A quality improvement program with nutrition therapy: restriction of lipid emulsions in cardiac surgical patients
Introduction
Nutritional treatment plays a unique role in the integrated management of post-cardiac surgery patients. It is known that poor nutritional status is associated with higher mortality, an increased postoperative infection risk, a prolonged length of intensive care unit (ICU) and hospital stay, and a poorer quality of life in post-cardiac surgery patients (1). It is recommended that nutrition support therapy in the form of early enteral nutrition (EN) be initiated within 24–48 hours in a critically ill patient who is unable to maintain volitional intake (2). However, most patients who have undergone cardiac surgery experienced postoperative hemodynamic instability courses, and some required high doses of vasopressor or even mechanical hemodynamic support, which led to inadequate calorie intake via the enteral route alone.
The ASPEN/SCCM guidelines recommend that for patients who are at either a low or high nutrition risk, the use of supplemental parenteral nutrition (SPN) should be considered after 7–10 days if the patients are unable to meet >60% of their energy and protein requirements via the enteral route alone (2). Nevertheless, in patients who are intolerant to EN within 72 hours of admission, the European guidelines recommend starting SPN within 24 to 48 hours (3). A cross-sectional study revealed that parenteral nutrition (PN) was predominantly used in patients requiring nutritional support in Mainland China. The ratio of PN to EN in the sampling areas was approximately 1.7:1.0, which indicated that the choice of nutritional support was occasionally inappropriate (4). Hence, there was a huge gap between the guidelines and real-world clinical practice in Mainland China.
Despite the wide use of PN, the necessity and safety of the component have not been well studied. Lipid emulsions are considered essential components of PN regimens that provide a concentrated source of calories, cell membrane components and biologically active substrates. Traditional soybean oil-based intravenous fat emulsions (IVFEs) are high in linoleic acid, which has been hypothesized to exacerbate the inflammatory immune response and result in adverse outcomes in critically ill patients (5). Furthermore, lipid emulsions have been implicated in the development of hepatobiliary disease in patients receiving PN (6,7). A restriction to intravenous soybean-based lipid in PN-fed surgical infants has been reported to be associated with a reduction in the incidence of liver disease (8).
The purpose of this study was to determine whether the restriction of IVFEs would be associated with reduced mortality and occurrence of nosocomial infections during ICU stay in cardiac surgical patients.
Methods
Study design
The study was conducted in a 38-bed cardiac surgery ICU (CSICU) at Zhongshan Hospital of Fudan University, China, from May 1, 2015, to November 30, 2015. This hospital, which is one of the largest centers for cardiovascular medicine in mainland China, performed more than 3,000 cardiac surgery procedures per year. A before-and-after interventional study was conducted to compare the clinical outcomes regarding the intervention. Two consecutive study periods were analyzed: (I) Period A, a 3-month baseline period before IVFE restriction (May to July 2015); and (II) Period B, a 4-month period with the implementation of IVFE restriction (August to November 2015). Data were collected from the medical records from Zhongshan Hospital Electronic Health Record System. This study was approved by the Ethics Committee of Zhongshan Hospital Affiliated to Shanghai Fudan University (No. B2016-142R) and was conducted in compliance with the institutional requirements.
Inclusion and exclusion criteria
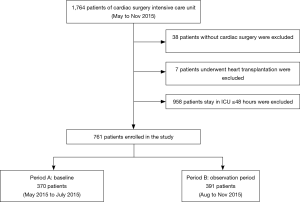
All patients who underwent cardiac surgery and were admitted to the CSICU were included in this study. The exclusion criteria were as follows: (I) patients who did not receive cardiac surgery, such as those with type A aortic dissection who were admitted to the CSICU from emergency room but died before the surgical intervention; (II) patients who underwent heart transplantation; and (III) patients who stayed in CSICU for less than 48 hours. The flowchart of patient enrollment was summarized in Figure 1.
Study procedures
The nutritional treatment protocol in our cardiac surgery intensive care unit (CSICU) is shown in Figure 2. The energy targets were set at 25 kcal/kg/day throughout the study period. Continuous intravenous insulin therapy to maintain blood glucose at lower than 10 mmol/L was provided, and the arterial blood glucose levels were checked frequently (depending on the clinical situation, but this occurred at least three times a day). Energy delivery was defined as the mean actual caloric intake per day during the ICU stay, which included fat from propofol. Energy balance was defined as the difference between energy target and energy delivery.

EN was initiated for patients who were on mechanical ventilation approximately 24 h after cardiac surgery. Nasogastric tubes were considered the preferred choice. Gastric residual volume was not routinely monitored in our CSICU. In non-diabetic patients, EN products containing 1.5 kcal/mL of energy (6 g/100 mL proteins, 5.83 g/100 mL lipids, and 18.4 g/100 mL carbohydrates) were administered. In patients with diabetes mellitus, the EN formulas consisted of 1 kcal/mL of energy (3.4 g/100 mL proteins, 3.2 g/100 mL lipids, and 12 g/100 mL carbohydrates). Patients who were extubated after cardiac surgery were encouraged to be orally fed.
Before August 2015, PN with a soybean-based lipid emulsion containing 450 kcal was routinely implemented if the patients failed to meet >60% of their energy requirements within 48 h post-cardiac surgery. The PN formulas consisted of 1.14 kcal/mL of energy (18% proteins, 34% lipids, and 48% carbohydrates). The team of intensivists gradually realized that such an aggressive use of IVFEs was not in accordance with the current ASPEN/SCCM guidelines (2). After a series of multidisciplinary discussions, beginning in August 2015, a lipid restriction strategy was implemented at our CSICU for all cardiac surgery patients. IVFEs were only considered after 7 days if the enteral route could not be established, as in situations such as with gastrointestinal bleeding. After this change was discussed by the interdisciplinary team and documented in the updated protocol, it was firmly implemented by the whole team. Alternative IVFEs containing fish oil or olive oil were not administered during the study period. Highly concentrated glucose (25% or 50%) were administered instead of IVFEs to supplement the calories, if necessary. There were no alterations in the goal protein provisions for IVFE-restricted patients. The initiation and advancement of enteral nutrition were encouraged throughout the study period.
Clinical outcomes
The primary endpoint of the study was the occurrence of nosocomial infections during ICU stay. Four infection categories were evaluated in this study: pulmonary infection, wound infection, blood stream infection (BSI) and urinary infection. The main secondary endpoint was in-ICU and in-hospital mortality. Other secondary endpoints included the following: (I) length of ICU and hospital stay; (II) ICU and hospital cost; (III) mechanical ventilation time; and (IV) postoperative complications.
Statistical analysis
Normal distributed data are expressed as the mean ± standard deviation, and non-normal distributed data are expressed as medians and interquartile range (IQR). Continuous data were compared using an unpaired t-test or a Wilcoxon test. Pearson’s chi-squared test or Fisher’s exact test (when the count in any cell of a contingency table was less than required) was used for categorical variables. Multivariate regression analysis was performed to compare between-group differences in the outcomes. A propensity score method was employed to control for the bias caused by patient selection using the inverse probability of treatment weighting (IPTW) method. All tests were two-tailed, and a P value less than 0.05 was considered statistically significant. SPSS for Windows 19.0 (Chicago, IL, USA) was used for statistical analysis.
Results
Patient characteristics
From May to November 2015, 1,764 patients were admitted to the CSICU. Thirty-eight patients who did not receive surgical intervention and 7 patients who received heart transplantation were excluded from this study. A total of 958 patients who stayed in CSICU for less than 48 hours were also excluded; thus, 761 patients (370 patients in Period A and 391 patients in Period B) were ultimately enrolled into this study (Figure 1).
The demographic data are summarized in Table 1. There was no statistically significant difference between the groups regarding patient age, gender, body mass index (BMI), major comorbidities (hypertension, diabetes mellitus, hyperlipidemia, chronic obstructive pulmonary disease, peptic or gastric ulcer, chronic kidney disease, and neurological dysfunction), prior cardiac surgery history or preoperative cardiac function. The preoperative BMIs in both groups were within the normal range. Regarding the preoperative nutritional status, there was no statistically significant difference between Periods A and B in terms of the total protein, albumin, or modified score of nutrition risk in critically ill patients (modified NUTRIC score).
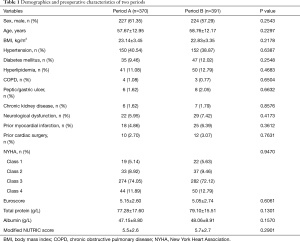
Full table
Intraoperative and postoperative parameters
The intra- and postoperative data are summarized in Table 2. Of the enrolled patients, 446 (58.61%) underwent isolated valve surgery, 178 (23.40%) underwent isolated coronary artery bypass grafting (CABG), 37 (4.86%) underwent combined valve procedure and CABG, 51 (6.70%) underwent aortic surgery, and 49 (6.44%) underwent other cardiac procedures. The European System for Cardiac Operative Risk Evaluation (Euroscore) and the Acute Physiology and Chronic Health Evaluation (APACHE) II were not statistically significantly different between the groups. There was no statistically significant difference in the proportion of emergency surgery, cardiopulmonary bypass (CPB) time, clamping time, intra-aortic balloon pump (IABP) use, extracorporeal membrane oxygenation (ECMO) use or continuous renal replacement therapy (CRRT) use.
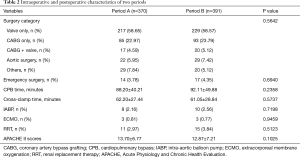
Full table
Nutrition measures
After the implementation of IVFEs restriction, a similar proportion of ICU patients received SPN (20.27% vs. 22.51%) and total PN (TPN) (5.14% vs. 5.62%). The usage of IVFEs was significantly reduced in patients receiving SPN and TPN therapy. Only one patient received IVFEs due to short bowel syndrome because of mesenteric arterial embolism in the latter period. The proportion of oral feeding and EN was comparable between the groups.
The energy target was not significantly different between the periods. However, the energy delivery was statistically significantly reduced after the implementation of IVFE restriction (1,117±692 vs. 1,236±677 kcal/day, P=0.0168). Therefore, a greater negative energy balance was found in the latter period (−572±421 vs. −482±401 kcal/day, P=0.0026) (Table 3).
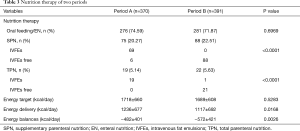
Full table
Clinical outcomes
The overall ICU mortality and hospital mortality were similar between the groups. After the implementation of IVFE restriction, the nosocomial infection rate was statistically significantly reduced (3.84% vs. 7.84%, P=0.0210), as confirmed after multivariate adjustment for age, gender, BMI, New York Heart Association (NYHA) classification, Euroscore, APACHE II score and postoperative complications (RR 0.50, 95% CI 0.25–0.96, P=0.0389). For the specific causes of infection, bloodstream infection was found to be significantly lower in Period B (0.77% vs. 5.41%, P=0.0015), as confirmed by multivariate analysis (RR 0.14, 95% CI 0.04–0.50, P=0.0025). In addition, there was no statistically significant difference between the groups in pulmonary infection (P=0.0561), wound infection (P=0.5356) or urinary tract infection (P=0.6674). The mean lengths of ICU stays (3.15 vs. 3.74 days, P<0.001) and hospital stays (12.14 vs. 13.24 days, P<0.001) were both statistically significantly shorter in Period B. Moreover, the mean in-hospital cost (133,368 vs. 139,383 Yuan, P=0.037) was also found to be reduced after the implementation of IVFE restriction. The duration of mechanical ventilation was statistically significantly shorter in Period B (35.23±10.43 vs. 47.63±12.54 hours, P=0.011). Postoperatively, the occurrence of complications including gastrointestinal bleeding and neurological dysfunction were comparable between the groups. Cholestasis defined as a direct bilirubin >2 mg/dL on two consecutive measurements was statistically significantly reduced in the latter period (2.81% vs. 6.76%, P=0.013) (Table 4).
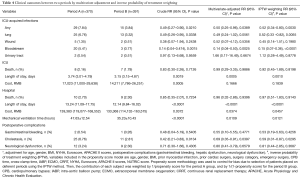
Full table
Discussion
The findings of this study indicate that the implementation of soybean-based IVFEs restriction in cardiac surgical patients reduced incidence of postoperative nosocomial infections. The main goal of nutritional support in post-cardiac surgery patients is to maintain an adequate nutritional supply, prevent potential malnutrition and decrease the risk of nosocomial infections (9,10). Despite recent improvements in the application of nutritional support in China, a much higher percentage of nitrogen and lipids is delivered through PN than through EN according to a cross-sectional study (4). IVFEs are able to provide sufficient caloric support and essential fatty acids to correct the energy deficit; however, it remains unclear whether perioperative IVFE administration in cardiac surgery patients will lead to improved clinical outcomes (11,12).
This study revealed that the compliance to guidelines is poor as reported by the previous study (4). The negative effects of soybean-based IVFEs have already been described by ASPEN/SCCM guidelines. Withholding or limiting soybean-based IVFE during the first week was suggested according to the guidelines. Alternative IVFEs may provide outcome benefit over soybean-based IVFEs; however, no recommendation was made due to lack of availability of these products in the US (2).
Contradictory results have been reported regarding the IVFEs and nosocomial infections. Battistella et al. showed that IVFEs during the early post injury period increased susceptibility to infection, prolonged pulmonary failure, and delayed recovery in critically injured patients. However, it is not clear whether the improved outcome in the IVFEs sparing group was directly related to withholding the IVFEs or was due to the hypocaloric nutritional regimen (underfeeding) that these patients received (13). In contrast, the analysis of a large US database of patients receiving premixed PN found that when it was administered with premixed PN, lipid emulsion was not significantly associated with an increase in the risk of infectious morbidity compared to omitting lipids from therapy (14). In the current study, we implemented an IVFE restriction program in a high-capacity CSICU that effectively reduced the postoperative nosocomial infection rate and shortened the ICU and hospital stay.
The CALORIES trial randomly assigned 2,400 adult critically ill patients who could be fed through either the parenteral or the enteral route to a delivery route. The trial found no significant difference in 30-day mortality associated with the route of delivery of early nutritional support (15). Hence, the association of early PN with worse outcome may not be route-related. One major possible explanation for the improved outcomes after IVFE restriction could be that the IVFEs administered in this study were soybean-based, which may have exaggerated the inflammatory response and promoted immunosuppressive effects such as apoptosis of immune cells or diminished phagocytosis of granulocytes (7,16). According to the current guidelines, alternative IVFEs might be considered for PN regimens in the critically ill, but more consistent evidence is needed. It is worth noting that soybean-based lipid emulsions were the only type of lipid emulsion available at this time in our hospital. It was reported that soybean-based IVFEs were associated with an elevated risk of adverse clinical outcomes, possibly due to their high content of omega-6 fatty acids, which may exacerbate the inflammatory immune response (17). Grau-Carmona et al. reported that the number of patients with nosocomial infections was significantly reduced in a fish oil-receiving group and the predicted time free of infection was prolonged. No significant differences were detected in the ICU, hospital, and 6-month mortality (18). The results of the multi-center database analysis suggested that both lipid-free and soybean-sparing strategies were better than soybean-based PN for critically ill patients (16). Thus, apart from providing energy and essential fatty acids, soybean-based IVFEs would appear to offer no other clinical benefits in the ICU (19).
During our clinical practice, after the implementation of IVFEs restriction, the adequacy of calories supply was a major concern for both intensivists and surgeons, some of whom worried that patients would not be able to achieve a sufficient energy supply and would thus suffer from malnutrition, which would lead to poor outcomes. In this study, the actual energy delivery was significantly reduced after IVFE restriction; therefore, a more negative energy balance was found in the latter period. However, the gap of energy balance between the groups was fairly small (only approximately 90 kcal/day), which could hardly explain the different prognoses in the two groups.
Our study has several limitations. First, this was a single-center and historical control study that was compared with retrospective nutritional therapy data. The retrospective data collection and outcome evaluation might have certain inevitable bias. Therefore, the findings merit further study with prospective trials to evaluate the effect of IVFEs restriction in cardiac surgical patients. Second, the intensivists and other health providers were all aware of study-group assignments because this change was discussed by the interdisciplinary team and documented in the updated protocol. Whether the improved outcome might be related to the “Hawthorne effect” remains uncertain. Third, the amount of nutrition was calculated without measuring the energy expenditure. Fourth, IVFE restriction may arouse a more positive attitude to EN to achieve the nutritional target. Whether the positive outcome was associated with increased EN use was not fully evaluated. Fifth, this was only a quality improvement program for the lipid emulsions; further improvement on other potential aspects might also be achieved. Finally, soybean-based IVFEs were used in PN in the Period A. Whether the conclusions can be extrapolated to other IVFEs remains to be further determined.
Conclusions
The implementation of soybean-based IVFEs restriction in cardiac surgical patients was associated with a lower postoperative nosocomial infection rate. It also led to reductions in the length of ICU/hospital stay, hospital costs and mechanical ventilation time and a lower incidence of cholestasis. Further prospective randomized studies are required to validate our conclusions. The adherence to critical care nutrition guidelines should be improved.
Acknowledgements
Funding: This article was supported by grants from the National Natural Science Foundation of China (No. 81500067), Natural Science Foundation of Shanghai (No. 16ZR1405600), Health and Family Planning Commission of Shanghai (No. 20154Y011) and the research funds of Zhongshan Hospital (No. 2017ZSQN16 and 2017ZSYXQN23).
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: This study was approved by the Ethics Committee of Zhongshan Hospital Affiliated to Shanghai Fudan University (No. B2016-142R) and was conducted in compliance with the institutional requirements.
References
- Evans AS, Hosseinian L, Mohabir T, et al. Nutrition and the Cardiac Surgery Intensive Care Unit Patient--An Update. J Cardiothorac Vasc Anesth 2015;29:1044-50. [Crossref] [PubMed]
- McClave SA, Taylor BE, Martindale RG, et al. Guidelines for the Provision and Assessment of Nutrition Support Therapy in the Adult Critically Ill Patient: Society of Critical Care Medicine (SCCM) and American Society for Parenteral and Enteral Nutrition (A.S.P.E.N.). JPEN J Parenter Enteral Nutr 2016;40:159-211. [Crossref] [PubMed]
- Singer P, Berger MM, Van den Berghe G, et al. ESPEN Guidelines on Parenteral Nutrition: intensive care. Clin Nutr 2009;28:387-400. [Crossref] [PubMed]
- Han G, Yu Z, Ma K. Current status of parenteral nutrition and enteral nutrition application: an assessment of nutritional prescriptions from 59 hospitals in the People's Republic of China. Ther Clin Risk Manag 2015;11:201-7. [PubMed]
- Boisramé-Helms J, Toti F, Hasselmann M, Meziani F. Lipid emulsions for parenteral nutrition in critical illness. Prog Lipid Res 2015;60:1-16. [Crossref] [PubMed]
- Teitelbaum DH, Tracy T. Parenteral nutrition-associated cholestasis. Semin Pediatr Surg 2001;10:72-80. [Crossref] [PubMed]
- Wanten GJ. Parenteral Lipid Tolerance and Adverse Effects: Fat Chance for Trouble? JPEN J Parenter Enteral Nutr 2015;39:33S-8S. [Crossref] [PubMed]
- Sanchez SE, Braun LP, Mercer LD, et al. The effect of lipid restriction on the prevention of parenteral nutrition-associated cholestasis in surgical infants. J Pediatr Surg 2013;48:573-8. [Crossref] [PubMed]
- Koekkoek KW, van Zanten AR. Nutrition in the critically ill patient. Curr Opin Anaesthesiol 2017;30:178-85. [Crossref] [PubMed]
- Mulherin DW, Cogle SV. Updates in Nutrition Support for Critically Ill Adult Patients. Hosp Pharm 2017;52:17-26. [Crossref] [PubMed]
- Langlois PL, Hardy G, Manzanares W. Omega-3 polyunsaturated fatty acids in cardiac surgery patients: An updated systematic review and meta-analysis. Clin Nutr 2017;36:737-46. [Crossref] [PubMed]
- Hecker M, Mayer K. Intravenous lipids in adult intensive care unit patients. World Rev Nutr Diet 2015;112:120-6. [Crossref] [PubMed]
- Battistella FD, Widergren JT, Anderson JT, et al. A prospective, randomized trial of intravenous fat emulsion administration in trauma victims requiring total parenteral nutrition. J Trauma 1997;43:52-8; discussion 58-60. [Crossref] [PubMed]
- Pontes-Arruda A, Liu FX, Turpin RS, et al. Bloodstream infections in patients receiving manufactured parenteral nutrition with vs without lipids: is the use of lipids really deleterious? JPEN J Parenter Enteral Nutr 2012;36:421-30. [Crossref] [PubMed]
- Harvey SE, Parrott F, Harrison DA, et al. Trial of the route of early nutritional support in critically ill adults. N Engl J Med 2014;371:1673-84. [Crossref] [PubMed]
- Edmunds CE, Brody RA, Parrott JS, et al. The effects of different IV fat emulsions on clinical outcomes in critically ill patients. Crit Care Med 2014;42:1168-77. [Crossref] [PubMed]
- Calder PC. Hot topics in parenteral nutrition. Rationale for using new lipid emulsions in parenteral nutrition and a review of the trials performed in adults. Proc Nutr Soc 2009;68:252-60. [Crossref] [PubMed]
- Grau-Carmona T, Bonet-Saris A, Garcia-de-Lorenzo A, et al. Influence of n-3 polyunsaturated fatty acids enriched lipid emulsions on nosocomial infections and clinical outcomes in critically ill patients: ICU lipids study. Crit Care Med 2015;43:31-9. [Crossref] [PubMed]
- Calder PC. Fishing for improved outcomes in the critically ill. Crit Care Med 2014;42:1306-7. [Crossref] [PubMed]


