Factors associated with generic health-related quality of life (HRQOL) in patients with chronic obstructive pulmonary disease (COPD): a cross-sectional study
Introduction
Chronic obstructive pulmonary disease (COPD) is a common respiratory disease with life-time prevalences ranging from 1.2% (Malta) to 13.2% (Germany) in Europe (1,2). Globally, COPD is the third leading cause of death (3). COPD is usually a progressive disease which is characterized by an airflow limitation that is not fully reversible. Common symptoms are chronic cough, sputum production and dyspnea (4). Due to the ongoing demographic change and the higher prevalence with increasing age (2), the number of COPD patients is estimated to rise by 47% by the year 2050 in Germany compared to numbers of 2007 (5). Since COPD has a major negative impact on the quality of life (QOL) and work productivity of COPD patients, it also poses a high burden on the economy in Germany (6).
In order to fully display the whole burden of disease, many studies emphasize the importance of measuring QOL (7-10). Particularly health-related quality of life (HRQOL) is more and more investigated, meaning the part of QOL in general that is determined by health. In order to quantify the impact of the disease on patients, studies use both generic and disease-specific instruments (11). Generic instruments, such as the Short-Form 12 (SF-12) questionnaire (12) used in this study, measure overall HRQOL and provide an advantage compared to disease-specific questionnaires, as they allow comparisons with other diseases or the general population.
Compared to healthy persons, previous studies showed a significantly lower physical and mental HRQOL in patients with COPD (13,14). Therefore, one aim in the German guidelines for diagnosis and therapy of COPD is the improvement of both health status and QOL (15).
Knowledge about determining factors of HRQOL is a mandatory prerequisite to improve it. Previous studies considered factors such as age, sex and co-morbidity (14,16) and revealed conflicting results (7). For instance, one study performed in the Netherlands found a higher age as a negative predicting factor for the health status of COPD patients (8) while another study from the USA found that younger patients had worse health status (17). Clear findings regarding influencing factors in previous studies exist for dyspnea, which seems to be the most important determinant of HRQOL in COPD patients (7,13). Based on strong evidence arising out of a systematic review, reduced HRQOL in COPD patients is negatively associated with depression and anxiety (18). So far, most studies have focused either on mild severity of disease using population based (13,19) or primary care based samples (8,20) or on severe cases only using data from secondary care settings (17,21).
The objective of this study is to identify factors associated with generic HRQOL in patients with COPD recruited from both primary and secondary care settings in Germany.
Methods
Study design and study population
The design of this study has been previously described in Böhmer et al. 2016 (22). In short the current study is based on data collected for a prospective patient cohort study investigating the influence of beliefs about medicines on adherence in patients with asthma or COPD. For the study presented here only patients with COPD are investigated. In order to cover a broad range of disease severity, patients were recruited from primary care and specialist practices as well as from in- and outpatients from hospital settings. The study sites are located in the region of Regensburg in the German federal state of Bavaria. The recruitment period for the baseline survey was from June 2013 until December 2014. Only patients who met the following inclusion criteria were enrolled in the study: COPD as main diagnosis ascertained by a physician, age ≥18 years; disease duration ≥3 months; no acute psychiatric/neurological disease (exception: depression or affective disorders) and sufficient knowledge of the German language. After a short introductory explanation all patients gave informed consent on-site before filling in the questionnaire. Data was collected both by using validated instruments and information from the patients’ medical records. Based on previous studies we determined a priori that we would investigate variables belonging to the domains patient characteristics, disease characteristics, treatment-related factors and psychological characteristics, as we aimed to take a broad perspective on variables likely influencing HRQOL.
Definition of variables
HRQOL: dependent variable
As a short version of the Short-Form (SF) 36 questionnaire (23), the SF-12 questionnaire contains 12 items in two scales: a physical (PCS-12) and mental health component scale (MCS-12) (12). The SF-12 explains the majority of the variance (80–85%) of the SF-36. The scores for the two scales were calculated as described by Ware et al. (12). Response categories differ from binary to six response options (like “always” to “never”). A range of 0 (worst conceivable QOL) to 100 (best conceivable QOL) is possible. For analysis, two summary scores were computed (12). The mean value of the German norm sample, which was used for standardization of scale scores in this study, is 50 in both the mental and physical component.
Patient characteristics
Sociodemographic data (age, gender and migration background), as well as information on estimated travelling time to the treating physician (in minutes) and the living situation (whether participants lived alone or not) were collected. Furthermore, the patients’ current smoking status was queried.
Level of education was divided into two groups for this analysis: low education level (no school degree or school leaving diploma after 9 school years) and high education level (school diploma after 10 school years or university entrance diploma).
Characteristics of disease
COPD symptoms and functional status were measured using the COPD Assessment Test (CAT) (24,25). The CAT score has an overall range of 0–40 and comprises eight questions with five response categories each (0= no impairment). The overall CAT score can be derived as a sum of each single item score. A score of <10 indicates a low impact, a score between 10 and 20 a medium impact and a score of more than 20 indicates a high impact level (26). For this analysis, CAT was calculated as continuous variable. Higher scores indicate more symptoms and functional impairment.
In addition, the duration of disease (in years) was obtained by asking for year of first diagnosis. Furthermore, we assessed the exacerbation history in the previous 12 months as an important reflection of disease control and as a potential predictor of the course of disease (27). The latest forced expiratory volume in 1 second (FEV1) value in percent predicted (obtained from the medical record) was also taken into account. A classification of severity of airflow limitation in COPD patients is given from the “Global Initiative for chronic obstructive lung disease” (GOLD) (4) and is based on post bronchodilator FEV1 values. Patients are classified as mild COPD (GOLD1) if their FEV1 is ≥80% predicted. A moderate COPD (GOLD2) includes FEV1 values between 50% and 80% predicted. If the patients’ FEV1 is between 30% and 50% predicted they are categorized as severe COPD or GOLD3. Very severe COPD (GOLD4) is present if FEV1 is less than 30% predicted. For analysis, only FEV1 in % predicted is taken into account, as GOLD status comprises the pulmonary function parameter and is therefore redundant.
Treatment of disease
The presence of severe side effects and the number of medical consultations due to COPD during the last year were enquired in the questionnaire. Patients were also asked whether they had ever taken part in a rehabilitation measure owing to COPD. Valid information on the patient´s current medication was obtained from the medical record. For analysis the total number of prescribed drugs was taken into account.
Psychological influences
To measure symptoms of anxiety and depression the German version of the hospital anxiety and depression scale (HADS) was used (28). The total of 14 items was divided into two subscales (anxiety and depression scale) with 7 items each. Scores are constructed by summation, whereby both scores were classified into three categories: inconspicuous findings (≤7), marginally noticeable findings (8-10) and noticeable findings (≥11) (29). In Germany, the mean scores of the general population are 4.7 for women and 4.6 for men (HADS-D) and 5.0 and 4.4 (HADS-A), respectively (30).
Statistical analysis
First, we performed a descriptive analysis. Continuous variables are reported as means (with minimum and maximum) and categorical variables as proportions. In a second step, we performed a univariate analysis in which all potential determinants were entered separately in linear regression models, with the physical and mental component summary scores (PCS-12/MCS-12) of the SF-12 as dependent variables, respectively. Finally, all variables with a significant association in the univariate analysis were used as predictive variables in the multivariable model. For regression analysis, the level of significance was defined based on the confidence interval with an alpha error less than 0.05. In case of missing data, the respective variables of these patients were not included in the analysis. All analyses were performed by using SPSS 22 (SPSS Inc., Chicago, USA).
Results
Characteristics of the study population
Data from 206 patients with COPD were analyzed. Of the seven study sites, three were practice and four were hospital settings. On average, COPD patients were 65 years old (SD =8.85) and approximately two thirds of them were of male sex. In total, 20.2% stated current smoking. On average, the diagnosis of COPD was made eight years (SD =7.92) before enrolment into the study. When categorizing the disease in four stages of disease severity, only a minority (4.7%) was grouped in the mildest stage GOLD 1. The largest group with 66 patients was GOLD 4 (34.7%), closely followed by GOLD 3 (32.1%) and GOLD 2 (28.4%). The number of exacerbations during the last year ranged from zero to 12, while about one third of the patients had more than two exacerbations (65 patients, 34.3%). An even greater range was found in the number of doctor visits during the last year. The number ranged from zero to 52 (one a week), while nearly one fifth visited the doctor 10 times or more last year due to COPD problems. About one third of COPD patients were in an outpatient treatment at time of enrolment. Concerning the patients’ total number of prescribed medications, the variation was between one and 17 different medications, while the median number was 7. Just less than half of the patients had an inconspicuous score in the HADS-A score. The same goes for the depression score of the HADS, indicating that more than half of the patients reported symptoms of depression. The mean value of the physical and mental component scale was 31.8 and 38.0, respectively. Characteristics of the study population are displayed in Table 1.
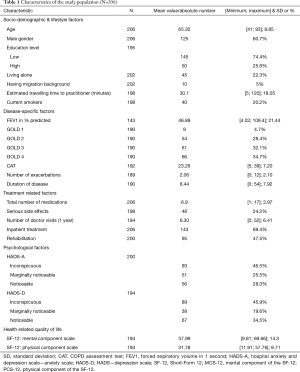
Full table
Univariate analysis
In total, 194 patients could be included in univariate regression analysis. As shown in Table 2, mainly disease-related, treatment-related and psychological factors were univariately associated with both component scales of the SF-12. Regarding socio-demographic factors, only female gender and migration background play a nearly significant or significant role in MCS-12 or PCS-12, respectively. Furthermore, the CAT score, the number of exacerbations during the last year, the total number of prescribed medications and reporting symptoms of depression or anxiety show a significant negative association with both scale scores of the SF-12. The FEV1 value in percent predicted was positively associated with both scores, PCS-12 and MCS-12. Having taken part in a rehabilitation measure was associated with a significantly lower PCS score. The same is true for ever having experienced serious side effects due to medications taken for COPD treatment (Table 2).
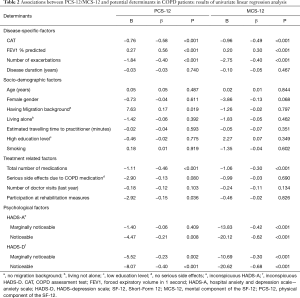
Full table
Multivariable analysis
The multivariable model was built of variables which showed significant associations with HRQOL in univariate analysis. Looking at the final model, PCS-12 score showed a significant negative association with the CAT score. Furthermore, a higher total number of medications prescribed was significantly associated with PCS-12 score in a negative way. A higher FEV1 value in percent predicted was significantly related to PCS-12 score in a positive manner. These variables explained 57% of the variance in the PCS-12 variable in the final multivariable model.
Like with PCS-12, having a higher CAT score was associated with a significantly lower MCS-12 score. In contrast to PCS-12, MCS-12 score was significantly associated with elevated patient-reported symptoms of anxiety or depression in a negative way. More precisely, even reporting marginally noticeable symptoms of anxiety as well as reporting noticeable symptoms of anxiety or depression were associated with a reduced mental HRQOL. In total, 54% of the variance in the MCS-12 variable was explained by the just named variables (Table 3).
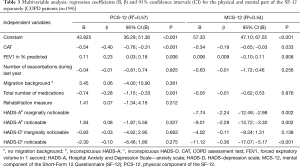
Full table
Sensitivity analyses were performed in order to investigate whether association patterns would differ between patients recruited from primary vs. secondary care. CAT score and FEV1 (in percent predicted) emerged as the strongest predictive factors in both subsamples and were, significantly related to PCS-12 score in both groups. For MCS-12 score, a noticeable HADS-D remained the factor most strongly associated in both groups (data not shown).
Discussion
Principal findings
This cross-sectional study, investigating determinants of generic HRQOL in COPD patients, indicates a lower PCS-12 score and MCS-12 score in COPD patients compared to the German norm population (31). Regarding significant determinants, the CAT score was the only factor associated with both the physical and mental component of the SF-12. Lung function and total number of medications, both of which reflect disease severity, were related to worse physical HRQOL. Reporting symptoms of anxiety or depression show the strongest associations with MCS-12 score.
Disease-specific factors
CAT
The CAT has been developed as simple and reliable measure of health status in COPD patients (24) and can therefore be considered as a measure of COPD specific QOL. As far as we know the relationship of CAT with generic HRQOL has not been investigated before. If one takes a closer look at the content of the CAT, it becomes apparent that it enquires about symptoms (cough, phlegm/mucus, chest tightness, dyspnea) and functional limitations (sleep disorders, domestic work, energy, confident leaving home). Therefore, an association with physical HRQOL was to be expected. However, the finding of a significant negative association between CAT and mental HRQOL is noteworthy and moreover the only significant relationship besides the association between MCS-12 score with psychological factors.
FEV1
FEV1 is the most commonly used way to express functional impairment. Although it is quite difficult to compare or summarize results, due to heterogeneity in outcome measures and instruments used, our results are comparable to previous studies (32). According to results of Garrido et al., who found a higher correlation between FEV1 and PCS-12 score (20), predicted FEV1% was only significantly associated with PCS-12 score in the multivariable analysis of this study. Bentsen et al. demonstrated that subjective health status in COPD patients is determined more by symptoms, particular breathlessness as well as anxiety and depression, than demographics or physiological variables like predicted FEV1% (33). In a study of Janson et al. (13) lower FEV1 was associated with a lower PCS-12 score, but there was no significant association between FEV1 and the mental part of QOL. The strong association in our univariate analysis is possibly explainable by the high number of severe and even very severe COPD patients in our study population. Often patients with COPD stage IV are underrepresented in studies due to time consuming test batteries which impose a burden to patients. In a study of Pereira et al. (34) 57.1% of patients were classified as having severe or extremely severe COPD. In this study, FEV1 was the parameter that best correlated with the St Georges Respiratory Questionnaire (SGRQ), another disease-specific measure of HRQOL for chronic respiratory illness, total score and the only respiratory function parameter that correlated with PCS-36 score.
Treatment related factors
In our study, poorer physical HRQOL was associated with a higher number of total medications in multivariable analysis. In reviewing the literature, a study with 611 COPD patients (43.7% with COPD GOLD III) found that patients who took two or more medications to treat their COPD compared to patients without any medication had a clinically relevant decrease in their HRQOL measured with SGRQ (35). Furthermore, Miravitlles et al. showed in a cross-sectional study with 441 COPD patients, that the PCS-12 score was significantly associated with the number of different drugs (36). Since in our study no differentiation was made between medications for treating COPD and other medications, a direct comparison with these studies is not possible. However, a similar trend can be observed. Since there is only a significant association with the physical QOL, the total number of medications taken could potentially represent a proxy measure for the number of comorbidities.
Psychological factors
In this study, about one third of the patients reported a noticeable amount of depressive symptoms and about 20% were grouped as having marginally noticeable depressive symptoms. Having marginally noticeable symptoms of anxiety is true for about 25% in our study. Our finding is comparable to the prevalence of clinically significant depressive symptoms in COPD patients revealed in a meta-analysis study by Zhang et al. (37). Together HADS-A and HADS-D explain the majority of variance in the mental component of HRQOL in our study. In contrast to the significantly negative associations between HADS and MCS-12 score, our study found no association between the different categories of the HADS and the physical component of the SF-12 questionnaire. A review and meta-analysis of Tsiligianni et al. (7) has shown a persisting association between depression or rather anxiety with QOL, when using different questionnaires. Looking at the SF-36, the long form of the SF-12 questionnaire used in our study, a cross-sectional study revealed that COPD patients without significant depressive symptoms had significantly higher scores in all sub-scales of the SF-36 compared to those with depressive symptoms (38). Even across multiple study designs the relationship between anxiety and depression with HRQOL remains the same (39). Moreover, when depression and anxiety are considered as comorbidities, a strong association with HRQOL can be found in literature (18). A clear association between depressive or anxious symptoms and HRQOL can therefore be assumed. However, it has to be noted, that both HADS and MCS-12 tap into related constructs which means that a correlation can be expected to some extent.
Strengths and weaknesses
To interpret the findings of the study correctly, some limitations should be acknowledged. Due to the cross-sectional design of our study, no causal relationships could be revealed as we are unable to disentangle the time sequence of events. Furthermore, HRQOL was obtained as a self-reported outcome, which means that for example daily sensitivities like stress or bad mood may influence the answers as there are included retrospective questions. However, self-reported outcome measures are considered important measuring tools in clinical research when it comes to HRQOL (40). Even if there was no random selection of participating physicians, we aimed to cover a wide range of different recruitment sites in order to get a most generalizable COPD population. Despite the attempt we made to recruit a broad range of severities from different recruitment sites, we did end up with a sample that has a higher proportion of severe and very severe stages of COPD compared to the general COPD population in Europe (41). A further strength is the broad approach with different spheres of influence analyzed, as living with COPD is complex and there are various domains that possibly affect HRQOL. Furthermore, the use of standardized and validated measurement instruments for our main outcome and most of our independent variables is a strength of our study.
Conclusions
Depending on the component of QOL, HRQOL is associated with a number of factors. The strongest of which are COPD-specific HRQOL for generic physical HRQOL and reporting symptoms of depression and/or anxiety for generic mental HRQOL. In clinical practice screening for depression and anxiety and referring potentially affected patients to psychiatric assessment may be promising approaches to enhance the QOL of COPD patients. Furthermore, the conduct of robust interventional studies is warranted.
Acknowledgements
We would like to thank the physicians who facilitated recruitment of patients for this study (Frank Heinemann, Sigrid Karrer, Christof Kundel, Jürgen Pahnke, Markus Reuter, Wolfgang Sieber, Rupert Zach) as well as all participating patients. We also thank Susanne Hammer, Florian Herl and Ursula Zach for their valuable help in patient recruitment and data entry. The study was funded by internal funds of the Medical Sociology unit as well as the funds provided by the Faculty of Medicine of the University of Regensburg (ReForM-A), earned by S Brandstetter.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: Prior to the investigation, ethical clearance was obtained from the local ethics committee on 16 May 2013 (reference number: 13-101-0091). Informed consent was obtained from all individual participants included in the study.
References
- OECDLibrary. Health at a Glance: Europe 2012. Available online: http://www.oecd-ilibrary.org/sites/9789264183896-en/01/16/index.html?itemId=/content/chapter/9789264183896-19-en
- Geldmacher H, Biller H, Herbst A, et al. The prevalence of chronic obstructive pulmonary disease (COPD) in Germany. Results of the BOLD study. Dtsch Med Wochenschr 2008;133:2609-14. [Crossref] [PubMed]
- World Health Organization. The top 10 causes of death. Availbale online: http://www.who.int/mediacentre/factsheets/fs310/en/
- GOLD. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease 2015. Available online: http://goldcopd.org/global-strategy-diagnosis-management-prevention-copd-2016/
- Teschler H, Seeger W, Vogelmeier C. The position of respiratory medicine in Germany: status quo and future outlook. Pneumologie 2010;64:143-8. [Crossref] [PubMed]
- Ruff LK, Volmer T, Nowak D, et al. The economic impact of smoking in Germany. Eur Respir J 2000;16:385-90. [Crossref] [PubMed]
- Tsiligianni I, Kocks J, Tzanakis N, et al. Factors that influence disease-specific quality of life or health status in patients with COPD: a review and meta-analysis of Pearson correlations. Prim Care Respir J 2011;20:257-68. [Crossref] [PubMed]
- Hesselink AE, van der Windt DA, Penninx BW, et al. What predicts change in pulmonary function and quality of life in asthma or COPD? J Asthma 2006;43:513-9. [Crossref] [PubMed]
- Wijnhoven HA, Kriegsman DM, Hesselink AE, et al. Determinants of different dimensions of disease severity in asthma and copd*: Pulmonary function and health-related quality of life. Chest 2001;119:1034-42. [Crossref] [PubMed]
- Ferrer M, Alonso J, Morera J, et al. Chronic Obstructive Pulmonary Disease Stage and Health-Related Quality of Life. The Quality of Life of Chronic Obstructive Pulmonary Disease Study Group. Ann Intern Med 1997;127:1072-9. [Crossref] [PubMed]
- Weldam SW, Schuurmans MJ, Liu R, et al. Evaluation of Quality of Life instruments for use in COPD care and research: a systematic review. Int J Nurs Stud 2013;50:688-707. [Crossref] [PubMed]
- Ware J Jr, Kosinski M, Keller SD. A. 12-Item Short-Form Health Survey: construction of scales and preliminary tests of reliability and validity. Med Care 1996;34:220-33. [Crossref] [PubMed]
- Janson C, Marks G, Buist S, et al. The impact of COPD on health status: findings from the BOLD study. Eur Respir J 2013;42:1472-83. [Crossref] [PubMed]
- Wacker ME, Hunger M, Karrasch S, et al. Health-related quality of life and chronic obstructive pulmonary disease in early stages - longitudinal results from the population-based KORA cohort in a working age population. BMC Pulm Med 2014;14:134. [Crossref] [PubMed]
- Vogelmeier C, Buhl R, Criée CP, et al. Guidelines for the diagnosis and therapy of COPD issued by Deutsche Atemwegsliga and Deutsche Gesellschaft fur Pneumologie und Beatmungsmedizin. Pneumologie 2007;61:e1-40. [Crossref] [PubMed]
- Wijnhoven HA, Kriegsman DM, Hesselink AE, et al. The influence of co-morbidity on health-related quality of life in asthma and COPD patients. Respir Med 2003;97:468-75. [Crossref] [PubMed]
- Moy ML, Reilly JJ, Ries AL, et al. Multivariate models of determinants of health-related quality of life in severe chronic obstructive pulmonary disease. J Rehabil Res Dev 2009;46:643-54. [Crossref] [PubMed]
- Huber MB, Wacker ME, Vogelmeier CF, et al. Comorbid Influences on Generic Health-Related Quality of Life in COPD: A Systematic Review. PLoS One 2015;10:e0132670. [Crossref] [PubMed]
- Voll-Aanerud M, Eagan TM, Wentzel-Larsen T, et al. Respiratory symptoms, COPD severity, and health related quality of life in a general population sample. Respir Med 2008;102:399-406. [Crossref] [PubMed]
- Carrasco Garrido P, de Miguel Díez J, Rejas Gutiérrez J. Negative impact of chronic obstructive pulmonary disease on the health-related quality of life of patients. Results of the EPIDEPOC study. Health Qual Life Outcomes 2006;4:31. [Crossref] [PubMed]
- Sundh J, Johansson G, Larsson K, et al. Comorbidity and health-related quality of life in patients with severe chronic obstructive pulmonary disease attending Swedish secondary care units. Int J Chron Obstruct Pulmon Dis 2015;10:173-83. [Crossref] [PubMed]
- Böhmer MM, Brandl M, Brandstetter S, et al. Factors associated with generic health-related quality of life in adult asthma patients in Germany: Cross-sectional study. J Asthma 2017;54:325-34. [Crossref] [PubMed]
- Bullinger M, Kirchberger I, Ware J. Der deutsche SF-36 Health Survey Übersetzung und psychometrische Testung eines krankheitsübergreifenden Instruments zur Erfassung der gesundheitsbezogenen Lebensqualität. J Public Health 1995;3:21-36. [Crossref]
- Jones PW, Harding G, Berry P, et al. Development and first validation of the COPD Assessment Test. Eur Respir J 2009;34:648-54. [Crossref] [PubMed]
- Jones P, Harding G, Wiklund I, et al. Improving the process and outcome of care in COPD: development of a standardised assessment tool. Prim Care Respir J 2009;18:208-15. [Crossref] [PubMed]
- Jones P, Jenkins C, Bauerle O. CAT. Expert Guidance on frequently asked questions. GlaxoSmithKline 2012.
- Miravitlles M, Ferrer M, Pont À, et al. Effect of exacerbations on quality of life in patients with chronic obstructive pulmonary disease: a 2 year follow up study. Thorax 2004;59:387-95. [Crossref] [PubMed]
- Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand 1983;67:361-70. [Crossref] [PubMed]
- Herrmann C, Buss U, Snaith RP. HADS-D: Hospital anxiety and depression scale-deutsche version; Ein Fragebogen zur Erfassung von Angst und Depressivität in der somatischen Medizin. Bern: Hans-Huber-Verlag, 1995.
- Hinz A, Schwarz R. Anxiety and depression in the general population: normal values in the Hospital Anxiety and Depression Scale. Psychother Psychosom Med Psychol 2001;51:193-200. [Crossref] [PubMed]
- Bullinger M, Kirchberger I. SF-36 Fragebogen zum Gesundheitszustand. Göttingen: Hogrefe, 1998.
- Curtis JR, Deyo RA, Hudson LD. Pulmonary rehabilitation in chronic respiratory insufficiency. 7. Health-related quality of life among patients with chronic obstructive pulmonary disease. Thorax 1994;49:162-70. [Crossref] [PubMed]
- Bentsen SB, Henriksen AH, Wentzel-Larsen T, et al. What determines subjective health status in patients with chronic obstructive pulmonary disease: importance of symptoms in subjective health status of COPD patients. Health Qual Life Outcomes 2008;6:115. [Crossref] [PubMed]
- Pereira ED, Pinto R, Alcantara M, et al. Influence of respiratory function parameters on the quality of life of COPD patients. J Bras Pneumol 2009;35:730-6. [Crossref] [PubMed]
- Esteban C, Moraza J, Quintana JM, et al. Use of medication and quality of life among patients with COPD. Respir Med 2006;100:487-95. [Crossref] [PubMed]
- Miravitlles M, Alvarez-Sala JL, Lamarca R, et al. Treatment and quality of life in patients with chronic obstructive pulmonary disease. Qual Life Res 2002;11:329-38. [Crossref] [PubMed]
- Zhang MW, Ho RC, Cheung MW, et al. Prevalence of depressive symptoms in patients with chronic obstructive pulmonary disease: a systematic review, meta-analysis and meta-regression. Gen Hosp Psychiatry 2011;33:217-23. [Crossref] [PubMed]
- Felker B, Katon W, Hedrick SC, et al. The association between depressive symptoms and health status in patients with chronic pulmonary disease1. General Hospital Psychiatry 2001;23:56-61. [Crossref] [PubMed]
- Blakemore A, Dickens C, Guthrie E, et al. Depression and anxiety predict health-related quality of life in chronic obstructive pulmonary disease: systematic review and meta-analysis. Int J Chron Obstruct Pulmon Dis 2014;9:501-12. [Crossref] [PubMed]
- Deshpande PR, Rajan S, Sudeepthi BL, et al. Patient-reported outcomes: A new era in clinical research. Perspect Clin Res 2011;2:137-44. [Crossref] [PubMed]
- Jones PW, Brusselle G, Dal Negro RW, et al. Health-related quality of life in patients by COPD severity within primary care in Europe. Respir Med 2011;105:57-66. [Crossref] [PubMed]


