Pneumorrhachis: an under-recognized entity correlates with severity of spontaneous pneumomediastinum
Spontaneous pneumomediastinum (SPM) is an uncommon condition that predominantly affects young males. Due to its rarity, the optimal management still remains uncertain without consensus.
We read with great interest the article titled “Clinical Experience of Spontaneous Pneumomediastinum: Diagnosis and Treatment” by Kim et al. (1), who reported one of the largest series of SPM in literature in the last decade (2-6). The authors demonstrate the result of no difference in symptoms, clinical course and SPM, which was conservatively managed regardless of the degree of severity via their proposed radiologic classification.
In the recent 2 years at our institution, a preliminary investigation for SPM was initiated retrospectively based on the authors’ classification. Surprisingly, we found that several cases of severe type of SPM exhibit additional epidural air, which is also known as pneumorrhachis (Figure 1A,B). Spontaneous pneumorrhachis is a rare condition and occasionally correlates with SPM. It is hypothesized to originate from air leak spreading through the posterior mediastinum into the epidural space via the cervical fascia planes or neural foramen (7). Owing to its scarcity in nature, there is no established incidence of pneumorrhachis associated with SPM except for only one published study revealing 4 out of 42 cases (9.5%) of SPM as well as extensive subcutaneous emphysema, suggesting that in SPM, pneumorrhachis is uncommon but not extraordinary (8).
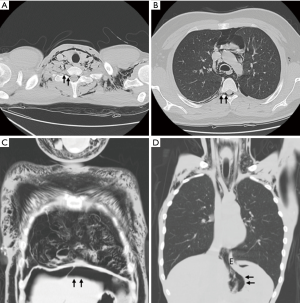
With the continuing advancement in imaging studies and frequent adoption of chest computed tomography in cases of SPM, pneumorrhachis may be increasingly detected. In spite of its benign and self-limiting entity, we would like to reclassify the degree of severity in SPM, encompassing the most severe type with concomitant pneumorrhachis and/or other extrathoracic air leak such as pneumoperitoneum and pneumoretroperitoneum (Figure 1C,D).
We hope this modified classification will be beneficial for future studies in a large scale or with prospective intent, enabling a validated outcome analysis based on degree of severity and drawing a more reliable and convincing conclusion in terms of diagnostic and therapeutic purposes for SPM.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Kim KS, Jeon HW, Moon Y, et al. Clinical experience of spontaneous pneumomediastinum: diagnosis and treatment. J Thorac Dis 2015;7:1817-24. [PubMed]
- Potz BA, Chao LH, Ng TT, et al. Clinical significance of spontaneous pneumomediastinum. Ann Thorac Surg 2017;104:431-5. [Crossref] [PubMed]
- Fitzwater JW, Silva NN, Knight CG, et al. Management of spontaneous pneumomediastinum in children. J Pediatr Surg 2015;50:983-6. [Crossref] [PubMed]
- Park SJ, Park JY, Jung J, et al. Clinical manifestations of spontaneous pneumomediastinum. Korean J Thorac Cardiovasc Surg 2016;49:287-91. [Crossref] [PubMed]
- Wong KS, Wu HM, Lai SH, et al. Spontaneous pneumomediastinum: analysis of 87 pediatric patients. Pediatr Emerg Care 2013;29:988-91. [Crossref] [PubMed]
- Iyer VN, Joshi AY, Ryu JH. Spontaneous pneumomediastinum: analysis of 62 consecutive adult patients. Mayo Clin Proc 2009;84:417-21. [Crossref] [PubMed]
- Oertel MF, Korinth MC, Reinges MH, et al. Pathogenesis, diagnosis and management of pneumorrhachis. Eur Spine J 2006;15 Suppl 5:636-43. [Crossref] [PubMed]
- Kono T, Kuwashima S, Fujioka M, et al. Epidural air associated with spontaneous pneumomediastinum in children: uncommon complication? Pediatr Int 2007;49:923-7. [Crossref] [PubMed]


