Oncogene-addicted non-small cell lung cancer and immunotherapy
Introduction
The identification of molecular aberrations in key components of signal transduction pathways leading to tumor growth and survival, so called oncogene-addicted tumors, has dramatically changed the treatment landscape of non-small cell lung cancer (NSCLC). Mutations in the epidermal growth factor receptor (EGFR) and anaplastic lymphoma kinase (ALK) rearrangements are so far the most frequent and clinically important targets. A new class of therapeutic agents, tyrosine kinase inhibitors (TKIs), that inhibit the enzymatic activity of these oncogenic drivers has become a concept where the receptor TKIs for EGFR and ALK have been in focus for treatment of NSCLC (1-18). EGFR TKIs gefitinib, erlotinib, afatinib and osimertinib, and the ALK inhibitors crizotinib, ceritinib, and alectinib have been approved in Europe and the United States for the treatment of advanced NSCLC. Through the genome sequencing projects of lung cancer (19,20), we have learnt that a majority of NSCLC, especially adenocarcinomas, harbour at least one driver mutation that can potentially be a target for therapy and this has opened up for many new targeted therapies being studied in clinical trials. The clinical benefit of these targeted therapies is often large with sometimes dramatic responses and improved quality-of-life for the patients. Objective response rates (ORR) of 60–70% are reported with these different TKIs and a disease control rate [DCR; ORR + stable disease (SD)], also including SD, of up to 80–90%. Quite often the same oncogenes are found to be drivers for tumor growth in different kinds of tumors, one example being BRAF mutations that have been identified as an oncogenic event both in malignant melanomas and in a smaller fraction of lung adenocarcinomas (around 1–2%). Other examples for NSCLC include aberrations in HER2, MET, PIK3CA, ROS1, RET, AKT, DDR2, and KRAS. Most recently, targeted therapies for ROS1 and BRAF have been approved for the treatment of advanced NSCLC. Furthermore, new generations of EGFR and ALK TKIs have been developed, some of them also being active in treatment-refractory tumors where acquired resistance to first-generation TKIs has developed. The development in the field is rapid and an increasing number of targeted therapies can be expected to be approved for the treatment of advanced NSCLC in the coming years.
Another paradigm shift in the treatment of NSCLC, as well as numerous other tumor types, has been the introduction of immunotherapy (IO) with immune checkpoint inhibitors targeting programmed cell death-1 (PD-1) or its ligand PD-L1, that has shown a clear clinical benefit with increased overall survival (OS) versus standard chemotherapy, both in the second-line setting and as first-line treatment in selected patients (21-25). A predictive biomarker, protein expression of PD-L1, is now being used in clinical routine to enrich for patients with a higher likelihood of responding to PD-1/PD-L1 inhibitors. Considering the complexity of the immune system and the observation that a substantial fraction of patients treated with immune checkpoint inhibitors do not derive a clinical benefit has been the driving force for further studies on other potential predictive biomarkers for checkpoint inhibition besides PD-L1. PD-1/PD-L1 inhibitors approved so far for the treatment of NSCLC include nivolumab, pembrolizumab and atezolizumab. Inhibitors of another immune checkpoint, CTLA-4, are being studied in lung cancer and one of them, ipilimumab, has already gained approval for the treatment of malignant melanoma. In order to increase the clinical benefit of IO different combination treatments are being studied, including combined treatment with IO and chemotherapy and even combinations with anti-CTLA-4 and anti-PD-1/PD-L1 antibodies that are currently being tested in phase 3 trials with promising results so far in phases 1 and 2 trials (26,27).
IO has revolutionized treatment of advanced NSCLC for patients without oncogenic-driven tumors. However, in tumors with clinically actionable mutations, no clear evidence exists on the correct use of IO. Most clinical data come from subgroup analyses with low number of patients in larger randomized trials, and these data do not support the use of IO after TKI in this category of NSCLC patients. If IO is more beneficial in the first-line setting or in combination with TKIs is still a major clinical issue which has not yet been addressed in large clinical trials.
The purpose of this review is to summarize the existing evidence about the use of IO in oncogenic-addicted tumors and highlight the issues that should be addressed in the future in order to optimize the treatment of these tumors.
IO in EGFR-mutated tumors
EGFR-mutations affect mainly the binding sites of EGFR TKIs and are detected in exons 18-21 of the encoding tyrosine kinase gene (28-30). These mutations are almost exclusively found in lung adenocarcinoma, with more than 85% of cases comprising of exon 19 deletions or the L858R point mutation in exon 21, both of which are clinically actionable targets (28,30,31). EGFR-mutations are found in 10–20% of Caucasians and in 30–50% of Asians with lung adenocarcinoma, with higher prevalence in never smokers and women (29,32).
First-generation EGFR TKIs, erlotinib and gefitinib, second-generation afatinib and third-generation osimertinib, have been approved for the treatment of EGFR-mutated NSCLC in the first and later lines, and osimertinib even in the second-line setting for tumors which develop resistance to first-line TKIs through the EGFR T790M mutation (1-11).
Several immune checkpoint inhibitors targeting PD-1 or PD-L1 have shown robust clinical efficacy in advanced NSCLC in the second-line setting. Pembrolizumab, a PD-1 inhibitor, has recently been approved in the first-line setting, in patients with high PD-L1 expression (≥50%) (25), and has shown promising activity in combination with chemotherapy with a clear progression-free survival (PFS) benefit over platinum-based chemotherapy, in a randomized phase 2 trial in treatment-naïve patients irrespective of PD-L1 expression (26). In both of these trials with pembrolizumab, no patients with activating EGFR-mutation or ALK-rearrangement were included.
In the second-line setting, nivolumab, a PD-1 inhibitor, has been approved for the treatment of squamous and non-squamous NSCLC (21,22). In the trial for non-squamous NSCLC, EGFR-mutated patients did not derive any survival benefit from nivolumab with a HR 1.18 (95% CI: 0.69–2.00), compared to the whole study population where nivolumab-treated patients had a better OS with a HR 0.75 (95% CI: 0.2–0.91) (21). In the trial conducted for squamous NSCLC, as expected, there were no patients with EGFR-mutated or ALK-rearranged tumors (22). Pembrolizumab has also shown superior efficacy compared to docetaxel in previously treated PD-L1 positive NSCLC patients with a HR for OS of 0.67 (95% CI: 0.56–0.80). In subgroup analyses, EGFR-mutation positive patients did not derive any statistically significant benefit from IO with a HR of 0.88 (95% CI: 0.45–1.70) (23).
Atezolizumab, a PD-L1 inhibitor, significantly improved OS compared with docetaxel in previously treated NSCLC patients in the phase 2 POPLAR trial (33) and the phase 3 OAK trial (in OAK trial irrespective of PD-L1 expression) (24). In POPLAR, no subgroup analysis for EGFR-mutation positive patients has been published. In OAK, HR for OS was 0.73 (95% CI: 0.62–0.87) in favour of atezolizumab for the whole study population, whereas 1.24 (95% CI: 0.71–2.18) for EGFR-mutation positive patients. Another PD-L1 inhibitor, durvalumab, has shown robust clinical activity with a clear PFS benefit after chemoradiotherapy in stage 3 locally advanced unresectable NSCLC (34). In this trial, the PACIFIC trial, HR for PFS for the whole study population was 0.55 (95% CI: 0.45–0.68) in favour of durvalumab consolidation therapy, whereas for EGFR-mutation positive patients HR was not significant, 0.76 (95% CI: 0.35–1.64).
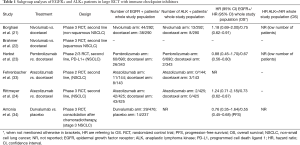
All data from these subgroup analyses from larger randomized phase 3 trials are summarized in Table 1. These data do not support the use of IO in the second-line setting for EGFR-mutation positive tumors, although no safe conclusions can be drawn due to the limited number of patients and the subgroup character of the analyses. Real-world data from the Italian nivolumab expanded access programme (EAP) are in line with those observed in the above-mentioned subgroup analyses. Survival and response rates with nivolumab in the Italian cohort of this EAP were similar to those observed in the nivolumab arm of the CheckMate 057 study (21), whereas survival was reduced in never-smokers with EGFR-mutation positive tumors (35). A recently published meta-analysis came to a similar conclusion (36), demonstrating that immune checkpoint inhibitors compared to docetaxel significantly prolonged OS over that with docetaxel overall (HR 0.68, 95% CI: 0.61–0.77, P<0.0001) and in the EGFR wild-type subgroup (HR 0.66, 95% CI: 0.58–0.76, P<0.0001), but not in the EGFR-mutant subgroup (HR 1.05, 95% CI: 0.70–1.55, P<0.81).
Full table
IO in ALK-rearranged NSCLC
ALK rearrangements, where EML4-ALK is the dominating rearrangement, is found in 3–7% of NSCLC, almost exclusively in younger adenocarcinoma patients with former light or no smoking history (37). Several ALK TKIs, including crizotinib and ceritinib, have shown superior efficacy compared to chemotherapy in the first and subsequent lines of therapy (14-18), and alectinib has shown superior efficacy and lower toxicity compared to crizotinib in the first-line setting (12,13).
Gainor et al. reported a very low ORR in ALK-rearranged or EGFR-mutated NSCLC patients treated with IO, ORR was lower than 5% in 58 IO treated patients (38). As shown in Table 1, in most of the randomized controlled trials with immune checkpoint inhibitors, there were either no patients with ALK-rearrangements included or low numbers which did not permit any meaningful subgroup analysis. In addition, no prospective data exist which address the use of IO in ALK-positive patients, and therefore no conclusions about the use of IO in ALK-positive patients can be drawn at this time point.
IO in other oncogenic-addicted tumors
New data have emerged during the past few years for the treatment of oncogenic-driven NSCLC with novel TKIs. The ROS1 fusion oncogene is detected in 1–2% of lung adenocarcinoma patients (39) for which crizotinib, ceritinib and lorlatinib have shown promising clinical activity in phases 1 and 2 trials, but no data exist regarding the effect of immune checkpoint inhibition in ROS1-positive tumors (17,40-42).
Mitogen-activated protein kinase (MAPK) pathway is commonly activated in tumors of NSCLC and mutated BRAF is an actionable target. A phase 2 trial with the BRAF inhibitor dabrafenib in BRAF-mutated NSCLC (V600E, 1–2% of lung adenocarcinoma patients) has shown modest activity with an ORR of 33% (43). The combination of dabrafenib with the MEK inhibitor trametinib has shown improved clinical activity in both pre-treated and untreated BRAF-mutated patients in two phase 2 trials with an ORR over 60% (44,45). There is so far no clinical data regarding the role of IO in BRAF-mutated lung adenocarcinoma. Preclinical trials from melanoma patients have shown that inhibition of the MAPK pathway enhances host anti-tumor immunity by elevating melanoma antigen expression and improving T-cell infiltration and function (46-52). Combining BRAF TKIs with IO seems to be a reasonable treatment strategy, since the above-mentioned changes may serve to prime the tumor microenvironment for response to immunotherapy. In a phase 1/2 melanoma trial, ipilimumab was combined with dabrafenib, or with dabrafenib and trametinib in a triplet arm. Early report of this trial showed preliminary activity in all patients in the doublet arm (53). No dose-limiting observations were reported in the doublet arm, whereas the triplet combination of dabrafenib + trametinib + ipilimumab was poorly tolerated and was closed due to safety findings.
Other TKIs targeting HER-2 mutations, MET exon 14 splice mutation or amplification, RET translocation, and NTRK translocation are in early clinical trials with variable results (54). The role of IO is unclear for patients bearing these mutations and there are no data regarding combination treatment with TKIs and IO for these actionable targets.
Future directions
The immunogenicity of a tumor and responsiveness to IO is determined by a complex set of immunomodulatory factors present both in the actual tumor cells as well as in cells in the surrounding tumor microenvironment (55). In the pivotal study by Rizvi and colleagues (56), whole exome sequencing was performed in tumors of NSCLC treated with pembrolizumab, and it was observed that higher non-synonymous mutation burden in tumors was associated with improved ORR, durable clinical benefit, and PFS. Efficacy also correlated with a molecular smoking signature, higher neoantigen burden, and DNA repair pathway mutations. These data indicate that the genomic landscape of tumors is critically important in the response to immune checkpoint inhibitors. Tumors of NSCLC are commonly characterized by a high mutational burden, especially those chronically exposed to carcinogens in tobacco smoke, providing a therapeutic rationale for immune checkpoint inhibition. In contrast, oncogene-addicted tumors such as EGFR-mutated, have been shown to have a lower mutation burden, which may explain, at least partly, the decreased efficacy of immunotherapy. This was observed in a study by Dong et al. (57) who demonstrated that EGFR mutated tumors, besides a decreased mutation burden, showed a lack of T-cell infiltration and shrinking proportion of PD-L1+/CD8+ tumor infiltrating lymphocytes (TILs). Patients with these EGFR-mutated tumors did not benefit from PD-1/PD-L1 inhibitors while patients with EGFR wild-type did, providing evidence of a correlation between EGFR mutations and an uninflamed tumor microenvironment with weak immunogenicity.
The most widely used predictive biomarker for checkpoint inhibition, PD-L1, seems to be differentially expressed depending on the molecular phenotype of the tumor. Data from cell lines and mouse models have shown that expression of PD-L1 is driven by EGFR-mutant tumors, and that PD-1 inhibition leads to prolonged survival in EGFR-mutation positive mice (58). Data from retrospective analyses show a strong correlation between high PD-L1 expression and activating EGFR-mutations in NSCLC patients (59). Chen et al. reported that EGFR activation upregulated PD-L1 through p-ERK1/2p-c-Jun, but no synergistic effect was observed with EGFR TKIs and anti-PD-1 antibody combination treatment. This could be related to the fact that immune escape in EGFR-mutant NSCLC is mainly mediated by the upregulation of PD-L1 through EGFR activation, and therefore EGFR TKIs and anti-PD-1 antibody may not have additive immune mediated effects (60). It is unclear if the combination of IO and EGFR TKIs can render a possible treatment option in EGFR-mutation positive NSCLC patients. A phase 1 trial with the combination of erlotinib and nivolumab in 21 patients with EGFR-mutation positive NSCLC showed a promising response rate of 20% and PFS rate at 24 weeks was 47% (61). All patients included in this trial had progressed on prior EGFR TKI, except for one who was TKI naïve, and the toxicity profile was manageable with four patients experiencing grades 3–4 toxicity, including diarrhea, weight loss and elevation of hepatic enzymes, two of these patients discontinued treatment due to toxicity. The combination of osimertinib plus durvalumab was investigated as part of TATTON, a multi-arm phase Ib study. Twenty-three EGFR TKI-pretreated (part A, dose escalation) and 11 EGFR TKI-naive patients (part B, dose expansion) were treated with 80 mg osimertinib plus 3 or 10 mg/kg durvalumab every 2 weeks. ORR was 67% in T790M-positive and 21% in T790M-negative patients who had received prior treatment with EGFR TKI, whereas it was 70% in EGFR TKI-naive patients (62). Unfortunately, this promising combination was associated with a high incidence of interstitial lung disease (ILD) (38% of the whole study population). Five in 13 patients with ILD had grade 3/4 toxicity without any fatal case. ILD was managed with high-dose corticosteroids and discontinuation of drugs, but the incidence considered to be unexpectedly high and therefore a major concern for further development of this treatment strategy. The combination of gefitinib plus durvalumab was investigated in the dose expansion phase of a phase 1b study. In this study, EGFR TKI-naive patients (n=10) were treated with either concurrent durvalumab plus gefitinib (arm 1) or with induction gefitinib monotherapy for 4 weeks followed by concurrent durvalumab plus gefitinib (arm 2) (63). ORR was 77.8% in arm 1 and 80% in arm 2, respectively, but a high incidence of grade 3/4 liver enzyme elevation (40–70%) was observed. Another phase Ib study of atezolizumab combined with erlotinib has shown promising results with an ORR of 75%. Twenty-eight patients were treated with this combination with a manageable toxicity profile. ILD was not observed, but 39% of the whole study population experienced grade 3/4 adverse events, including ALT elevation (7%), pyrexia (7%), and rash (7%). Adverse events leading to atezolizumab discontinuation occurred in 18% of patients (64).
As mentioned above, in the studies with pembrolizumab in the first-line setting, no EGFR-mutation positive patients were included (25,26). The use of immune checkpoint inhibitors in the first-line setting can be a possible treatment strategy for EGFR-mutation positive patients, especially taking into consideration the observation that PD-L1 expression decreases in EGFR-mutant cell lines after exposure to an EGFR-TKI (58).
Regarding ALK-rearranged tumors, there are several trials ongoing with the combination of ALK TKIs and immune checkpoint inhibitors (65) with no published data so far. A higher PD-L1 expression in ALK-rearranged NSCLC cell lines has been reported, which declined after treatment of these cell lines with alectinib (66,67). The use of immune checkpoint inhibition monotherapy in the first-line setting in ALK-positive NSCLC is an interesting concept, which should be addressed in a randomized setting. No other clinically relevant results exist in the literature, which could guide treatment with IO in ALK-rearranged NSCLC patients.
There may be several potential strategies to increase the immunogenicity of oncogene-addicted tumors and hence increase the efficacy of checkpoint inhibitors. One promising approach is to combine radiotherapy with immunotherapy. Radiotherapy targeted to the tumor leads to the release of neoantigens through tumor cell death, which in turn may lead to triggering of the immune system, including activation of tumor-specific T-cells. This may lead to not only a local anti-tumoral effect but also an immune reaction towards all systemic disease, a phenomenon called abscopal effect. The potential benefit of combining radiotherapy with IO is being studied in several clinical trials and has already been demonstrated, for example in the PACIFIC trial mentioned above (34). Other possible strategies to increase the efficacy of IO is to combine with other systemic treatments, one way being to treat with a combination of different immunotherapies. In the CheckMate 012 open-label multicohort phase 1 study (27), two different checkpoint inhibitors, nivolumab and ipilimumab, were given as a first-line combination treatment to patients with advanced NSCLC. Results showed a tolerable safety profile and an encouraging clinical activity characterised by a high response rate (57%) and durable response, indicating an improved benefit over anti-PD-1 monotherapy. Other promising combination strategies that are being studied include immune checkpoint inhibition plus anti-angiogenic therapy as well as combining checkpoint inhibitors with chemotherapy. Future studies will tell how well these combinations can be applied to the treatment of oncogene-addicted NSCLC.
Conclusions
The role of immune checkpoint inhibition for NSCLC with oncogenic-addicted tumors is so far unclear. In EGFR-mutation positive patients there seems to be a worse effect of IO after TKI treatment compared to patients without actionable mutations, though no safe conclusions can be drawn due to the lack of randomized trials addressing this clinical issue. For other oncogenic driver mutations there is no clinical evidence regarding the effect of IO up to date. Preclinical data are also limited but in the case of BRAF, some guidance for future treatment strategies can be derived from melanoma trials. In order to improve treatment decision making for oncogenic-driven NSCLC it is of vital importance to design randomized trials in the future, also in the first-line setting, comparing TKIs to immunotherapy, as well as evaluating different treatment combinations and sequences including immunotherapy.
Acknowledgements
Research by the authors is supported by Stockholm Cancer Society and Stockholm County Council. This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Mok TS, Wu YL, Thongprasert S, et al. Gefitinib or carboplatin-paclitaxel in pulmonary adenocarcinoma. N Engl J Med 2009;361:947-57. [Crossref] [PubMed]
- Rosell R, Carcereny E, Gervais R, et al. Erlotinib versus standard chemotherapy as first-line treatment for European patients with advanced EGFR mutation-positive non-small-cell lung cancer (EURTAC): a multicentre, open-label, randomised phase 3 trial. Lancet Oncol 2012;13:239-46. [Crossref] [PubMed]
- Sequist LV, Yang JC, Yamamoto N, et al. Phase III study of afatinib or cisplatin plus pemetrexed in patients with metastatic lung adenocarcinoma with EGFR mutations. J Clin Oncol 2013;31:3327-34. [Crossref] [PubMed]
- Wu YL, Zhou C, Hu CP, et al. Afatinib versus cisplatin plus gemcitabine for first-line treatment of Asian patients with advanced non-small-cell lung cancer harbouring EGFR mutations (LUX-Lung 6): an open-label, randomised phase 3 trial. Lancet Oncol 2014;15:213-22. [Crossref] [PubMed]
- Zhou C, Wu YL, Chen G, et al. Erlotinib versus chemotherapy as first-line treatment for patients with advanced EGFR mutation-positive non-small-cell lung cancer (OPTIMAL, CTONG-0802): a multicentre, open-label, randomised, phase 3 study. Lancet Oncol 2011;12:735-42. [Crossref] [PubMed]
- Maemondo M, Inoue A, Kobayashi K, et al. Gefitinib or chemotherapy for non-small-cell lung cancer with mutated EGFR. N Engl J Med 2010;362:2380-8. [Crossref] [PubMed]
- Mitsudomi T, Morita S, Yatabe Y, et al. Gefitinib versus cisplatin plus docetaxel in patients with non-small-cell lung cancer harbouring mutations of the epidermal growth factor receptor (WJTOG3405): an open label, randomised phase 3 trial. Lancet Oncol 2010;11:121-8. [Crossref] [PubMed]
- Inoue A, Kobayashi K, Maemondo M, et al. Updated overall survival results from a randomized phase III trial comparing gefitinib with carboplatin-paclitaxel for chemo-naive non-small cell lung cancer with sensitive EGFR gene mutations (NEJ002). Ann Oncol 2013;24:54-9. [Crossref] [PubMed]
- Han JY, Park K, Kim SW, et al. First-SIGNAL: first-line single-agent iressa versus gemcitabine and cisplatin trial in never-smokers with adenocarcinoma of the lung. J Clin Oncol 2012;30:1122-8. [Crossref] [PubMed]
- Mok TS, Wu YL, Ahn MJ, et al. Osimertinib or Platinum-Pemetrexed in EGFR T790M-Positive Lung Cancer. N Engl J Med 2017;376:629-40. [Crossref] [PubMed]
- Soria JC, Ohe Y, Vansteenkiste J, et al. Osimertinib in Untreated EGFR-Mutated Advanced Non-Small-Cell Lung Cancer. N Engl J Med 2018;378:113-25. [Crossref] [PubMed]
- Hida T, Nokihara H, Kondo M, et al. Alectinib versus crizotinib in patients with ALK-positive non-small-cell lung cancer (J-ALEX): an open-label, randomised phase 3 trial. Lancet 2017;390:29-39. [Crossref] [PubMed]
- Peters S, Camidge DR, Shaw AT, et al. Alectinib versus Crizotinib in Untreated ALK-Positive Non-Small-Cell Lung Cancer. N Engl J Med 2017;377:829-38. [Crossref] [PubMed]
- Solomon BJ, Mok T, Kim DW, et al. First-line crizotinib versus chemotherapy in ALK-positive lung cancer. N Engl J Med 2014;371:2167-77. [Crossref] [PubMed]
- Shaw AT, Kim TM, Crino L, et al. Ceritinib versus chemotherapy in patients with ALK-rearranged non-small-cell lung cancer previously given chemotherapy and crizotinib (ASCEND-5): a randomised, controlled, open-label, phase 3 trial. Lancet Oncol 2017;18:874-86. [Crossref] [PubMed]
- Soria JC, Tan DSW, Chiari R, et al. First-line ceritinib versus platinum-based chemotherapy in advanced ALK-rearranged non-small-cell lung cancer (ASCEND-4): a randomised, open-label, phase 3 study. Lancet 2017;389:917-29. [Crossref] [PubMed]
- Shaw AT, Felip E, Bauer TM, et al. Lorlatinib in non-small-cell lung cancer with ALK or ROS1 rearrangement: an international, multicentre, open-label, single-arm first-in-man phase 1 trial. Lancet Oncol 2017;18:1590-9. [Crossref] [PubMed]
- Kim DW, Tiseo M, Ahn MJ, et al. Brigatinib in Patients With Crizotinib-Refractory Anaplastic Lymphoma Kinase-Positive Non-Small-Cell Lung Cancer: A Randomized, Multicenter Phase II Trial. J Clin Oncol 2017;35:2490-8. [Crossref] [PubMed]
- Cancer Genome Atlas Research Network. Comprehensive genomic characterization of squamous cell lung cancers. Nature 2012;489:519-25. [Crossref] [PubMed]
- Imielinski M, Berger AH, Hammerman PS, et al. Mapping the hallmarks of lung adenocarcinoma with massively parallel sequencing. Cell 2012;150:1107-20. [Crossref] [PubMed]
- Borghaei H, Paz-Ares L, Horn L, et al. Nivolumab versus Docetaxel in Advanced Nonsquamous Non-Small-Cell Lung Cancer. N Engl J Med 2015;373:1627-39. [Crossref] [PubMed]
- Brahmer J, Reckamp KL, Baas P, et al. Nivolumab versus Docetaxel in Advanced Squamous-Cell Non-Small-Cell Lung Cancer. N Engl J Med 2015;373:123-35. [Crossref] [PubMed]
- Herbst RS, Baas P, Kim DW, et al. Pembrolizumab versus docetaxel for previously treated, PD-L1-positive, advanced non-small-cell lung cancer (KEYNOTE-010): a randomised controlled trial. Lancet 2016;387:1540-50. [Crossref] [PubMed]
- Rittmeyer A, Barlesi F, Waterkamp D, et al. Atezolizumab versus docetaxel in patients with previously treated non-small-cell lung cancer (OAK): a phase 3, open-label, multicentre randomised controlled trial. Lancet 2017;389:255-65. [Crossref] [PubMed]
- Reck M, Rodriguez-Abreu D, Robinson AG, et al. Pembrolizumab versus Chemotherapy for PD-L1-Positive Non-Small-Cell Lung Cancer. N Engl J Med 2016;375:1823-33. [Crossref] [PubMed]
- Langer CJ, Gadgeel SM, Borghaei H, et al. Carboplatin and pemetrexed with or without pembrolizumab for advanced, non-squamous non-small-cell lung cancer: a randomised, phase 2 cohort of the open-label KEYNOTE-021 study. Lancet Oncol 2016;17:1497-508. [Crossref] [PubMed]
- Hellmann MD, Rizvi NA, Goldman JW, et al. Nivolumab plus ipilimumab as first-line treatment for advanced non-small-cell lung cancer (CheckMate 012): results of an open-label, phase 1, multicohort study. Lancet Oncol 2017;18:31-41. [Crossref] [PubMed]
- Sharma SV, Bell DW, Settleman J, et al. Epidermal growth factor receptor mutations in lung cancer. Nat Rev Cancer 2007;7:169-81. [Crossref] [PubMed]
- Cadranel J, Ruppert AM, Beau-Faller M, et al. Therapeutic strategy for advanced EGFR mutant non-small-cell lung carcinoma. Crit Rev Oncol Hematol 2013;88:477-93. [Crossref] [PubMed]
- Ellison G, Zhu G, Moulis A, et al. EGFR mutation testing in lung cancer: a review of available methods and their use for analysis of tumour tissue and cytology samples. J Clin Pathol 2013;66:79-89. [Crossref] [PubMed]
- Beau-Faller M, Degeorges A, Rolland E, et al. Cross-validation study for epidermal growth factor receptor and KRAS mutation detection in 74 blinded non-small cell lung carcinoma samples: a total of 5550 exons sequenced by 15 molecular French laboratories (evaluation of the EGFR mutation status for the administration of EGFR-TKIs in non-small cell lung carcinoma [ERMETIC] project--part 1). J Thorac Oncol 2011;6:1006-15. [Crossref] [PubMed]
- Hirsch FR, Janne PA, Eberhardt WE, et al. Epidermal growth factor receptor inhibition in lung cancer: status 2012. J Thorac Oncol 2013;8:373-84. [Crossref] [PubMed]
- Fehrenbacher L, Spira A, Ballinger M, et al. Atezolizumab versus docetaxel for patients with previously treated non-small-cell lung cancer (POPLAR): a multicentre, open-label, phase 2 randomised controlled trial. Lancet 2016;387:1837-46. [Crossref] [PubMed]
- Antonia SJ, Villegas A, Daniel D, et al. Durvalumab after Chemoradiotherapy in Stage III Non-Small-Cell Lung Cancer. N Engl J Med 2017;377:1919-29. [Crossref] [PubMed]
- Grossi F, Crinò L, Delmonte A, et al. MA 10.06 Real-World Results in Non-Squamous Non-Small Cell Lung Cancer Patients: Italian Nivolumab Expanded Access Program. J Thorac Oncol 2017;12:S1841. [Crossref]
- Lee CK, Man J, Lord S, et al. Checkpoint Inhibitors in Metastatic EGFR-Mutated Non-Small Cell Lung Cancer-A Meta-Analysis. J Thorac Oncol 2017;12:403-7. [Crossref] [PubMed]
- Soda M, Choi YL, Enomoto M, et al. Identification of the transforming EML4-ALK fusion gene in non-small-cell lung cancer. Nature 2007;448:561-6. [Crossref] [PubMed]
- Gainor JF, Shaw AT, Sequist LV, et al. EGFR Mutations and ALK Rearrangements Are Associated with Low Response Rates to PD-1 Pathway Blockade in Non-Small Cell Lung Cancer: A Retrospective Analysis. Clin Cancer Res 2016;22:4585-93. [Crossref] [PubMed]
- Takeuchi K, Soda M, Togashi Y, et al. RET, ROS1 and ALK fusions in lung cancer. Nat Med 2012;18:378-81. [Crossref] [PubMed]
- Shaw AT, Solomon BJ. Crizotinib in ROS1-rearranged non-small-cell lung cancer. N Engl J Med 2015;372:683-4. [Crossref] [PubMed]
- Mazieres J, Zalcman G, Crino L, et al. Crizotinib therapy for advanced lung adenocarcinoma and a ROS1 rearrangement: results from the EUROS1 cohort. J Clin Oncol 2015;33:992-9. [Crossref] [PubMed]
- Lim SM, Kim HR, Lee JS, et al. Open-Label, Multicenter, Phase II Study of Ceritinib in Patients With Non-Small-Cell Lung Cancer Harboring ROS1 Rearrangement. J Clin Oncol 2017;35:2613-8. [Crossref] [PubMed]
- Planchard D, Kim TM, Mazieres J, et al. Dabrafenib in patients with BRAF(V600E)-positive advanced non-small-cell lung cancer: a single-arm, multicentre, open-label, phase 2 trial. Lancet Oncol 2016;17:642-50. [Crossref] [PubMed]
- Planchard D, Smit EF, Groen HJ, et al. Dabrafenib plus trametinib in patients with previously untreated BRAF(V600E)-mutant metastatic non-small-cell lung cancer: an open-label, phase 2 trial. Lancet Oncol 2017;18:1307-16. [Crossref] [PubMed]
- Planchard D, Besse B, Groen HJ, et al. Dabrafenib plus trametinib in patients with previously treated BRAF(V600E)-mutant metastatic non-small cell lung cancer: an open-label, multicentre phase 2 trial. Lancet Oncol 2016;17:984-93. [Crossref] [PubMed]
- Boni A, Cogdill AP, Dang P, et al. Selective BRAFV600E inhibition enhances T-cell recognition of melanoma without affecting lymphocyte function. Cancer Res 2010;70:5213-9. [Crossref] [PubMed]
- Kono M, Dunn IS, Durda PJ, et al. Role of the mitogen-activated protein kinase signaling pathway in the regulation of human melanocytic antigen expression. Mol Cancer Res 2006;4:779-92. [Crossref] [PubMed]
- Frederick DT, Piris A, Cogdill AP, et al. BRAF inhibition is associated with enhanced melanoma antigen expression and a more favorable tumor microenvironment in patients with metastatic melanoma. Clin Cancer Res 2013;19:1225-31. [Crossref] [PubMed]
- Liu C, Peng W, Xu C, et al. BRAF inhibition increases tumor infiltration by T cells and enhances the antitumor activity of adoptive immunotherapy in mice. Clin Cancer Res 2013;19:393-403. [Crossref] [PubMed]
- Callahan MK, Masters G, Pratilas CA, et al. Paradoxical activation of T cells via augmented ERK signaling mediated by a RAF inhibitor. Cancer Immunol Res 2014;2:70-9. [Crossref] [PubMed]
- Jiang X, Zhou J, Giobbie-Hurder A, et al. The activation of MAPK in melanoma cells resistant to BRAF inhibition promotes PD-L1 expression that is reversible by MEK and PI3K inhibition. Clin Cancer Res 2013;19:598-609. [Crossref] [PubMed]
- Atefi M, Avramis E, Lassen A, et al. Effects of MAPK and PI3K pathways on PD-L1 expression in melanoma. Clin Cancer Res 2014;20:3446-57. [Crossref] [PubMed]
- Puzanov I, Callahan MK, Linette GP, et al. Phase 1 study of the BRAF inhibitor dabrafenib (D) with or without the MEK inhibitor trametinib (T) in combination with ipilimumab (Ipi) for V600E/K mutation–positive unresectable or metastatic melanoma (MM). J Clin Oncol 2014;32:2511.
- Hirsch FR, Suda K, Wiens J, et al. New and emerging targeted treatments in advanced non-small-cell lung cancer. Lancet 2016;388:1012-24. [Crossref] [PubMed]
- Maleki Vareki S, Garrigós C, Duran I. Biomarkers of response to PD-1/PD-L1 inhibition. Crit Rev Oncol Hematol 2017;116:116-24. [Crossref] [PubMed]
- Rizvi NA, Hellmann MD, Snyder A, et al. Cancer immunology. Mutational landscape determines sensitivity to PD-1 blockade in non-small cell lung cancer. Science 2015;348:124-8. [Crossref] [PubMed]
- Dong ZY, Zhang JT, Liu SY, et al. EGFR mutation correlates with uninflamed phenotype and weak immunogenicity, causing impaired response to PD-1 blockade in non-small cell lung cancer. Oncoimmunology 2017;6:e1356145. [Crossref] [PubMed]
- Akbay EA, Koyama S, Carretero J, et al. Activation of the PD-1 pathway contributes to immune escape in EGFR-driven lung tumors. Cancer Discov 2013;3:1355-63. [Crossref] [PubMed]
- D'Incecco A, Andreozzi M, Ludovini V, et al. PD-1 and PD-L1 expression in molecularly selected non-small-cell lung cancer patients. Br J Cancer 2015;112:95-102. [Crossref] [PubMed]
- Chen N, Fang W, Zhan J, et al. Upregulation of PD-L1 by EGFR Activation Mediates the Immune Escape in EGFR-Driven NSCLC: Implication for Optional Immune Targeted Therapy for NSCLC Patients with EGFR Mutation. J Thorac Oncol 2015;10:910-23. [Crossref] [PubMed]
- Rizvi NA, Chow LQ, Borghaei H, et al. Safety and response with nivolumab (anti-PD-1; BMS-936558, ONO-4538) plus erlotinib in patients (pts) with epidermal growth factor receptor mutant (EGFR MT) advanced NSCLC. J Clin Oncol 2014;32:abstr 8022.
- Ahn MJ, Yang J, Yu H, et al. 136O: Osimertinib combined with durvalumab in EGFR-mutant non-small cell lung cancer: Results from the TATTON phase Ib trial. J Thorac Oncol 2016;11:S115. [Crossref] [PubMed]
- Gibbons DL, Chow LQ, Kim DW, et al. 57O Efficacy, safety and tolerability of MEDI4736 (durvalumab [D]), a human IgG1 anti-programmed cell death-ligand-1 (PD-L1) antibody, combined with gefitinib (G): A phase I expansion in TKI-naive patients (pts) with EGFR mutant NSCLC. J Thorac Oncol 2016;11:S79. [Crossref] [PubMed]
- Ma BB, Rudin CM, Cervantes A, et al. 441O - Preliminary safety and clinical activity of erlotinib plus atezolizumab from a Phase Ib study in advanced NSCLC. Ann Oncol 2016;27:ix139-56. [Crossref]
- Bylicki O, Paleiron N, Margery J, et al. Targeting the PD-1/PD-L1 Immune Checkpoint in EGFR-Mutated or ALK-Translocated Non-Small-Cell Lung Cancer. Target Oncol 2017;12:563-9. [Crossref] [PubMed]
- Ota K, Azuma K, Kawahara A, et al. Induction of PD-L1 Expression by the EML4-ALK Oncoprotein and Downstream Signaling Pathways in Non-Small Cell Lung Cancer. Clin Cancer Res 2015;21:4014-21. [Crossref] [PubMed]
- Hong S, Chen N, Fang W, et al. Upregulation of PD-L1 by EML4-ALK fusion protein mediates the immune escape in ALK positive NSCLC: Implication for optional anti-PD-1/PD-L1 immune therapy for ALK-TKIs sensitive and resistant NSCLC patients. Oncoimmunology 2015;5:e1094598. [Crossref] [PubMed]


