The management of chemical pleurodesis with viscum album in patients with persistent air leakage
Introduction
Persistent air leak (PAL) is an occasionally encountered difficult problem in the management of patients with major pulmonary resection or underlying secondary lung disease. It has been reported to occur up to 26% of patients after major pulmonary resection (1). These air leaks denote a significant cause of morbidity and cost as it prolongs chest tube indwelling, and increase risk of infection, pain and length of hospital stay (1). There have been various ways to resolve the PAL, such as prolonged chest tube drainage, surgical repair, chemical agent pleurodesis or blood patch pleurodesis. Besides, diverse techniques have been contrived for the purpose of decreasing the incidence of PAL including the application of visceral pleural sealants (2), pleural tents (3), and alternate suction-water seal (4), etc. However, there is actually no ideal strategy on the most efficacious treatment of PAL. Recently, chemical pleurodesis is generally recognized as a practical therapeutic tool to manage the patients with PAL. Many agents such as talc, iodopovidone, taurolidine, minocycline, autologous blood, OK432 have been introduced for this procedure (5-8). There is no global consensus on the best chemical agent for pleurodesis. An ideal chemical agent for pleurodesis should have a high molecular weight and chemical polarity, rapid systemic clearance, low regional clearance, easily available and minimal or no side effects (9). It is practically hard to find out such ideal agents. Among them, viscum album (fraxini) extract is a new chemical agent for pleurodesis, and only a few studies have reported outcomes of chemical pleurodesis in the treatment of malignant pleural effusion. Furthermore, the complications related to pleurodesis using viscum album are very rare in comparison with other substances. Viscum album (fraxini), also known as European mistletoe, contains a number of biologically active compounds, mostly the mistletoe lectins, viscotoxins, and other low molecular weight proteins, which exert immune-modulatory, cytotoxic, apoptotic, and anti-angiogenic effects (10). This study was aimed at the analysis of clinical efficacy and safety of viscum album (fraxini) pleurodesis in patients with intractable prolonged air leakage. The primary endpoint was focused on success rate of pleurodesis assessed on chest radiography and cessation of the air leak after procedure. Secondary endpoints included the mean length to cessation of air leak, duration of chest tube indwelling after pleurodesis, mean number of pleurodesis, and length of hospitalization. Other side effects or complications such as pain, fever and respiratory problems after pleurodesis procedure were also evaluated.
Methods
Study design and patients
All patients undergoing chemical pleurodesis because of prolonged air leak are sequentially registered in our institution. These registries contain baseline characteristics of patients, post-procedural evaluation data and results or other relevant complications. We retrospectively analyzed the clinical results of patients who underwent viscum album (fraxini) instillation for the management of PAL from February 2013 to February 2015. Patients were included in the study if moderate air leakage persists more than 4 days after pulmonary resection surgery or tube thoracostomy procedure due to intractable pneumothorax with underlying secondary lung disease like pulmonary tuberculosis, empyema, or chronic obstructive pulmonary disease (COPD). Surgical and procedural consent was naturally obtained from all patients. A total of 73 patients with PAL underwent chemical pleurodesis using viscum album extract from February 2013 to February 2015. We reviewed medical records and obtained such data as patient’s basic characteristics, diagnosis, number of procedure, length to cessation of air leak, chest tube indwelling time after pleurodesis, hospitalization. Other subjective pain score with visual analogue scale (VAS) and fever (tympanic temperature >38.0 °C) were also evaluated. The study was approved by Institutional Review Board of Konkuk University Medical Center (No. 1080025).
Pleurodesis procedures (viscum album)
Pleurodesis was performed at the bedside through an indwelling chest tube. The viscum album instillation fluid was prepared with 100 mg of viscum album extract (Abnobaviscum F®, Abnobapharma, Seoul, Korea) and 20 mL of normal saline. Prior to instillation, 200 mg of 2% lidocaine was applied via chest tube for premedication. The chest tube was not clamped. The connected tube line was lifted up about 1 m off the ground. Patients were asked to change their position on the bed every 10 minutes for about 1 to 1.5 hour. The posture was shifted alternately in accordance with bilateral decubitus, supine, prone, and knee-chest positions. The chest tube was connected to a water seal during pleurodesis, and continuous negative suction was restarted after pleurodesis. The patients had chest radiographs taken once a day after pleurodesis. Chest pain or discomfort after pleurodesis was recorded on a VAS from 0 to 10. Pulse, blood pressure, respiratory rate and temperature were measured before and every 60 minutes after the procedure for 12 hours. Patients received diclofenac (90 mg) intramuscularly as needed after the procedure.
End points and criteria
The criteria for removal of the chest tube were fully expanded lung on chest X-ray (CXR), cessation of the air leak, and pleural effusion of <150 mL/day. The cessation of air leak was routinely checked every 8 hours. If the air leak had not stopped within 24 hours after 1st instillation, pleurodesis was repeated using viscum album (fraxini) as same manner. The PAL which is necessary more than three episodes of instillation was regarded as a failure of pleurodesis.
Results
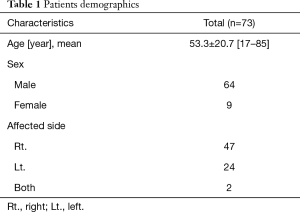
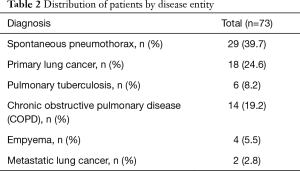
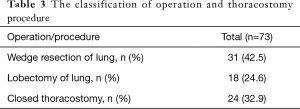
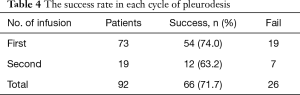
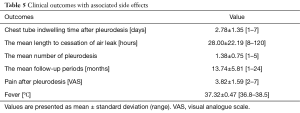
Out of 73 patients who underwent viscum album (fraxini) pleurodesis, 64 patients (87.7%) were predominantly male, and mean age was 53.3±20.7 ranging from 17 to 85 (Table 1). Majority of patients had spontaneous pneumothorax (39.7%) and lung cancer (24.6%) (Table 2). A single closed thoracostomy was performed in 24 patients (32.9%) with secondary spontaneous pneumothoax due to underlying pulmonary disease such as COPD, pulmonary tuberculosis or empyema entity. Thirty-one patients (42.5%) underwent pulmonary wedge resection surgery for spontaneous pneumothorax or metastatic lung cancer, while 18 patients (24.6%) had operation of lobectomy for primary lung cancer (Table 3). Overall, 66 patients (90.4%) fulfilled success criteria of air leakage cessation with viscum album infusion only. With regard to number of pleurodesis procedure, pleurodesis was successful in 66 patients (71.7%) out of 92 total attempts. The air leak was stopped on the first attempt in 54 patients (74.0%). A second round was successful in 12 patients (63.2%) out of 19 patients (Table 4). Meanwhile, seven patients needed more than three episodes of instillation for the prolonged air leak. One patient had 4 times of pleurodesis, who died of pneumonia not related to the procedure. Others (six patients) stopped the air leak in the third pleurodesis attempt. The mean number of pleurodesis was 1.38±0.75 (range, 1–5). The mean length to cessation of air leak was 28.00±22.19 hours (range, 8–120 hours). Chest tube indwelling time after pleurodesis was 2.78±1.35 days (range, 1–7 days). The mean post-treatment follow up period was 13.74±5.81 months (range, 1–24 months) (Table 5). During the follow up period, recurrence episodes were not observed. One of the most common complications of viscum album pleurodesis was regional chest pain. The majority of patients complained of mild to moderate myalgia and chest discomfort. The mean VAS score [0–10] was 3.82±1.59 (range, 2–7). The majority of patients did not require more than one extra dose of intravenous tramadol in addition to that given as routine premedication. There were 36 patients (49.3%) who want to receive pain killer, and diclofenac (90 mg) was administered intramuscularly at once. Fever over 38.0 °C occurred in 12 patients (16.4%), but resolved spontaneously within 24 hours. None of the patients developed acute respiratory distress syndrome (ARDS), empyema or hypotension associated with application of viscum album agent. There were no involved mortalities, either.
Full table
Full table
Full table
Full table
Full table
Discussion
The definition of prolonged air leak has been described to be an air leak that persists for more than 4 to 10 days after surgery (11). PAL is one of the most common complications after thoracic surgery such as mobilization or major pulmonary resection, which causes significant morbidities, increased hospitalization, cost, and relevant pain (11-13). PAL has been reported to develop up to 26% of patients after pulmonary resection (14). Air leaks more than 7 days have been even associated with an empyema up to 8.2% compared with 0% in patients without PAL (15). In addition, PAL can be easily encountered after tube thoracostomy procedure due to intractable pneumothorax with severe underlying secondary lung disease such as pulmonary tuberculosis, empyema, bullous emphysematous lung disease, or COPD. Chemical pleurodesis is widely recommended in the treatment of PAL in many different pathologic conditions as well as malignant pleural effusions or chylothorax (16). Infusion of a sclerosing agent into the pleural space implies that it obliterates the visceral and parietal pleural surfaces by an inflammation reaction with the intention of preventing the accumulation of either air or fluid in the pleural space. Pleurodesis is principally aimed at the palliation of malignant pleural effusions or recurrent pneumothorax. There are numerous chemical agents (fibrin glue, erythromycin, OK-432, tetracycline, 50% glucose solution, autologous blood patch and talc slurry, etc.) in order to produce pleural symphysis. Several studies have investigated the efficacy and complications of them. Generally, minor complications like fever, regional chest pain, tachycardia, and respiratory discomfort were usually reported. One of the most commonly used pleurodesis agents is talc, which is known to be most effective substance. However, there have been not a few of reports related to its serious complications such as ARDS, acute pneumonitis, pulmonary edema and infiltrations (17-19). Besides, it has also several drawbacks like high costs, various particle size, impurities, and necessity of sterilization before use. For these reasons, many investigators have been trying to search for new agents for pleurodesis. Byun et al. studied effectiveness of taurolidine, and proposed it is an efficacious alternative agent for the management of PAL (20). Godazandeh et al. suggested that iodopovidone is an effective, inexpensive, safe material for chemical pleurodesis in the treatment of malignant pleural effusion and intractable pneumothorax (21). Meanwhile, these diverse challenging agents revealed different success rates of pleurodesis, respectively. In an extensive review of the English language literature from 1966 to 1994 that included 1,168 patients participating in observational studies, the rate of complete success with talc was 93%, compared with 76% for corynebacterium parvum, 67% for tetracycline, 72% for doxycycline and 54% for bleomycin (22). Similarly, talc was completely or partially effective in 659 patients (91%) among 723 patients in 32 serial cases of predominantly malignant effusions (22). However, the efficacy of talc has inconsistently varied from 71% to 100% in randomized controlled attempts of talc slurry compared with other agents for chemical pleurodesis in patients with malignant pleural effusions (23). In other systematic review, the rate of complete success with iodopovidone was 88.5% in patients with pleural effusions and 93.5% in patients with pneumothorax (24). With regard to taurolidine as chemical pleurodesis agent, overall success rate at first infusion was 54.7%.
As for the present study, Abnobaviscum F® is an extract of viscum album (European mistletoe) which grows on trees of the genus fraxinus. This extract substance is the most frequently prescribed drug for complementary treatment in cancer patients in several European countries. It is known to stimulate the immune system, improve survival, enhance equality of life, and decrease the side effects of chemotherapy and radiotherapy (25). Meanwhile, a number of documents have showed favorable outcomes after its use for chemical pleurodesis in the management of malignant pleural effusion (26). Stumpf et al. reported on a successful treatment of malignant pleural effusion in 72% of patients with an intrapleural administration of viscum album (fraxini), while side effect of mild fever developed in 1.2% of patients (27). Likewise, these relevant studies do not report any serious complications, only slight side effects such as mild febrile sensation, trivial burning, and minimal loculated effusion. On the other hand, there have been few reports related to its effectiveness in the management of PAL. Accordingly, this study was aimed at the analysis of clinical efficacy and safety of pleurodesis using viscum album (fraxini) in patients with intractable prolonged air leakage. The research findings validated the evidence of high success rate and low recurrence rate without major complications. However, this study was a retrospective observation report. For the avoidance of selection bias, a large prospective randomized trial should be performed to confirm our findings. We believe that a treatment strategy with viscum album extract for chemical pleurodesis can be feasible after further variable and intensified studies.
Conclusions
In conclusion, Abnobaviscum F® (viscum album extract, fraxini) preparation is an efficacious and well-tolerated sclerosing agent, and chemical pleurodesis using viscum album could be considered as a suitable option for the treatment of prolonged air leak patients, associated with acceptable side effects.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The study was approved by Institutional Review Board of Konkuk University Medical Center (No. 1080025). Surgical and procedural consent was naturally obtained from all patients.
References
- Abolhoda A, Liu D, Brooks A, et al. Prolonged air leak following radical upper lobectomy: an analysis of incidence and possible risk factors. Chest 1998;113:1507-10. [Crossref] [PubMed]
- Macchiarini P, Wain J, Almy S, et al. Experimental and clinical evaluation of a new synthetic, absorbable sealant to reduce air leaks in thoracic operations. J Thorac Cardiovasc Surg 1999;117:751-8. [Crossref] [PubMed]
- Okur E, Kir A, Halezeroglu S, et al. Pleural tenting following upper lobectomies or bilobectomies of the lung to prevent residual air space and prolonged air leak. Eur J Cardiothorac Surg 2001;20:1012-5. [Crossref] [PubMed]
- Brunelli A, Sabbatini A, Xiume' F, et al. Alternate suction reduces prolonged air leak after pulomonary lobectomy: A randomized comparison versus water seal. Ann Thorac Surg 2005;80:1052-5. [Crossref] [PubMed]
- Stefani A, Natali P, Casali C, et al. Talc poudrage versus talc slurry in the treatment of malignant pleural effusion. A prospective comparative study. Eur J Cardiothorac Surg. 2006;30:827-32. [Crossref] [PubMed]
- Agarwal R, Aggarwal AN, Gupta D. Efficacy and safety of iodopovidone pleurodesis through tube thoracostomy. Respirology 2006;11:105-8. [Crossref] [PubMed]
- Rinaldi S, Felton T, Bentley A. Blood pleurodesis for the medical management of pneumothorax. Thorax 2009;64:258-60. [Crossref] [PubMed]
- Yokomise H, Satoh K, Ohno N, et al. Autoblood plus OK432 pleurodesis with open drainage for persistent air leak after lobectomy. Ann Thorac Surg 1998;65:563-5. [Crossref] [PubMed]
- Antunes G, Neville E, Duffy J. BTS guidelines for the management of malignant pleural effusions. Thorax 2003;58 Suppl 2:ii29-38. [Crossref] [PubMed]
- Kienle GS, Kiene H. Review article: influence of Viscum album L (European mistletoe) extracts on quality of life in cancer patients: a systematic review of controlled clinical studies. Integr Cancer Ther 2010;9:142-57. [Crossref] [PubMed]
- Okereke I, Murthy SC, Alster JM, et al. Characterization and importance of air leak after lobectomy. Ann Thorac Surg 2005;79:1167-73. [Crossref] [PubMed]
- Varela G, Jiménez MF, Novoa N, et al. Estimating hospital costs attributable to prolonged air leak in pulmonary lobectomy. Eur J Cardiothorac Surg 2005;27:329-33. [Crossref] [PubMed]
- Irshad K, Feldman LS, Chu VF, et al. Causes of increased length of hospitalization on a general thoracic surgery service: a prospective observational study. Can J Surg 2002;45:264-8. [PubMed]
- Brunelli A, Monteverde M, Borri A, et al. Predictors of prolonged air leak after pulmonary lobectomy. Ann Thorac Surg 2004;77:1205-10; discussion 1210. [Crossref] [PubMed]
- Brunelli A, Xiume F, Al Refai M. Air leaks after lobectomy increase risk of empyema but not cardiopulmonary complications: a case-matched analysis. Chest 2006;130:1150-6. [Crossref] [PubMed]
- Cerfolio RJ, Tummala RP, Holman WL, et al. A prospective algorithm for the management of air leaks after pulmonary resection. Ann Thorac Surg 1998;66:1726-31. [Crossref] [PubMed]
- Brant A, Eaton T. Serious complications with talc slurry pleurodesis. Respirology 2001;6:181-5. [Crossref] [PubMed]
- Rehse DH, Aye RW, Florence MG. Respiratory failure following talc pleurodesis. Am J Surg 1999;177:437-40. [Crossref] [PubMed]
- Bouchama A, Chastre J, Gaudichet A, et al. Acute pneumonitis with bilateral pleural effusion after talc pleurodesis. Chest 1984;86:795-7. [Crossref] [PubMed]
- Byun CS, Park IK, Shim HS, et al. Taurolidine: a new alternative agent for the management of the postoperative air leak. Ann Thorac Cardiovasc Surg 2013;19:6-11. [Crossref] [PubMed]
- Godazandeh G, Qasemi NH, Saghafi M, et al. Pleurodesis with povidone-iodine, as an effective procedure in management of patients with malignant pleural effusion. J Thorac Dis 2013;5:141-4. [PubMed]
- Kennedy L, Sahn SA. Talc pleurodesis for the treatment of pneumothorax and pleural effusion. Chest 1994;106:1215-22. [Crossref] [PubMed]
- Ong KC, Indumathi V, Raghuram J, et al. A comparative study of pleurodesis using talc slurry and bleomycin in the management of malignant pleural effusions. Respirology 2000;5:99-103. [Crossref] [PubMed]
- Agarwal R, Aggarwal AN, Gupta D. Efficacy and safety of iodopovidone in chemical pleurodesis: a meta-analysis of observational studies. Respir Med 2006;100:2043-7. [Crossref] [PubMed]
- Bock PR, Friedel WE, Hanisch J, et al. Efficacy and safety of long-term complementary treatment with standardized European mistletoe extract (Viscum album L.) in addition to the conventional adjuvant oncologic therapy in patients with primary non-metastasized mammary carcinoma. Results of a multi-center, comparative, epidemiological cohort study in Germany and Switzerland. Arzneimittelforschung 2004;54:456-66. [PubMed]
- Salzer G. The local treatment of malignant pleural exudations with Iscador (a drug obtained from Misteltoe). Preliminary report (author's transl). Osterr Z Onkol 1977;4:13-4. [PubMed]
- Stumpf C, Btumpf A. Stimulation of antitumour immunity by intrapleural instillation of a Viscum album L. extract. Anticancer Drugs 1997;8 Suppl 1:S23-6. [Crossref] [PubMed]


