Correlative factors for the location of tracheobronchial foreign bodies in infants and children
Introduction
Tracheobronchial foreign body is one of the most common critical diseases in otolaryngology-head and neck surgery. Due to anatomy, physiology, eating habits, infant curiosity and other factors, tracheobronchial foreign body mostly occurs in 1–3-year-old infants; and the complication rate and mortality are relatively high (1-4). The severity depends largely on the nature of the foreign body and the degree of obstruction determined by the location of the foreign body. The complete blockage of the larynx or trachea by foreign bodies is the main cause of death in infants below three years of age. When the foreign body is located in the left and right principal bronchi and the next lower level bronchi, it can lead to repeated pneumonia, emphysema, atelectasis, or even death (5). Previous studies on tracheobronchial foreign bodies have mostly focused on the description of the age, gender, nature of the foreign body, diagnosis and treatment (6-10). However, few studies were conducted on the association of the location of the foreign body with age, gender, operation time and length of hospital stay. In the present study, factors related to the location of foreign bodies were investigated and studied to provide help in the diagnosis of diseases and related complications, the timing of operation, and the evaluation of the operation risk and prognosis.
Methods
Clinical data
The clinical data of 1,060 infants and children, who were diagnosed with tracheobronchial foreign bodies and underwent rigid bronchoscopy in Nanjing Children’s Hospital Affiliated to Nanjing Medical University from January 2015 to December 2015, were retrospectively analyzed. Inclusion criteria: (I) infants and children with or without a definite history of foreign body cough; (II) subjects with clinical manifestations of cough, asthma, fever and dyspnea; (III) pulmonary auscultation reveals weakened unilateral respiratory sounds, coarse double lung respiratory sounds, wheezing sounds, and dry or moist rales; (IV) chest CT reveals emphysema, atelectasis and pneumonia; (V) tracheobronchial 3D reconstruction reveals an obstructed shadow of the foreign body in the airway. Exclusion criteria: (I) patients who were able to spontaneously coughed out the foreign body after hospitalization; (II) patients with a history of asthma or acute infection of the superior respiratory tract; (III) patients with foreign bodies that could not be removed under a rigid bronchoscope, and needs to be transferred to other departments for treatment. A correlation analysis was performed according to age, gender, chest CT and 3D reconstruction and complications, the location of the foreign body (the location of the foreign body revealed by imaging and bronchoscopic findings), treatment outcome, and length of hospital stay. This study was conducted with approval from the Ethics Committee of our hospital. This study was conducted in accordance with the declaration of Helsinki.
Therapeutic methods
Patients underwent bronchoscopy and the removal of the foreign body under general anesthesia within 24 hours after admission. Combined intravenous anesthesia: intravenous injections of 0.1 mg/kg of midazolam (batch number: 20130480, Jiangsu Nhwa Pharmaceutical Co., Ltd., Xuzhou, China), 0.3 mg/kg of dexamethasone (batch number: 1208176412, Shandong Chenxin Pharmaceutical Co., Ltd., Jining, China), and 2 mg/kg of propofol (batch number: KA500, AstraZeneca, Basilico, Italy) were successively performed. After 30 seconds, 3 µg/kg of fentanyl (batch number: 2121130, Hubei Yichang human well Pharmaceutical Co., Ltd., Yichang, China) was slowly intravenously injected (the injection was completed at 60 seconds, and the spontaneous breathing of the patient was maintained), and 100 µg·kg−1min−1 of propofol was used for maintenance. After 4–6 minutes, the epiglottis was stirred up with an anesthetic laryngoscope, 1% lidocaine hydrochloride (batch number: 7A99J1, China Otsuka Pharmaceutical Co, Ltd., Tianjin, China) was inhaled in the trachea with respiratory for full surface anesthesia of the trachea. Then, after 8 minutes, the operation was begun.
Surgical methods: A rigid bronchoscope was inserted through the throat (the bronchoscope was any type of STORZE (Germany), and the corresponding size of the bronchoscope was chosen according to the age of the child). The bronchoscope was entered into the trachea and bronchus to remove the foreign bodies. Granulation was removed when found. If the foreign body was broken or the mucous membrane bled, alveolar lavage was performed with 2 mL of 1% lidocaine hydrochloride solution containing 1:100,000 epinephrine hydrochloride (batch number: 1606161, Zhucheng Pharmaceutical Co. Ltd., Zhengzhou, China). After 30 seconds, the lavage fluid was sucked out using 50–70 mmHg of negative pressure, and rinsing was repeated until the tracheobronchial lumen was unobstructed. Routine electrocardiogram and blood oxygen saturation were monitored during the operation. Routine intravenous administration, as well as nebulized inhalation of antibiotics and hormone, was given after the operation. Chest fluoroscopy was performed at three days after the operation. If no obvious abnormality was found, the patient was discharged.
Statistical analysis
Data were statistically analyzed using statistical software SPSS19.0. The rank correlation coefficient was used to describe the association between two quantitative variables, or between a quantitative and categorical variable, which were not normally distributed. For the association analysis of two categorical variables with at least one variable as an unordered categorical variable, the independence of two attributes was first evaluated using χ2-test, according to the contingency tables obtained by cross classification and counting (if these could not be evaluated using χ2-test, Fisher’s exact probability test was used). Then, the correlation coefficient was calculated. In the present study, the inspection level was α=0.05.
Results
The correlation between the location of the foreign bodies with age, operation time, and length of hospital stay
Rank correlation analysis revealed that the location of the foreign bodies was not correlated with age, operation time and length of hospital stay (P>0.05, Table 1).

Full table
The correlation between the location of foreign bodies and gender
χ2-test revealed that the difference in the location of foreign bodies between two genders was not statistically significant at an inspection level of α=0.05 (χ2=6.537, P=0.088). Furthermore, it could not be considered that the location of the foreign body was related to gender (Table 2).

Full table
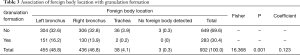
Correlations between the location of the foreign body and granulation formation
Fisher’s exact probability test revealed that the difference in the location of foreign bodies between the presence and absence of granulation formation was statistically significant at an inspection level of α=0.05 (Fisher =16.368, P=0.001), and the coefficient of contingency was 0.123. This indicate that the location of the foreign body was lowly correlated to granulation formation (Table 3).
Full table
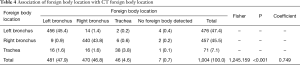
Correlations between the location of the foreign body and the location of foreign bodies displayed by chest CT
The difference in the actual location of the foreign bodies among the locations of foreign bodies displayed by CT was statistically significant at an inspection level of α=0.05 (Fisher =1,245.159, P<0.001), and the coefficient of contingency was 0.749. Furthermore, this indicates that the location of the foreign body was highly related to the location of the foreign body displayed by chest CT (Table 4).
Full table
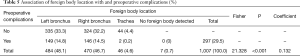
Correlations between the location of the foreign body and preoperative complications
The difference in the location of foreign bodies based on the presence of preoperative complications was statistically significant at an inspection level of α=0.05 (Fisher =21.328, P<0.001), and the coefficient of contingency was 0.132. This indicates that the location of the foreign body was lowly correlated to preoperative complications (Table 5).
Full table
Discussion
Tracheobronchial foreign body is one of the most common critical diseases in otolaryngology-head and neck surgery in a children’s hospital, which often occurs in 1–3 years old infants. This requires doctors in otolaryngology-head and neck surgery to provide the timely and accurate diagnosis and treatment of tracheobronchial foreign bodies. Bronchoscopy under general anesthesia is the gold standard for the diagnosis of tracheobronchial foreign bodies. Furthermore, history of foreign body cough, asymmetry of lung auscultation and chest imaging examination are the common clinical diagnostic bases, which play extremely important roles in the clinical diagnosis of tracheobronchial foreign bodies.
In the present study, 1,060 infants and children with tracheobronchial foreign bodies were studied. Results revealed that tracheobronchial foreign bodies accounted for 92.5% in 0–3-year-old infants, 64.3% in male patients, and 88.9% in patients with plant foreign bodies. This is consistent with the results of previous reports (11-13). In the present experiment, 1,060 infants and children who underwent bronchoscopy were studied. Results revealed that the location of the foreign bodies was not correlated with age, gender, operation time and length of hospital stay. Johnson et al. (14) reported that the location of foreign bodies changed with the age of the children, and affected mechanical ventilation and hospital mortality. The reason may be that in their study, the age of the children was 0–17 years old, and the foreign bodies were located in the larynx, trachea, bronchus and secondary bronchus. In the present study, among the 1,060 infants and children, the minimum age was 6 months, the maximum age was nine years and 11 months old, and the main locations of the foreign bodies were the trachea and left and right bronchi. The reason may be the differences in living habits and environment in different regions. On the other hand, the common complication of tracheobronchial foreign bodies is granulation formation; particularly, plant foreign bodies that are rich in oil are more likely to induce granulation. Previous literatures have provided various reports on risk factors for granulation formation (15,16). However, there has been no report on the correlation between granulation formation and the location of foreign bodies. The present study revealed that the difference in the location of foreign bodies detected by bronchoscopy between the presence and absence of granulation formation was statistically significant at an inspection level of α=0.05 (Fisher =16.368, P=0.001), and the coefficient of contingency was 0.123. This indicates that the location of the foreign body was lowly correlated to granulation formation, and the incidence of granulation was higher in patients with bronchial foreign bodies than in patients with tracheal foreign bodies.
Imaging examination, especially chest CT and 3D reconstruction, is essential to patients with tracheobronchial foreign bodies. The present study revealed that the coefficient of contingency between the location of the foreign body under a bronchoscope and the location of the foreign body revealed by CT was 0.749 (P<0.001). This indicates that the location of the foreign body under a bronchoscope was highly correlated to the location of the foreign body detected by chest CT and 3D reconstruction. Previous studies have revealed that the sensitivity and specificity of chest CT in the diagnosis of tracheobronchial foreign bodies were higher than those of X-ray chest films (17,18). Chest CT and 3D reconstruction can be used for the diagnosis of tracheobronchial foreign bodies in children: (I) the presence of any tracheobronchial foreign body; (II) the determination of whether the foreign body blocked the airway, whether atelectasis occurred in case of complete obstruction, and whether distal pulmonary emphysema was induced by the valve mechanism in case of incomplete obstruction; (III) the determination of whether pneumonia occurred; (IV) the determination of whether complications such as subcutaneous emphysema, mediastinal emphysema and pneumothorax occurred; (V) the determination of whether the child has any foreign body or related complications, who has no significant history of foreign body, and has suspected symptoms and signs for foreign bodies. In summary, the correlation of the location of foreign bodies with chest CT and 3D reconstruction revealed that the high correlation between the locations of foreign bodies suggests that clinicians should put importance to the use of CT, which is helpful for the accurate diagnosis of the disease, ensuring the safety of the patient.
Common complications of tracheobronchial foreign bodies include pneumonia, emphysema, atelectasis and bronchiectasis. When severe, it leads to asphyxiation and death; and the most common complication in infants is emphysema (19). The present study revealed that the coefficient of contingency between the location of the foreign body under a bronchoscope and preoperative complications was 0.132 (P<0.001). This indicates that the location of the foreign body was lowly correlated to preoperative complications. Understanding of the condition and preoperative complications of children is propitious to reducing operative complications and mortality, through the intraoperative cooperation with the anesthesiologist (20).
In summary, the location of foreign bodies was not correlated with age, gender, operation time and length of hospital stay, but was associated with granulation formation, thoracic computed tomography and three-dimensional reconstruction results, and preoperative complications.
Acknowledgements
We are particularly grateful to all the people who have given us help on our article.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: This study was conducted with approval from the Ethics Committee of our hospital (No. 201601001-1). This study was conducted in accordance with the declaration of Helsinki.
References
- Altuntas B, Aydın Y, Eroglu A. Foreign Bodies in Trachea: A 25-years of Experience. Eurasian J Med 2016;48:119-23. [Crossref] [PubMed]
- Saki N, Nikakhlagh S, Heshmati SM. 25-Year Review of the Abundance and Diversity of Radiopaque Airway Foreign Bodies in Children. Indian J Otolaryngol Head Neck Surg 2015;67:261-6. [Crossref] [PubMed]
- Ciftci AO, Bingöl-Koloğlu M, Senocak ME, et al. Bronchoscopy for evaluation of foreign body aspiration in children. J Pediatr Surg 2003;38:1170-6. [Crossref] [PubMed]
- Sumanth TJ, Bokare BD, Mahore DM, et al. Management of tracheobronchial foreign bodies: a retrospective and prospective study. Indian J Otolaryngol Head Neck Surg 2014;66:60-4. [Crossref] [PubMed]
- Skoulakis CE, Doxas PG, Papadakis CE, et al. Bronchoscopy for foreign body removal in children. A review and analysis of 210 cases. Int J Pediatr Otorhinolaryngol 2000;53:143-8. [Crossref] [PubMed]
- Gvetadze P, Chkhaidze I, Baldas S, et al. Injuries due to foreign body aspirations in Georgia: A prevention perspective. Int J Pediatr Otorhinolaryngol 2016;83:84-7. [Crossref] [PubMed]
- Naragund AI, Mudhol RS, Harugop AS, et al. Tracheo-bronchial foreign body aspiration in children: a one year descriptive study. Indian J Otolaryngol Head Neck Surg 2014;66:180-5. [Crossref] [PubMed]
- Saki N, Nikakhlagh S, Rahim F, et al. Foreign body aspirations in infancy: a 20-year experience. Int J Med Sci 2009;6:322-8. [Crossref] [PubMed]
- Liang J, Hu J, Chang H, et al. Tracheobronchial foreign bodies in children-a retrospective study of 2,000 cases in Northwestern China. Ther Clin Risk Manag 2015;11:1291-5. [PubMed]
- Haddadi S, Marzban S, Nemati S, et al. Tracheobronchial Foreign-Bodies in Children; A 7 Year Retrospective Study. Iran J Otorhinolaryngol 2015;27:377-85. [PubMed]
- Aydoğan LB, Tuncer U, Soylu L, et al. Rigid bronchoscopy for the suspicion of foreign body in the airway. Int J Pediatr Otorhinolaryngol 2006;70:823-8. [Crossref] [PubMed]
- Mansour B, Elias N. Foreign Body Aspiration in Children with Focus on the Role of Flexible Bronchoscopy: A 5 Year Experience. Isr Med Assoc J 2015;17:599-603. [PubMed]
- Foltran F, Ballali S, Passali FM, et al. Foreign bodies in the airways: a meta-analysis of published papers. Int J Pediatr Otorhinolaryngol 2012;76:S12-9. [Crossref] [PubMed]
- Johnson K, Linnaus M, Notrica D. Airway foreign bodies in pediatric patients:anatomic location of foreign body affects complications and outcomes. Pediatr Surg Int 2017;33:59-64. [Crossref] [PubMed]
- Huang Z, Zhou A, Zhang J, et al. Risk factors for granuloma formation in children induced induced by tracheobronchial foreign bodies. Int J Pediatr Otorhinolaryngol 2015;79:2394-7. [Crossref] [PubMed]
- Barbato A, Novello A Jr, Tormena F, et al. Problems with the retrieval of long-standing inhaled foreign bodies in children. Monaldi Arch Chest Dis 1996;51:419-20. [PubMed]
- Sattar A, Ahmad I, Javed AM, et al. Diagnostic accuracy of chest x-ray in tracheobronchial foreign body aspiration in paediatricpatients. J Ayub Med Coll Abbottabad 2011;23:103-5. [PubMed]
- Pugmire BS, Lim R, Avery LL. Review of Ingested and Aspirated Foreign Bodies in Children and Their Clinical Significance for Radiologists. Radiographics 2015;35:1528-38. [Crossref] [PubMed]
- Yang YH, Zhang XG, Zhang JL, et al. Risk factors for preoperative respiratory complications in children with tracheobronchial foreign bodies. J Int Med Res 2016;44:338-45. [Crossref] [PubMed]
- Buu NT, Ansermino M. Anesthesia for removal of inhaled foreign bodies in children. Paediatr Anaesth 2005;15:533-5. [Crossref] [PubMed]


