Consolidative ablative radiotherapy improves outcomes in oligometastatic non-small cell lung cancer: a further step toward new evidence
Lung cancer is associated with the worst cancer-specific survival than any other tumor. Most of the patients with non-small cell lung cancer (NSCLC) are diagnosed in IV Stage or will develop metastatic progression during the course of the disease (1). A paucity of treatments warrant durable survival benefits once the tumor has spread over the lungs, likely due to the aggressive nature and the ability to progress.
Recently, an oligometastatic state of NSCLC has been demonstrated to exist in selected category of patients, who may benefit not only from systemic therapies but also from aggressive local therapies such as stereotactic ablative radiotherapy (SABR) and surgery to the active sites of disease (2). Accordingly, in the eighth edition of the TNM classification of lung cancer the single metastasis in a single distant organ should be included in the M1b group that is distinguished from the M1c category, that include multiple metastatic lesions in single organ or multiple organs (3). The M1b metastatic state therefore may be considered as a more indolent disease and the definitive combined therapy of the primary tumor and the single metastasis could show higher chance to obtain a good control and survival. The oligometastatic patients, so called “long survivors”, usually present with controlled primary tumor, negative lymph node status, low volume metastatic disease and good response to previous therapies. As a matter of fact, promising outcomes in terms of longer progression-free survival (PFS) and overall survival (OS) might not be due to the treatments themselves, but rather to the selection of patients based on favorable inclusion criteria. Although this favorable subgroup of metastatic patients often present heterogeneities (primary tumor histology, molecular characteristics, site of metastatic spread, number and locations of the metastases, involved organs, and applied therapies), good outcome and tolerance has been described in a meta-analysis by Ashworth et al. (4) showing a median OS of 26 months (5-year 29.4%) in those treated with surgery, SABR or standard radiotherapy to the primary tumor (83.9%) and metastases (62.3%).
According to the present evidence, failure after first-line systemic therapy is more likely to occur at the baseline sites of disease rather than new metastatic sites. SABR has an increased role in the setting of slowly progressive limited metastatic NSCLC and these patients could benefit from such local aggressive therapy without significant toxicities. Unfortunately, most of the present data are reported in form of monoinstitutional retrospective experience and small series of patients (5). In several studies, the oligometastatic state was analyzed separately and divided for the involved organs such as liver, lung, brain, adrenal glands rather than having explored the problematic entity of the metastatic NSCLC (6). In this way, no robust evidence has been built for the oligometastatic/oligorecurrent NSCLC itself, even though a rational in the clinical practice has been further developed. The most relevant prospective and randomized studies in this field are summarized in Table 1 (7-11).
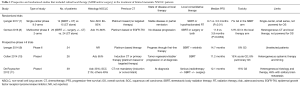
Full table
Over the last years, the development of more safe and effective maintenance chemotherapy combined with technological advances in SABR have improved the options available to such patients. The combination of radiation therapy (RT) with chemotherapy in patients with oligometastatic NSCLC has already shown to dramatically boost disease progression compared to those who received chemotherapy alone, according to a randomized trial by Gomez et al. (8). In the recently published study by Iyengar et al. (7) PFS increased from 3.5 to 9.7 months when RT was delivered to both metastatic sites and the primary tumor site, while treatment-related toxicity was similar for the two treatments. The study was a randomized phase II trial seeking whether the incorporation of consolidative RT to the established systemic therapy improved PFS for patients with oligometastatic NSCLC. Eligible patients were those diagnosed with advanced NCSCL with ≤6 metastatic sites (including the primary disease site) obtaining a stable disease/partial response to 4–6 cycles of first-line/induction platinum-based chemotherapy. They were randomly assigned to receive maintenance chemotherapy alone (control arm) or the same systemic schedule preceded by the addition of SABR to all metastatic sites (experimental arm). RT to metastases consisted of biologically equivalent regimens of single fraction (21–27 Gy), three fractions (26.5–33 Gy) or five fractions (30–37.5 Gy) of SABR. RT to the primary tumor was delivered to a total dose of 45 Gy via SABR if possible, or by means of 15 fractions of hypofractionated RT if the primary tumor involved a central site. The choice of maintenance chemotherapy was left to the discretion of the treating physicians and consisted of pemetrexed, docetaxel, erlotinib or gemcitabine. Between April 2014 and July 2016, 29 patients (69% males) were enrolled. The median age was 70 years (range, 51–79 years) in the control arm and 63.5 years (range, 51–78 years) in the experimental arm. Non-squamous histology was the most common tumor presentation (86% of all patients). The median follow-up was 9.6 months (range, 2.4–30.2 months). Patients’ accrual was stopped when an unplanned interim analysis showed a median PFS rate of 9.7 months in the experimental arm versus 3.5 months in the control arm (P=0.01; hazard ratio =0.304, 95% CI, 0.113–0.815). Specifically, in the consolidative RT followed by chemotherapy group, there were no recurrences in the original sites of gross disease versus seven failures in the maintenance chemotherapy-only group. At the time of analysis, 10 out of the 15 patients in the control arm had progressed, compared with four of the 14 patients in the experimental arm. Overall, treatment-related toxicity was similar between the two groups. No grade 5 toxic effects were reported. There were 2 instances of grade 3 toxic effects and 1 case of grade 4 toxic effects on the maintenance-only arm, while one grade 4 toxicity in the SABR plus maintenance chemotherapy arm was observed.
Some valuable arguments can be gleaned from these data: both of these randomized trials use the response to first-line chemotherapy to select the favorable candidates who have an indolent disease growth. Unlike the other trial from Gomez et al. (8) however, in the commented study patients receiving first-line targeted therapy for EGFR positive and/or ALK-positive NSCLC were excluded, thus representing a broader population of oligometastatic NSCLC. Moreover, in the study by Iyengar et al. (7) only RT was considered for the consolidative treatment of good-responders, whereas Gomez et al. (8) used also the surgery option, which should be considered a viable strategy only for very selected patients due to presence of comorbid conditions and patients preferences. In both of them the PFS was similar in the experimental arms (11.9 and 9.7 months, respectively), and was substantially longer than in the control groups, thus supporting an aggressive approach in this setting. Interestingly, in both of the trials the addition of local consolidative therapy delayed the metastatic spread of new lesions, suggesting that the benefit of treatment intensification could extend beyond known sites of disease. This breakdown in the natural history of disease might be attributed to the optimal tolerability of consolidative radiation, which has allowed patients to keep on going to additional systemic therapy, or to the activation of systemic anticancer immune responses. Both of these circumstances might have facilitated the control of the underlying subclinical disease.
In conclusion, local therapy in the form of consolidative radiation is well positioned to become an important procedure for the management of limited metastatic NSCLC patients. While encouraging findings have shown a dramatic increase in PFS when adding local radiotherapy to maintenance chemotherapy, no impact on OS could be demonstrated because the study was not enough powered for this endpoint. This approach should be tested in larger, randomized phase III trials to confirm whether an increase in PFS may also translate in a significant prolongation of the OS, and to clarify which subgroups of patients are most likely to benefit. Ongoing NRG LU 002 and SARON trials will provide insightful data to address this issue.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Aupérin A, Le Péchoux C, Rolland E, et al. Meta-analysis of concomitant versus sequential radiochemotherapy in locally advanced non-small-cell lung cancer. J Clin Oncol 2010;28:2181-90. [Crossref] [PubMed]
- Ashworth A, Rodrigues G, Boldt G, et al. Is there an oligometastatic state in non-small cell lung cancer? A systematic review of the literature. Lung Cancer 2013;82:197-203. [Crossref] [PubMed]
- Eberhardt WE, Mitchell A, Crowley J, et al. The IASLC lung cancer staging project: proposal for the revisions of the M descriptors in the forthcoming eighth edition of the TNM classification of lung cancer. J Thorac Oncol 2015;10:1515-22.
- Ashworth AB, Senan S, Palma DA, et al. An individual patient data meta-analysis of outcomes and prognostic factors after treatment of oligometastatic non-small-cell lung cancer. Clin Lung Cancer 2014;15:346-55. [Crossref] [PubMed]
- Agolli L, Valeriani M, Nicosia L, et al. Stereotactic ablative body radiotherapy (SABR) in pulmonary oligometastatic/oligorecurrent non-small cell lung cancer patients: a new therapeutic approach. Anticancer Res 2015;35:6239-45. [PubMed]
- Juan O, Popat S. Ablative Therapy for oligometastatic non-small cell lung cancer. Clin Lung Cancer 2017;18:595-606. [Crossref] [PubMed]
- Iyengar P, Wardak Z, Gerber DE, et al. Consolidative radiotherapy for limited metastatic non-small-cell lung cancer: a phase 2 randomized clinical trial. JAMA Oncol 2018;4:e173501. [Crossref] [PubMed]
- Gomez DR, Blumenschein GR Jr, Lee JJ, et al. Local consolidative therapy versus maintenance therapy or observation for patients with oligometastatic non-small-cell lung cancer without progression after first-line systemic therapy: a multicentre, randomised, controlled, phase 2 study. Lancet Oncol 2016;17:1672-82. [Crossref] [PubMed]
- Iyengar P, Kavanagh BD, Wardak Z, et al. Phase II trial of stereotactic body radiation therapy combined with erlotinib for patients with limited but progressive metastatic non-small-cell lung cancer. J Clin Oncol 2014;32:3824-30. [Crossref] [PubMed]
- Collen C, Christian N, Schallier D, et al. Phase II study of stereotactic body radiotherapy to primary tumor and metastatic locations in oligometastatic non small-cell lung cancer patients. Ann Oncol 2014;25:1954-9. [Crossref] [PubMed]
- De Ruysscher D, Wanders R, van Baardwijk A, et al. Radical treatment of non-small-cell lung cancer patients with synchronous oligometastases: long-term results of a prospective phase II trial. J Thorac Oncol 2012;7:1547-55. [Crossref] [PubMed]


