Enhanced recovery pathways in thoracic surgery: the Shanghai experience
Introduction
Despite the significant recent advances in thoracic surgery and rapid transition from the era of traditional surgeries (open thoracotomy) to the era of minimally invasive surgery, R0 resection with lymph node dissection is still the optimal treatment for a patient with operable NSCLC (1,2). Lobectomy remains a major procedure and could be associated with a major morbidity and even mortality (3). Hence the importance of having a perioperative program based on multiple specialties to minimize errors and complications in addition to speeding up the patient’s treatment and recovery as much as possible. Perhaps the first attempts to implement the enhanced recovery (ER) program were in the early 1990s by Henrik Kehlet (4). Since then, an emphasis has been placed on this subject, given its importance and vitality. In the field of thoracic surgery, the main focus was on relieving patient’s pain by providing the minimally invasive surgical techniques and development of therapeutic protocols controlling pain after surgery (5,6). The patient should be involved in this program since his first visit to the clinic until the day he left the hospital after undergoing the operation. The most important preoperative elements of this program are thoroughly medical advice, preparing the patient in terms of feeding optimization and smoking mitigation so that the patient in the most appropriate conditions for the surgery before being admitted to the hospital. During and after the surgery, standard anesthetic and analgesic protocols, early mobilization, and fast-tracking chest drain management are the most important factors (7,8). In China mainland, because there is no unified hospital system and there are large differences between hospitals’ results and protocols, there is no accurate information on the average length of hospital stay after undergoing a pulmonary resection. The patient length of stay rate at the Shanghai Pulmonary Hospital (very high-volume referral hospital) is 7 days and may be considered a very good result compared to international rates (9-11). Perhaps thanks to these results may be due to our belief in the importance of minimally invasive approaches, and their positive effects on the patients and conduct as routinely as possible, in addition to starting to build our ER protocols.
Preoperative outfit
ER depends on the patient is as good as the possible surgical condition. The goal of the patient’s visit to the clinic is to give advice to him and give him some orientation in addition to starting work to review the state of health carefully and address the difficulties that may affect the journey of surgical treatment so that the patient can leave the hospital as soon as possible and with the best possible results. At this stage, the most important elements to pay attention to and approach are malnutrition, reducing smoking, treating anemia, and increasing physical activity, in addition to the importance of controlling blood pressure and diabetes. Patients suffering from chronic obstructive pulmonary disease (COPD) are treated by a pulmonologist so that they are given the ideal treatment of inhalers and bronchodilators; so that the lungs function in the best possible condition before the operation.
A nutritionist is consulted regarding patients with malnutrition and provides them with a diet advice appropriate to the patient’s condition. The nutritionist follows the patient while in the hospital after the operation to follow up his condition and make sure that his nutritional status is well.
Although the period required to reap the benefit of stopping smoking prior to the operation of a pulmonary resection is unknown (12), the patient is asked not to smoke for at least 2 weeks before surgery. In cases of anemia (Hb less than 11 g/dL), the patient is referred to his or her physician to investigate the cause and correct the anemia before the procedure. In addition to its beneficial effects such as strengthening the patient’s muscles and reducing the psychological pressure, physical exercise may improve aerobic capacity and quality of life, and advised at all stages of treatment (13). We ask the patient to exercise as much as possible before the operation, at least climb the stairs several times a day and breathing exercises. From an anesthesia point of view, the anesthesiologist examines and evaluates patients with high risk of undergoing a pulmonary operation in the so-called initial preoperative assessment. The anesthesiologist identifies the circumstances that may lead to complications during and after the operation, the risk factors that can be adjusted preoperatively are directed and managed. In addition, the final preoperative assessment performed just before the operation (before the patient goes to the operating room). At this time, it is paramount to review the data from the initial evaluation and the results of the ordered tests before. There are two other determinants affecting the thoracic anesthesia: the difficult isolation of the lungs and the risk of saturation during lung ventilation (14).
Intraoperative management
When we discuss the ER system we must mention the advanced surgical techniques that are integral to this program. In our department, we believe in the importance of minimally invasive surgeries for the treatment of lung, mediastinal and chest wall pathologies because of its benefits in reducing pain and hurrying the recovery process after surgery significantly, in addition to reducing the complications after the operation (15-17). In recent years, the most advanced minimally invasive techniques have been adopted by most of the surgeons in our academy. More than 90% of the operations are performed by the VATS and most (even complex ones) are performed by intercostal, subxiphoid and subcostal uniportal VATS approaches (18-20). In addition to excellent results, these techniques have helped us to shorten the time and effort in pain management during and after the operation. Wherein we stopped using the epidural or paravertebral block during the surgery except in rare cases. And for the treatment of pain, we mainly rely on giving light intravenous (IV) or oral analgesics, this also of great benefit to further reduction of the rate of complications and accelerate the mobilization of the patient after surgery. Although restricted fluid administrations is required in some cases [e.g., post-pneumonectomy, congestive heart failure (CHF)], Acknowledgement of the importance of good hydration before surgery and its effect in facilitating fluid handling during the operation and minimizing the post-operative complications, we ask the patient to abstain from eating for 6 hours and from drinking for only 2 hours before entering the operating room. Ordinary patients are given 60–100 mL fluids per hour as a maintenance dose for 24 hours after the surgery. Prophylactic antibiotics are given within 30 minutes before the incision, and discontinued in the day after the surgery if there is no risk or evidence for infection. Premedications are not given prior to the operation in order to ensure the movement of the patient for as long as possible (until arrival to the door of the operating room). Venous access applied in the external jugular vein or peripherally and usually removed 1 day after the operation. Central venous pressure (CVP) lines are utilized only in specific cases when inotropic support or parental nutrition is anticipated. Urinary catheter applied in patients who are undergoing major surgeries and usually removed 1 day after the surgery if there are no obstacles.
Postoperative management
Controlling pain after thoracic surgery is a paramount factor for successful expeditious recovery, pain prevention, therefore, means preventing many complications after surgery. As mentioned earlier, the use of modern techniques in minimally invasive surgeries has enabled us to reduce the amount and doses of pain medications, in addition to significantly reducing the dependence on epidural and regional analgesia. Since there is an obvious difference in the level of pain between patients who undergoes thoracotomy compared to VATS patients, we have therefore implemented a protocol specific to each type of patients as shown in the table (Table 1). The patient is given his permanent medications after 48 hours of operation unless there is a health condition preventing this. We encourage the patient to move as soon as possible after surgery. Few hours after the operation, the surgeons or nurses instruct the patient to move, to cough productively and how to use the spirometer or blow balloon. On the first day after surgery, doctor in charge visits the patient twice, then once a day or as needed. In most cases, we use only one chest drain. This leads to less pain after surgery and therefore less use of analgesics (21). The suction is not routinely used unless there is a need for it (a clinically important postoperative space), as this may help quicker removal of the tube and thus speed the patient out of the hospital (22-24). The use of the digital portable suction device is still uncommon in our department, but we are seeking to introduce this technology to serve our patients because of its benefits in promoting the postoperative mobilization of the patients, and facilitate decision-making to remove the chest drains without delay (25). The tube is removed when air leakage stops; the lung is expanded, and when the amount of fluid is less than 200 milliliters per day, provided that the fluid is not blood or chyle. Otherwise, the patient will discharge home with a chest drain in place (26,27). The discharge date and post-discharge arrangements should be verified and strengthened with the patient and his family on a daily basis. Acceptable status for the patient to be discharged from the hospital after making sure that his laboratory tests are fine is that there is no high temperature, moving freely without oxygen supplementation, able to expectorate without difficulties. In our department, the presence of the chest drain does not influence the time of discharge from the hospital unless it is suction dependent. The patient is provided with all the necessary instructions and how to act in the event of any complications expected after the process and is encouraged to communicate with the department if he has any queries.
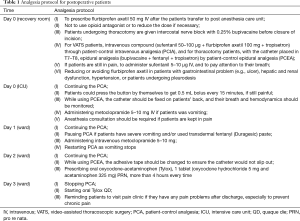
Full table
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Scott WJ, Howington J, Feigenberg S, et al. Treatment of non-small cell lung cancer stage I and stage II:ACCP evidence-based clinical practice guidelines (2nd edition). Chest 2007;132:234S-242S.
- Goldstraw P, Crowley J, Chansky K, et al. The IASLC Lung Cancer Staging Project: proposals for the revision of the TNM stage groupings in the forthcoming (seventh) edition of the TNM Classification of malignant tumours. J Thorac Oncol 2007;2:706-14. [Crossref] [PubMed]
- Burt BM, Kosinski AS, Shrager JB, et al. Thoracoscopic lobectomy is associated with acceptable morbidity and mortality in patients with predicted postoperative forced expiratory volume in 1 second or diffusing capacity for carbon monoxide less than 40% of normal. J Thorac Cardiovasc Surg 2014;148:19-28, dicussion 28-29.e1.
- Kehlet H. Multimodal approach to control postoperative pathophysiology and rehabilitation. Br J Anaesth 1997;78:606-17. [Crossref] [PubMed]
- Tovar EA, Roethe RA, Weissig MD, et al. One-day admission for lung lobectomy: an incidental result of a clinical pathway. Ann Thorac Surg 1998;65:803-6. [Crossref] [PubMed]
- Scarci M, Solli P, Bedetti B. Enhanced recovery pathway for thoracic surgery in the UK. J Thorac Dis 2016;8:S78-83. [PubMed]
- Cerfolio RJ, Pickens A, Bass C, et al. Fast-tracking pulmonary resections. J Thorac Cardiovasc Surg 2001;122:318-24. [Crossref] [PubMed]
- Kehlet H, Wilmore DW. Evidence-based surgical care and the evolution of fast-track surgery. Ann Surg 2008;248:189-98. [Crossref] [PubMed]
- Bach PB, Cramer LD, Schrag D, et al. The influence of hospital volume on survival after resection for lung cancer. N Engl J Med 2001;345:181-8. [Crossref] [PubMed]
- Memtsoudis SG, Besculides MC, Zellos L, et al. Trends in lung surgery: United States 1988 to 2002. Chest 2006;130:1462-70. [Crossref] [PubMed]
- Boffa DJ, Allen MS, Grab JD, et al. Data from The Society of Thoracic Surgeons General Thoracic Surgery database: the surgical management of primary lung tumors. J Thorac Cardiovasc Surg 2008;135:247-54. [Crossref] [PubMed]
- Mason DP, Subramanian S, Nowicki ER, et al. Impact of smoking cessation before resection of lung cancer: a Society of Thoracic Surgeons General Thoracic Surgery Database study. Ann Thorac Surg 2009;88:362-70; discussion 370-1. [Crossref] [PubMed]
- Pouwels S, Fiddelaers J, Teijink JA, et al. Preoperative exercise therapy in lung surgery patients: A systematic review. Respir Med 2015;109:1495-504. [Crossref] [PubMed]
- Kempainen RR, Benditt JO. Evaluation and management of patients with pulmonary disease before thoracic and cardiovascular surgery. Semin Thorac Cardiovasc Surg 2001;13:105-15. [Crossref] [PubMed]
- Abu Akar F, Gonzalez-Rivas D, Ismail M, et al. Uniportal video-assisted thoracic surgery: the Middle East experience. J Thorac Dis 2017;9:871-7. [Crossref] [PubMed]
- Jutley RS, Khalil MW, Rocco G. Uniportal vs standard three-port VATS technique for spontaneous pneumothorax: comparison of post-operative pain and residual paraesthesia. Eur J Cardiothorac Surg 2005;28:43-6. [Crossref] [PubMed]
- Cao C, Manganas C, Ang SC, et al. Video-assisted thoracicsurgery versus open thoracotomy for non-small cell lung cancer: a meta-analysisof propensity score-matched patients. Interact Cardiovasc Thorac Surg 2013;16:244-9. [Crossref] [PubMed]
- Abu Akar F, Yang C, Lin L, et al. Intra-pericardial double sleeve uniportal video-assisted thoracoscopic surgery left upper lobectomy. J Vis Surg 2017;3:51. [Crossref] [PubMed]
- Zhao X, Abu Akar F, Song J, et al. Thoracoscopic tracheal resection and reconstruction using two ports approach. J Vis Surg 2017;3:19. [Crossref] [PubMed]
- Gonzalez-Rivas D, Lirio F, Sesma J, et al. Subxiphoid complex uniportal video-assisted major pulmonary resections. J Vis Surg 2017;3:93. [Crossref] [PubMed]
- Dawson AG, Hosmane S. Should you place one or two chest drains inpatients undergoing lobectomy? Interact Cardiovasc Thorac Surg 2010;11:178-81. [Crossref] [PubMed]
- Deng B, Tan QY, Zhao YP, et al. Suction or non-suction to the underwater seal drains following pulmonary operation:meta-analysis of randomised controlled trials. Eur J Cardiothorac Surg 2010;38:210-5. [Crossref] [PubMed]
- Nomori H, Horio H, Suemasu K. Early removal of chest drainage tubes and oxygen support after a lobectomy for lung cancer facilitates earlier recovery of the 6-minute walking distance. Surg Today 2001;31:395-9. [Crossref] [PubMed]
- Marshall MB, Deeb ME, Bleier JI, et al. Suction vs water seal after pulmonary resection: a randomized prospective study. Chest 2002;121:831-5. [Crossref] [PubMed]
- Brunelli A, Salati M, Refai M, et al. Evaluation of a new chest tube removal protocol using digital air leak monitoring after lobectomy: a prospective randomised trial. Eur J Cardiothorac Surg 2010;37:56-60. [Crossref] [PubMed]
- Cerfolio RJ, Bryant AS. Results of a prospective algorithm to remove chest tubes after pulmonary resection with high output. J Thorac Cardiovasc Surg 2008;135:269-73. [Crossref] [PubMed]
- Antanavicius G, Lamb J, Papasavas P, et al. Initial chest tube management after pulmonary resection. Am Surg 2005;71:416-9. [PubMed]


