Renal denervation therapy beyond resistant hypertension
The scope of the problem
It is estimated that over one billion people worldwide are affected by hypertension (HTN) and that over nine million annual deaths can be attributed to complications of HTN such as myocardial infarction, stroke and renal disease. The prevalence of HTN is constantly rising and this trend is expected to continue unless appropriate measures are taken (1,2). Importantly, even very mild reductions in blood pressure were linked to a large effect on rates of cardiovascular events (3,4).
Definitions of HTN
Recently published American guidelines (5) categorize HTN into four levels according to an average of two office measurements: (I) normal: systolic blood pressure (SBP) <120 mmHg and diastolic blood pressure (DBP) <80 mmHg; (II) elevated: SBP 120–129 mmHg and DBP <80 mmHg; (III) HTN stage 1: SBP 130–139 mmHg or DBP 80–89 mmHg; and (IV) HTN stage 2: SBP ≥140 mmHg or DBP ≥90 mmHg. This new categorization is in agreement with recently published data which has shown that lower cut offs for defining HTN and its treatment are beneficial (6). Often, office BP measurements are higher than those measured out of the office, and this phenomenon has been defined as “white coat HTN”. Population-based studies have shown that the prevalence of white coat HTN may be as high as 16% and ranging from 35% to 46% among hypertensive patients (7,8). The clinical importance of isolated white coat HTN is still under debate since some studies have found these patients to have higher cardiovascular risk when compared to normotensives, while others have failed to demonstrate this association (9). Yet, 24 hours average measurements have consistently shown to better correlate with morbidity and mortality than office BP measurements (10,11). Most trials focused on white coat HTN have used a cut-off of 135/85 mmHg for out of office or 130/80 mmHg for 24-hour ambulatory BP monitor (ABPM) measurements and therefore have a slightly different definition of HTN.
Is pharmacotherapy really failing?
Since pharmacotherapy for HTN had been proven to be efficacious in numerous trials, the growing prevalence of HTN may be explained in several ways: (I) ageing of population; (II) lack of public health policies and their implementation, especially in low and mid income countries (1) leading to under-diagnosis of HTN and thus delayed treatment; (III) non-adherence to therapy; (IV) resistant HTN. The first two are out of our intended scope. Non-adherence to anti-hypertensive therapy is very common, yet it is difficult to detect and it varies over time (12). While good adherence is associated with reduced risk of cardiovascular events (13), it is estimated that up to 50% of patients become non-adherent within 1 year of initial drug therapy (14). The European Society of Cardiology guidelines define “resistant HTN” when a therapeutic strategy that includes appropriate lifestyle measures plus a diuretic and two other antihypertensive drugs belonging to different classes at adequate doses fail to lower SBP to <140 mmHg and DBP values to <90 mmHg, respectively (15). Recent American guidelines define HTN as “resistant” when a patient is treated with 3 antihypertensive medications with complimentary mechanisms (one of which a diuretic) an fail to achieve control or when control is achieved but under treatment of at least 4 different medications (5). The prevalence of resistant HTN is estimated to be less than 10% of the overall hypertensive population. It is important to differentiate true resistant HTN from apparent ones such as in cases of isolated office HTN, non-adherence and sub-optimal medical regiments since true resistant HTN is associated with a higher risk of cardiovascular and renal disease (16).
The sympathetic nervous system and the rationale for renal denervation (RDN)
In the early 20th century, the medical community started to learn about the effect of the sympathetic nervous system on BP. From the 1920s onto the 1950s, patients with severe HTN were treated with splanchnicectomy, the surgical division of the thoracic and lumbar ganglia. This treatment, although quite effective in lowering BP, was associated with relatively high perioperative morbidity and severe side effects and was subsequently relinquished with the advent of hypertensive medications. However, it provided the basis for future research and therapeutic procedures.
The kidneys are innervated by efferent sympathetic nerves from the central nervous system and by afferent sympathetic sensory nerves from the kidneys to the hypothalamus. Efferent sympathetic activity has three major effects on the kidney: (I) increased renin secretion; (II) increased sodium reabsorption in the tubules; and (III) decreased blood flow to the kidneys. Together, all these mechanisms contribute to elevation of BP. The afferent nerves respond to renal injury and ultimately cause an increase in central sympathetic outflow as well. In untreated hypertensive patients, a high level of sympathetic activation had been demonstrated. Thus, uncontrolled activation of the renal sympathetic nerves seems to play a role in the pathophysiology of essential HTN (17,18) and therefore, decreasing the sympathetic outflow to the kidneys may potentially be associated with a decrease in systemic BP. From an anatomical stand point, the renal sympathetic nerves originate in the sympathetic chain and in ganglia surrounding the aorta and proximal renal arteries, whereupon they form a plexus surrounding the mid and distal parts of the renal arteries which runs in parallel to the renal arteries through the outer adventitia (19). These factors, the role of the renal sympathetic outflow in the development of HTN, the anatomy of the renal sympathetic nerves and their proximity to the renal arteries, and finally, the unmet need for a new therapeutic option in the context of low adherence to medications as well as resistant HTN had led to the development and design of radiofrequency-based ablation catheters for RDN.
RDN trials: lessons learned were not a simplicity
The Symplicity HTN-1 was the first-in-man trial published in 2009. In this proof-of-concept trial, RDN therapy had been used amongst resistant HTN patients who were selected due to the potential clinical benefit (20). Later on, the Symplicity HTN-2 was a randomized-controlled, multi-center trial that enrolled 106 patients with resistant HTN and randomized them to RDN therapy plus medical management vs. medical management alone. Patients with hemodynamically significant renal artery stenosis, previous renal artery intervention, kidney dysfunction with estimated glomerular filtration rate (eGFR) <45 mL/min/1.73 m2, type-1 diabetes mellitus or renal artery anatomy that precluded treatment (defined as <4 mm diameter, <20 mm length, or more than one main renal artery) were excluded. This trial has shown a significant reduction in BP of approximately 32/12 mmHg in the study group patients as opposed to an increase of 1/0 mmHg in the control group measured 6 months after the procedure. A difference between the groups had been recorded in office visits, home measurements and ABPM. No serious adverse effects such as dissection, severe worsening of renal function or renal artery stenosis were documented (21). The 3-year follow-up results of these two trials had shown long-term efficacy achieving a reduction in SBP of over 30 mmHg and in DBP of 13 mmHg as compared to baseline, and an overall good safety profile with only one recorded dissection and two cases of kidney injury which had resolved (22,23). The promising results of these initial trials had driven the industry to develop various other devices for catheter-based RDN, such as second-generation radiofrequency catheters with multi electrodes which allow a faster and more thorough ablation, internal and external ultrasound therapies, chemical ablations and cryotherapy. Yet, at the same time, some concerns regarding the Symplicity trials have been expressed: (I) the trials were not blinded; (II) no sham-controlled design; (III) secondary causes for HTN were not excluded; (IV) neither adherence to medications nor guidelines-based pharmacotherapy had been ensured; (V) BP measurements were a mixture of office and ambulatory measurements; and (VI) reno-vascular safety had not been completely characterized. These concerns, on top of incomplete data regarding optimal sites for ablation, heterogeneity in response, and lack of data on the durability of the procedure after more than three years had proven to be the catalyst in the design and execution of the Symplicity HTN-3 trial (24). In this trial, patients with resistant HTN were randomly assigned to RDN therapy or a sham-controlled procedure. Both, patients and BP assessors were blinded to the procedure. The BP was recorded in the office and at home, patients had to be taking maximally tolerated doses of three or more antihypertensive medications of complementary classes. Clinical exclusion criteria were known secondary causes of HTN and more than one hospitalization for a hypertensive emergency in the previous year. Anatomical exclusion criteria were renal artery stenosis of more than 50%, renal artery aneurysm, prior renal artery intervention, multiple renal arteries, a renal artery of less than 4 mm in diameter, or a treatable segment of less than 20 mm in length. Notably, this trial failed to show a significant reduction in BP in patients with resistant HTN 6 months after RDN as compared to the sham-controlled arm (24). The 12-month report reconfirmed these findings (25). The results of this trial had a detrimental effect on the prospect of RDN, yet other trials published at the time did manage to show the potential benefit of RDN therapy when attention was paid to the medication regimen and to ABPM measurements (26,27).
The surprising results of Symplicity HTN-3 had become the focal point of many debates which led to the expression of several concerns: (I) adherence to medications was not monitored; (II) trial medications were not standardized nor they were prescribed according to guidelines; (III) about 40% of trial participants required changes in medications for various reasons with an unknown effect on outcome (28); (IV) unique population with severe resistant HTN treated with at least five different drugs, owing the fact that US-only population has a high prevalence of African American and obese patients (28); (V) lack of standardization with regards to the procedure including operator experience, number of ablations per artery and their locations.
These reservations were addressed in the design of the SPYRAL HTN-OFF MED trial (29). This trial recruited patients with mild to moderate HTN defined as office SBP ≥150 and <180 mmHg and/or DBP ≥90 mmHg or mean SBP on 24-hour ABPM measurement ≥140 and <170 mmHg. The main goal of the trial was to evaluate RDN therapy in the absence of any antihypertensive medication compared to a sham-controlled population. Prior to randomization, patients underwent a washout period of 3 to 4 weeks. Patients in both arms had similar baseline characteristics including baseline BP. RDN therapy was applied using the Symplicity Spyral multi-electrode catheter (Medtronic, Galway, Ireland) and the Symplicity G3 (Medtronic, Minneapolis, MN, USA) generator. This catheter consists of a four-electrode catheter that is positioned to deliver circumferential radiofrequency energy and thus, cover the four quadrants of the renal artery and branch vessels (29). At 3 months of follow-up, the RDN group had shown statistically significant decrease in BP measurements in comparison to the sham-controlled group. Of note, these changes were quite modest with only 5 and 4.4 mmHg difference in SBP and DBP ambulatory measurements, respectively, between the RDN group and the sham one. Office measurements had shown a larger difference between the groups with a drop in SBP of 7.7 mmHg and DBP of 4.9 mmHg favoring the RDN group. No adverse events were recorded (29). Table 1 summarizes data on clinical outcomes in Medtronic-sponsored trials.
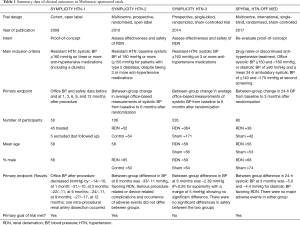
Full table
Discussion
Although anti-hypertensive medications are effective, adherence is low and some patients are found, or simply “tagged”, to be resistant to treatment. In this setting, a new innovative method to control HTN would be considered a game changer. Targeting the sympathetic nervous system and specifically the fibers enervating the kidneys had been shown to work in the past in a surgical approach. The mental leap that was taken to adjust this treatment to modern era with catheter-based technology seemed to have considerable potential. On top of that, previous evidence suggests additional benefits in terms of improvements in arrhythmias burden and obstructive sleep apnea, reversal of left ventricle hypertrophy and diastolic dysfunction, renal protection and improvement of glucose tolerance (30-33).
Even if initial trials results were promising, the results of Symplicity HTN-3 had undoubtedly changed the perception of RDN amongst the medical community. Almost a decade after the first proof-of-concept trial started, a full circle had been made with a renewed proof-of-concept SPYRAL HTN-OFF MED trial (29). This trial had succeeded to show a significant benefit 3 months after RDN therapy with regards to the primary end-point of office BPs and 24-hour ABPM. Yet, as stated before, the effect of RDN was quite modest and may raise the question of whether an invasive procedure is justified in this setting. Furthermore, many trials have shown that even in patients who are considered to have resistant HTN, this can often be attributed to low adherence to medical therapy (34).
Future perspectives for RDN
The RADIANCE-HTN and REQUIRE studies are multicenter, blinded, randomized, sham-controlled trials designed to assess the BP-lowering efficacy of the ultrasound-based Paradise RDN system (ReCor Medical) in patients with established HTN either on or off antihypertensive medications (35). There will be 2 cohorts, the SOLO cohort including patients with essential HTN at low cardiovascular risk, and either controlled with 1 to 2 antihypertensive medications, or uncontrolled on 0 to 2 antihypertensive medications. The TRIO cohort includes patients with resistant HTN on at least 3 antihypertensive medications (including a diuretic). The primary endpoint is the reduction in daytime ambulatory systolic BP at 2-month follow-up. The REQUIRE is designed to evaluate patients with resistant HTN on standard of care medication in Japan and Korea. The primary endpoint is reduction in systolic BP on 24-hour ABPM assessed at 3-month of follow-up (35). The results of both studies are expected in 2018.
Conclusions
The data provided by the SPYRAL HTN-OFF MED trial further contribute with another piece to the puzzle and, although not convincing to consider RDN as an alternative, stand-alone therapy, it may allow keeping the gate ajar for further research in the field of catheter-based RDN for the treatment of HTN.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- WHO. Global Report on Hypertension. 2013. Available online: https://hcupnet.ahrq.gov/#setup. Accessed on December 12th 2017.x
- Lim SS, Vos T, Flaxman AD, et al. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990-2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet 2012;380:2224-60. [Crossref] [PubMed]
- Lewington S, Clarke R, Qizilbash N, Peto R, Collins R. Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies. Lancet 2002;360:1903-13. [Crossref] [PubMed]
- Ettehad D, Emdin CA, Kiran A, et al. Blood pressure lowering for prevention of cardiovascular disease and death: a systematic review and meta-analysis. Lancet 2016;387:957-67. [Crossref] [PubMed]
- Whelton PK, Carey RM, Aronow WS, et al. ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension 2017.2017. [Epub ahead of print]. [PubMed]
- SPRINT Research Group, Wright JT Jr, Williamson JD, et al. A randomized trial of intensive versus standard blood-pressure control. N Engl J Med 2015;373:2103-16. [Crossref] [PubMed]
- Mancia G, Zanchetti A. White-coat hypertension: misnomers, misconceptions and misunderstandings. What should we do next? J Hypertens 1996;14:1049-52. [Crossref] [PubMed]
- Fagard RH, Cornelissen VA. Incidence of cardiovascular events in white-coat, masked and sustained hypertension versus true normotension: a meta-analysis. J Hypertens 2007;25:2193-8. [Crossref] [PubMed]
- Mancia G, Facchetti R, Bombelli M, et al. Long-term risk of mortality associated with selective and combined elevation in office, home, and ambulatory blood pressure. Hypertension 2006;47:846-53. [Crossref] [PubMed]
- Clement DL, De Buyzere ML, De Bacquer DA, et al. Prognostic value of ambulatory blood-pressure recordings in patients with treated hypertension. N Engl J Med 2003;348:2407-15. [Crossref] [PubMed]
- Dolan E, Stanton A, Thijs L, et al. Superiority of ambulatory over clinic blood pressure measurement in predicting mortality: the Dublin outcome study. Hypertension 2005;46:156-61. [Crossref] [PubMed]
- Schmieder RE, Ott C, Schmid A, et al. Adherence to antihypertensive medication in treatment-resistant hypertension undergoing renal denervation. J Am Heart Assoc 2016;5:e002343. [PubMed]
- Perreault S, Dragomir A, Roy L, et al. Adherence level of antihypertensive agents in coronary artery disease. Br J Clin Pharmacol 2010;69:74-84. [Crossref] [PubMed]
- Blaschke TF, Osterberg L, Vrijens B, et al. Adherence to medications: insights arising from studies on the unreliable link between prescribed and actual drug dosing histories. Annu Rev Pharmacol Toxicol 2012;52:275-301. [Crossref] [PubMed]
- Mancia G, Fagard R, Narkiewicz K, et al. 2013 ESH/ESC guidelines for the management of arterial hypertension: the Task Force for the Management of Arterial Hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). Eur Heart J 2013;34:2159-219. [Crossref] [PubMed]
- Daugherty SL, Powers JD, Magid DJ, et al. Incidence and prognosis of resistant hypertension in hypertensive patients. Circulation 2012;125:1635-42. [Crossref] [PubMed]
- Esler M. The sympathetic nervous system in hypertension: back to the future? Curr Hypertens Rep 2015;17:11. [Crossref] [PubMed]
- Grassi G, Mark A, Esler M. The sympathetic nervous system alterations in human hypertension. Circ Res 2015;116:976-90. [Crossref] [PubMed]
- Mompeo B, Maranillo E, Garcia-Touchard A, et al. The gross anatomy of the renal sympathetic nerves revisited. Clin Anat 2016;29:660-4. [Crossref] [PubMed]
- Krum H, Schlaich M, Whitbourn R, et al. Catheter-based renal sympathetic denervation for resistant hypertension: a multicentre safety and proof-of-principle cohort study. Lancet 2009;373:1275-81. [Crossref] [PubMed]
- Symplicity HTN-2 Investigators, Esler MD, Krum H, et al. Renal sympathetic denervation in patients with treatment-resistant hypertension (The Symplicity HTN-2 Trial): a randomised controlled trial. Lancet 2010;376:1903-9. [Crossref] [PubMed]
- Krum H, Schlaich MP, Sobotka PA, et al. Percutaneous renal denervation in patients with treatment-resistant hypertension: final 3-year report of the Symplicity HTN-1 study. Lancet 2014;383:622-9. [Crossref] [PubMed]
- Esler MD, Böhm M, Sievert H, et al. Catheter-based renal denervation for treatment of patients with treatment-resistant hypertension: 36 month results from the SYMPLICITY HTN-2 randomized clinical trial. Eur Heart J 2014;35:1752-9. [Crossref] [PubMed]
- Bhatt DL, Kandzari DE, O'Neill WW, et al. A controlled trial of renal denervation for resistant hypertension. N Engl J Med 2014;370:1393-401. [Crossref] [PubMed]
- Bakris GL, Townsend RR, Flack JM, et al. 12-month blood pressure results of catheter-based renal artery denervation for resistant hypertension: the SYMPLICITY HTN-3 trial. J Am Coll Cardiol 2015;65:1314-21. [Crossref] [PubMed]
- Rosa J, Widimský P, Toušek P, et al. Randomized comparison of renal denervation versus intensified pharmacotherapy including spironolactone in true-resistant hypertension: six-month results from the Prague-15 study. Hypertension 2015;65:407-13. [Crossref] [PubMed]
- Azizi M, Sapoval M, Gosse P, et al. Optimum and stepped care standardised antihypertensive treatment with or without renal denervation for resistant hypertension (DENERHTN): a multicentre, open-label, randomised controlled trial. Lancet 2015;385:1957-65. [Crossref] [PubMed]
- Kandzari DE, Bhatt DL, Brar S, et al. Predictors of blood pressure response in the SYMPLICITY HTN-3 trial. Eur Heart J 2015;36:219-27. [Crossref] [PubMed]
- Townsend RR, Mahfoud F, Kandzari DE, et al. Catheter-based renal denervation in patients with uncontrolled hypertension in the absence of antihypertensive medications (SPYRAL HTN-OFF MED): a randomised, sham-controlled, proof-of-concept trial. Lancet 2017;390:2160-70. [Crossref] [PubMed]
- Nammas W, Airaksinen JK, Paana T, et al. Renal sympathetic denervation for treatment of patients with atrial fibrillation: Reappraisal of the available evidence. Heart Rhythm 2016;13:2388-94. [Crossref] [PubMed]
- Fukuta H, Goto T, Wakami K, et al. Effects of catheter-based renal denervation on heart failure with reduced ejection fraction: a systematic review and meta-analysis. Heart Fail Rev 2017;22:657-64. [Crossref] [PubMed]
- Kampmann U, Mathiassen ON, Christensen KL, et al. Effects of renal denervation on insulin sensitivity and inflammatory markers in nondiabetic patients with treatment-resistant hypertension. J Diabetes Res 2017;2017:6915310.
- Mahfoud F, Cremers B, Janker J, et al. Renal hemodynamics and renal function after catheter-based renal sympathetic denervation in patients with resistant hypertension. Hypertension 2012;60:419-24. [Crossref] [PubMed]
- de Jager RL, van Maarseveen EM, Bots ML, et al. Medication adherence in patients with apparent resistant hypertension: findings from the SYMPATHY trial. Br J Clin Pharmacol 2018;84:18-24. [Crossref] [PubMed]
- Mauri L, Kario K, Basile J, et al. A multinational clinical approach to assessing the effectiveness of catheter-based ultrasound renal denervation: The RADIANCE-HTN and REQUIRE clinical study designs. Am Heart J 2018;195:115-29. [Crossref] [PubMed]


