Thoracoscopic stapler-based “bidirectional” segmentectomy for posterior basal segment (S10) and its variants
Introduction
Segmentectomy for the posterior basal segment (S10) may be the most challenging anatomical segmentectomy, particularly if it is thoracoscopically conducted. Stapler-based segmentectomy provides better sealing of the lung parenchyma and thus expected to reduce post-operative air-leakage and associated complications such as empyema (1). However, the application of stapler-based segmentectomy to S10 is challenging for multiple reasons: (I) similar to other basal segments [e.g., anterior basal segment (S8)], three-dimensional stapling to fold a cuboidal segment is necessary (1); (II) the belonging pulmonary artery is not directly facing the interlobar fissure or the hilum, which makes identification of target artery difficult; (III) the anatomy of S10 and adjacent segments is variable.
There are several different strategies proposed. One is to separate superior (S6) and basal segments first and then resect the posterior part of the basal segment. However, this results in complete separation of S8 and S6 (2). Leaving a small segment alone is concerning regarding possible torsion of the segment. The effect on the lung volume may also be a relative concern. Another strategy is complete posterior approach, tracking the anatomy from the pulmonary vein, and then the riding bronchus and pulmonary artery. Although successful tracking of the hilar structures enables anatomical S10 segmentectomy without separating S6 and S8, the surgery tends to be tricky because of the difficulty in obtaining good exposure of hilar anatomy and resulting confusion, particularly the bronchus and pulmonary artery. For example, even if the exposed pulmonary artery and bronchus are considered to be A10 and B10, they are frequently more peripheral structures such as A10c and B10c, respectively. This kind of misunderstanding on anatomy may lead to unsatisfactory outcomes such as resection of insufficient lung tissue. Conversely, resection of a wrong hilar structure without appropriate confirmation of anatomy may necessitate larger resection than the original plan such as basal segmentectomy or even lobectomy.
To overcome the challenges and to achieve satisfactory outcomes, we herein report the “bidirectional” approach, by which surgeons can easily resolve the potential problems of S10 segmentectomy.
Operative techniques
Technical principle of stapler-based segmentectomy
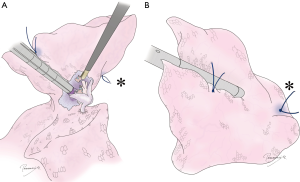
Technical details of stapler-based segmentectomy in general have been described previously (1). We usually use virtual-assisted lung mapping (VAL-MAP), a preoperative bronchoscopic multi-spot dye marking technique, to determine appropriate resection lines intraoperatively (3,4), although other methods such as conventional and applied inflation-deflation line (5), and intravenous or bronchoscopic indocyanine green (ICG) injection (6-8) are also usable. Regardless of the methods to demark resection lines, we recommend placing “standing stitches” along resection lines with a monofilament stitch such as 3-0 proline, especially at the corner of intersegmental plane(s) (Figure 1). These stitches are well visible at stapling even in limited vision of thoracoscope (Figure 1), even in a uniportal VATS approach of our recent experience.

After dissection of hilar structures, confirmation of anatomy is another key for successful segmentectomy. The hilar anatomy should be carefully inspected in the light of preoperative 3D images, and intraoperative bronchoscopy. Removal of hilar lymph nodes is also important not only for lymph node sampling but for exposure of clean anatomy (1). And then the target bronchus and vessels are resected by a stapler, energy device, or simply after tying. The hilar pulmonary parenchyma should be further resected along the intersegmental plane by approximately 1 cm. This maneuver creates space to allow for a stapler to be placed smoothly at the hilum (1).
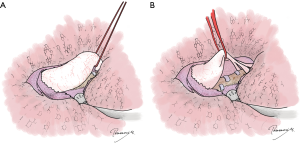
Finally, the intersegmental planes are resected by a stapler. The recommended principle of stapling is “peripherally to centrally” and “step-by-step” stapling. Namely, stapling is started from the thing, peripheral, and easy parts of the lung and continued to reach the most difficult hilar stapling and/or stapling of the thick lung tissue in a step-by-step manner. Especially in segmentectomies involving the basal segment of the lower lobe necessitating three-dimensional stapling, different peripheral stapling are done first and then the staple lines are connected together toward the center (1). Notably it is safe to place the cartilage side of the stapler to the hilum rather than the anvil side, which can easily damage the lung parenchyma or vessels (Figure 2). After removal of the specimen, sealing of the hilum using soft coagulation is effective in preventing air leakage.
Techniques specific to S10 segmentectomy step 1: anterior approach
Nowadays construction of 3D images based on thin-slice CT images is almost mandatory. Particularly the vascular and bronchial anatomy of S10 and adjacent segments such as S6, 9, and S7 is variable.
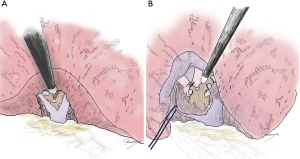
In the two-directional S10 segmentectomy, hilar dissection is started from the interlobar fissure. The purpose of this dissection is to obtain correct orientation of pulmonary artery, especially A9, A10, and their branches, which are often located deep in the lung. The interlobar pulmonary artery is exposed and then A6 and basal pulmonary artery should be easily identified. Although A8 is usually easily identified as well, the separation of A9, A10, and their branches are located deep in the lung. The visualization is often interfered with the existence of A8a and/or A9a, which stands up in front of the targeted deep structures. A technical tip is to encircle basal artery and retract it with a vessel tape. This maneuver helps to “pull up” the artery to visualize peripheral branches (Figure 3). Usually branching as far as to A10 or A10a can be visualized without resecting any pulmonary parenchyma. If the resection is S9+10, A9a for example can be resected at this stage, which help visualizing the deep structures. The taping of pulmonary artery also helps to visualize bronchus behind (Figure 3). It is ideal to encircle the target artery and resect it, followed by the target bronchus at this stage. However, as a reality, it is often felt too deep to safely encircle (especially A10 in S10 segmentectomy or A10b and c in subsegmentectomy). If this was the case, we leave the vessel tape encircling the basal artery or encircle a more peripheral branch such as A9+10 and then proceed to the next step. Once again, the key at this stage is clarify the anatomy of pulmonary artery from the interlobar fissure. Resection of pulmonary artery and bronchus can be done later from the posterior hilum.
Techniques specific to S10 segmentectomy step 2: posterior approach
As the second step, the posterior hilum is exposed. This is why we call this approach “bidirectional”. The pulmonary ligament is resected and the inferior pulmonary vein is exposed to examine the branching referring to the prepared 3D images. By tracking the pulmonary vein peripherally, the bronchus and pulmonary artery behind the venous branch can be exposed relatively easily (Figure 4). However, this posterior approach alone is difficult in correctly nominate the exposed pulmonary artery and bronchus. Very often, the exposed bronchus and artery are more peripheral ones than presumed. Also note that the lung is usually retracted anteriorly to expose the posterior hilum, pulmonary artery and bronchus are retracted as well, making the anatomy even more confusing. A10 running caudally may look running even anteriorly. At this stage, identification of the pulmonary artery and bronchus from the interlobar fissure is of great help. By tracking the pulmonary artery and bronchus centrally, the vessel tape encircling the pulmonary artery can be identified. If the target artery and bronchus are already resected from the fissure side, the stumps can be reached relatively easily.
Exposure of the bronchus and pulmonary artery is often felt unsatisfactory and difficult because they are still hidden behind the lung parenchyma. We do not hesitate to start creating the posterior intersegmental plane between S6 and S10 from the posterior approach (Figure 5A). Just a single stapling dramatically improves the hilar exposure. If the posterior space is felt too small for stapling, energy device could also be used to resect the lung parenchyma.
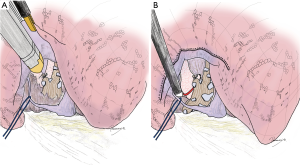
If the vessel tape encircling the pulmonary artery cannot be visualized yet, exposure of structures belonging to S6 (V6 and B6) is also recommended. Namely, by taping V6 and retracting it cranially, the basal bronchus can easily be tracked centrally toward the bronchus intermedius on the right side or the main bronchus on the left side (Figure 5B). Once branching to B6 is identified, it becomes an important landmark to exposure more central pulmonary artery. This maneuver is particularly useful when the anatomy of S6 is complex such as the case of dual branching of B6, wherein S6 tends to be larger than usual.
These maneuvers of resecting S6–S10 intersegmental plane and exposure of S6 structures make the approach much safer than “digging a hole” along a peripheral pulmonary artery. Bronchial anatomy can and should always be confirmed by intraoperative bronchoscope.
Techniques specific to S10 segmentectomy step 3: stapler-based development of intersegmental line
Once the anatomy is clear, the target artery, vein, and bronchus are resected. Confirmation of bronchial branching by interoperative bronchoscopy is mandatory. Following resection of all the targeted hilar structures, the intersegmental planes are made using staplers based on the principle of “peripherally to centrally” and “step-by-step stapling” as was described previously (1). For S10 segmentectomy, followed by the posterior separation of S6/S10 (Figure 5A), we usually staple the lung facing the diaphragm (Figure 6A,B,C; arrows b to f, and c to g, and then f to g). And then the lung tissue between the two resection lines are further stapled (Figure 6A,B,C; arrows g to h, and h to e). The resulting lung after completion of S10 segmentectomy is shown in Figure 6D,E.
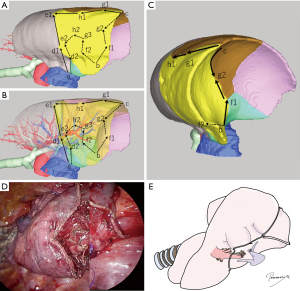
Management of S7
Particularly on the right side, special attention should be paid to the resection line between S7 and S10 (arrow b to f in Figure 6). A typical mistake is to set this line “downwards” as shown in the interrupted arrow in Figure 7, which tends to result in congested, useless S7 shaping like a “peninsula”. Because surgeons intend to preserve the lung volume as much as possible, such a downward resection line seems especially tempting if a part of S7 is protruding laterally beyond the pulmonary ligament (Figure 7B). Rather we recommend stapling this part in a relatively “upward” manner, somewhat medial to the pulmonary ligament (solid arrows in Figure 7). On the diaphragm side, it is better not to go too deep toward the center of the diaphragm (i.e., to make the angle b-f in Figure 6C not too sharp). At the hilum, attention should also be paid to preserve the pulmonary vein draining from S7.
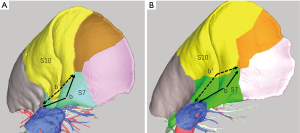
This technique usually results in resecting a part of S7, although the loss of the lung volume and/or lung function appears to be minimal. If it is really necessary to preserve the complete S7, the technique using electrocautery may be better than stapling. Indeed, at the extension of the pulmonary ligament, there may be a fibrous layer bordering S7 and S10, which is well separated by electrocautery without causing air leakage.
Comments
The stapler-based segmentectomy for S10 or related ones (e.g., S9+10 segmentectomy, S9b+c combined subsegmentectomy) is probably the most challenging one among different types of segmentectomies. This is because of the anatomical property of this segment, including (I) three-dimensional stapling is necessary similar to other basal segments (1); (II) the belonging pulmonary artery is not directly facing the interlobar fissure or the hilum but hidden behind the pulmonary vein and thus disorientation could happen relatively easily; (III) the anatomy of S10 and adjacent segments is variable. To overcome these challenges one by one, we herein summarized the technique of S10 segmentectomy, particularly focusing on the stapler-based “bidirectional” method wherein complete separation of S6 and basal segment is not necessary.
Stapler-based segmentectomy is easier if it can be completed by “linear” stapling (e.g., S2, S6, and lingular) or U-shaper or V-shaped stapling (e.g., right S1, left S3, right S2b+3a) (1). Conversely, in what we call “three-dimensional” segmentectomy, the intersegmental planes make a cuboid-shaped segment primarily because of the plane phasing the diaphragm. This anatomical characteristic of the segment makes it difficult to imagine how multiple stapling folds the cuboidal segment. As was described previously, the principle of “staple from the periphery to the center” and “step-by-step” stapling along the “standing” marking stitches allows for effective stapling even in limited thoracoscopic view (1).
In addition to the necessity of the three-dimensional stapling, segmentectomy of S10 and its variants is further challenging because the belonging pulmonary artery, the primary landmark of segmentectomy, is not facing either the interlobar fissure or the hilum, but hidden behind the inferior pulmonary vein from the posterior view. The anatomy of pulmonary artery cannot be tracked from the central part where the anatomy is obvious. We herein described the advantage of the two-directional approach, which allows for correct understanding of the patient’s hilar anatomy from the posterior hilum without separating S6 and basal segments. As was described previously, complete separation of S6 and basal segment allows for clear visualization of hilar anatomy (2). Although this approach is technically easier, it leaves relatively small segments separated, which is potentially concerning in the function and the torsion of the segment. The two-directional approach allows for anatomical confirmation from the fissure, while stapler-based resection of the segment from the posterior hilum.
Lastly, the anatomy of S10 and its adjacent segments is quite variable among patients. It is critical to understand the patient’s anatomy using three-dimensional imaging and to confirm it using multiple modalities during operation such as bronchoscopy, reference of preoperative three-dimensional imaging, and the two-directional approach as was mentioned above. Particularly, we herein focused on the management of S7 in this article because this relatively minor segment is rarely under the spotlight but actually almost always a problem in S10 segmentectomy on the right side. Unfortunately, complete resection of S10 using a stapler often results in resection of a part of S7 to avoid excessive congestion. We consider it is important to understand this anatomical property before operation and to appropriately manage it.
Acknowledgements
The authors thank Drs. Kentaro Kitano, Jyun-ichi Nitadori, and Kazuhiro Nagayama for providing operative videos and pictures.
Funding: This work was funded by Japan Agency of Medical Research and Development, category of medical arts, 17ck0106244h0002.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: We do not obtain informed consent for this particular publication, although the patients participated in a study with written informed consent. We consider registration at a research comprehensively include potential publication.
References
- Sato M, Murayama T, Nakajima J. Techniques of stapler-based navigational thoracoscopic segmentectomy using virtual assisted lung mapping (VAL-MAP). J Thorac Dis 2016;8:S716-30. [Crossref] [PubMed]
- Yamanashi K, Okumura N, Otsuki Y, et al. Stapler-based thoracoscopic basilar segmentectomy. Ann Thorac Surg 2017;104:e399-402. [Crossref] [PubMed]
- Sato M, Kuwata T, Yamanashi K, et al. Safety and reproducibility of virtual-assisted lung mapping: a multicentre study in Japan. Eur J Cardiothorac Surg 2017;51:861-8. [PubMed]
- Sato M, Omasa M, Chen F, et al. Use of virtual assisted lung mapping (VAL-MAP), a bronchoscopic multispot dye-marking technique using virtual images, for precise navigation of thoracoscopic sublobar lung resection. J Thorac Cardiovasc Surg 2014;147:1813-9. [Crossref] [PubMed]
- Okada M, Mimura T, Ikegaki J, et al. A novel video-assisted anatomic segmentectomy technique: selective segmental inflation via bronchofiberoptic jet followed by cautery cutting. J Thorac Cardiovasc Surg 2007;133:753-8. [Crossref] [PubMed]
- Tarumi S, Misaki N, Kasai Y, et al. Clinical trial of video-assisted thoracoscopic segmentectomy using infrared thoracoscopy with indocyanine green. Eur J Cardiothorac Surg 2014;46:112-5. [Crossref] [PubMed]
- Oh S, Suzuki K, Miyasaka Y, et al. New technique for lung segmentectomy using indocyanine green injection. Ann Thorac Surg 2013;95:2188-90. [Crossref] [PubMed]
- Sekine Y, Ko E, Oishi H, et al. A simple and effective technique for identification of intersegmental planes by infrared thoracoscopy after transbronchial injection of indocyanine green. J Thorac Cardiovasc Surg 2012;143:1330-5. [Crossref] [PubMed]


