figure 2). The third step is cutting the middle/lower mediastinal pleural along the azygos vein and thoracic aorta, and in the other side along the right main bronchus and right lung from azygos vein arch to diaphragm. The fourth step is ligating all the esophageal arteries with Harmonic or clip along the aorta (Figure 3), and the thoracic duct should be noted. From our perspective, because of the gas leakage in building the pneumoperitoneum, it is not necessary to cut the pleural reflection during the dissection of the hiatus (Figure 4).
If the esophagus is dissected using Harmonic, attention should be given to put the working side facing the esophagus to avoid injury of the membranous part of trachea and bronchus. There is a fixed bronchial artery coming from the aorta arch striding over the esophageal surface on the azygos vein arch level which we usually divide. The fifth step is the mobilization of upper esophagus, care should be taken to the left recurrent never when drawing the esophagus (Figure 5). Then, the left recurrent nerve lymph node is explored. The last step in thorax is dividing the esophagus with endocutter and connecting it with a cotton tape (Figure 6). Before closing the incision, one chest tube and one mediastinal drainage are placed (Figure 7).
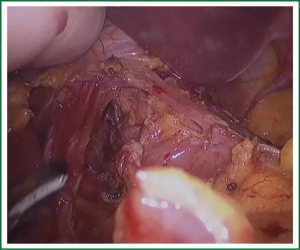
In the laparoscopic procedure, with hand assistant, it will be easy for the beginners of laparoscopic surgery. The greater gastric curvature is excised, then the short gastric arteries and posterior gastric artery (Figure 8) are divided, the lesser omentum is cut to expose the left gastric vessel in the top of pancreas, the vein is divided by clip and the artery by Hem-o-lok (Figure 9). Finally, the hiatus is opened and the esophagus and stomach are taken out from the abdominal cavity to make the gastric tube (Figure 10). Esophagogastric anastomosis is similar with McKeown procedure.
Comments
There is a current debate exists as to whether thoracolaparoscopic esophagectomy are more safe and practicable than traditional open procedures. What are the advantages of minimally invasive esophagectomy? Is it decreasing the mortality and morbidity? Mamidanna (2) reported MIE results in less postoperative functional complications, similar technical complications but with more intervention after summing short-term outcomes following open versus minimally invasive esophagectomy for cancer in England. Kinjo et al. (3) reported that operation with the help of minimally invasive endoscope technology in esophagus caner might decrease the occurrence of functional complication. Zingg et al. (4) also observed that MIE could be possible to decrease the risk of pulmonary complication and respiratory failure. Luketich et al. (5) reviewed 222 cases of MIE, in his series, and found that the mortality is 1.4%, the cardiopulmonary complication is 12.5%, nevertheless in concurrent report (6) of open esophagectomy, and the cardiopulmonary complication is up to 37%. So far, there has not been a phase III clinical trial to prove the oncological long-term outcome of MIE, Luketich et al. (5) just reported its stage specific survival was similar to that of open series in his largest group of MIE. Therefore, it needs to wait the result of the intergroup trial (ECOG 2202) to assess MIE in a multicenter setting.
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- Birkmeyer JD, Siewers AE, Finlayson EV, et al. Hospital volume and surgical mortality in the United States. N Engl J Med 2002;346:1128-37. [PubMed]
- Mamidanna R, Bottle A, Aylin P, et al. Short-term outcomes following open versus minimally invasive esophagectomy for cancer in England: a population-based national study. Ann Surg 2012;255:197-203. [PubMed]
- Kinjo Y, Kurita N, Nakamura F, et al. Effectiveness of combined thoracoscopic-laparoscopic esophagectomy: comparison of postoperative complications and midterm oncological outcomes in patients with esophageal cancer. Surg Endosc 2012;26:381-90. [PubMed]
- Zingg U, Smithers BM, Gotley DC, et al. Factors associated with postoperative pulmonary morbidity after esophagectomy for cancer. Ann Surg Oncol 2011;18:1460-8. [PubMed]
- Luketich JD, Alvelo-Rivera M, Buenaventura PO, et al. Minimally invasive esophagectomy: outcomes in 222 patients. Ann Surg 2003;238:486-94; discussion 494-5. [PubMed]
- Bailey SH, Bull DA, Harpole DH, et al. Outcomes after esophagectomy: a ten-year prospective cohort. Ann Thorac Surg 2003;75:217-22; discussion 222. [PubMed]