Enhanced recovery after surgery protocols in video-assisted thoracic surgery lobectomies: the best is yet still to come?
Introduction
In the 1990s, a sequence of papers on fast-track programme in general surgery was published, showing a reduction of complications and the hospital length of stay (LOS). This knowledge is grown into a multidisciplinary tool usually known as enhanced recovery after surgery (ERAS) that assimilates numerous perioperative elements (ERAS protocols) (1). Presently, there are several official guidelines published by the ERAS Society for many specialities and several meta-analyses documented the benefits of ERAS. ERAS thinking involves a team of surgeons, anaesthesiologist, nurses, physiotherapists and dieticians with the aim to advance the quality of care by assimilating evidence-based knowledge into clinical practice (2-4). On the contrary, regarding thoracic surgery, up to now, there are no endorsed ERAS guidelines, and the papers supporting the benefits of modern perioperative management are partial. Most of the general principles used in other surgical disciplined may be applicable. Nevertheless, the existing results on ERAS pathways compared with traditional perioperative management of patients undertaking video-assisted thoracic surgery (VATS) lobectomy for cancer is still under debate. In addition, in a systematic review to summarise the evidence of ERAS in lung resections, authors identified only a small number of low-quality comparative studies. Some non-randomised studies yield encouraging results suggesting that ERAS may reduce primary LOS and hospitalisation costs, but they should be interpreted considering several methodologic limitations (1).
Developments of enhanced recovery pathways in VATS lobectomies
VATS lobectomies are safe and useful as a typical operation for early-stage lung cancer regarding the postoperative clinical stay. The expansion of an ERAS program in thoracic surgery was fewer than other specialities. Nevertheless, ERAS decreased postoperative complications and decreased the LOS. ERAS highlights the complete change within a hospital (5) (Table 1). Members of a team should assess the protocol at unequal intervals, assemble data to analyse variances with hindsight and attempt to advance the care progression. Nevertheless, handling variance also necessitates ongoing determination and perseverance, and it remains uncertain the timing of meeting and the developments to realised. Variances are rarely analysed in healthcare organisations that have applied clinical pathways due to the difficulties in creating definitions, classifying variance, and handling technology. It is essential to define critical events of conformance and outcomes to resolve these data management difficulties, identifying the critical procedures, result criteria and outcomes. These actions comprise compliance with the clinical pathway, timeliness, and types of dissimilarities from the pathway. The developments and use of the clinical pathway vary among groups, and the management differs among groups. Therefore, beginning clinical guidelines that the evaluation of the value or practicability of clinical pathways should be achieved (6). In a prospective, randomised, controlled pilot trial included lung resections cared using either a traditional treatment or a fast-track protocol, the fast-track group fasted for only 2 hours (7). By conducting daily physiological assessments, it was identified the daily rehabilitation time as crucial after VATS lobectomies (8). ERAS preoperative assessment from anaesthesiologist aimed to recognise high-risk patients, with the objective of optimising them before VATS, and for planning postoperative management. Preoperative reduced functional capacity is recognised risk factors for complications following thoracic surgery. Smoking addiction, ischaemic heart disease, peripheral vascular disease and renal impairment will frequently be seen. However, some interventions, which may not be ERAS part, may be required in advanced chronic conditions (5). As a fast track, VATS has become a well-known technique in the treatment of lung cancer, the planning of pain management should be tailored. Epidural patient-controlled analgesia and intravenous patient-controlled analgesia achieved the comparable efficacy of pain control for fast-track VATS lobectomy (9). The chest drainage pain decreases in VATS due to early removal of this pain-inducing device. VATS drops the surgical trauma due to no rib-spreading instruments, and smaller thoracotomy, with fewer drainage and, therefore, a smaller amount of fluid evacuation (10). It could be found in the literature some papers suggesting after VATS lobectomy the chest tube removal notwithstanding volumes of fluid <500 mL/day (11). Few patients developed pleural effusion requiring reintervention, and furthermost could be treated without hospital readmission and additional complications (11). In ERAS protocols, laboratory tests should be ordered when indicated, but routine use of tests may not be required. Although the length of hospital stays, postoperative testing, and the use of intensive care after VATS lobectomy has decreased, thoracic surgeons must pay attention to and further improve their outcomes. During these years, a minimalist approach was developed by some large volume groups (12). Chest roentgenograms in the recovery room and after drainage removal could be not necessary since the chest drainage is not an indication for a chest X-ray (12). Patients on the ERAS programme had a significantly reduced postoperative LOS and a better after a survey. It was calculated that ERAS project resulted in a net saving major than €235,000. The ERAS pathway has proven to be a safe perioperative management strategy without increasing postoperative morbidity or mortality (13). Even if used in elderly patients, ERAS protocols not increased the overall hospital LOS, and mean economic cost of treatment. The prevention of complications caused successful management of ERAS pathway. Clinical pathways are not a humble instrument in the management procedure without considerate the potential meaning or background of each step. Skill to predict variance is crucial to effective management while managing the variance disclosed by reviews is also indispensable. A new kind of global pathway was recognised as daily one-paged, continuous, multi-paged table with space for documentation along typical evolution. Also, collecting variance with the gateway method was applied in the early identification of critical conditions (6).
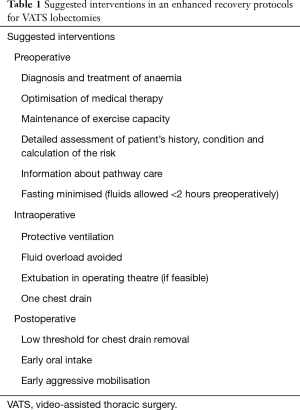
Full table
The “dark side” of ERAS pathways
As with the implementation of any change, there were barriers encountered during the implementation of ERAS program. There were safety concerns, concerns regarding having the appropriate staffing ratios to implement the program, concerns about patient compliance, and concerns about how the program would affect patients’ pain. Perhaps the most formidable barrier to implementation of the ERAS principles in minimally invasive thoracic surgery program was a concern for patient safety. When discussing barriers specific, it was described a lack of workforce and time as a barrier to implementation of ERAS principles. This issue was a barrier to implementation in our program as well. Overcoming this barrier required significant collaboration between hospital administrators and the leaders of the thoracic surgery team (7). A uniform approach to the perioperative care may yield benefits regarding reserve use and efficiency savings, also, to increase quality. Protocols that ensure reliable patient management lead to complications decrease and consequently overdue hospital discharge, enhancing the satisfaction of the patient. Selection and safety of patients are fundamental. It is probable that several thoracic surgery patients will be at high-risk for these protocols. A graded implementation process may be considered: fairly low-risk measures and patients first, then selected higher-risk patients after (14). On the contrary, it was recently demonstrated no benefit by the ERAS program on outcomes (complications, 30/90-days mortality, hospital LOS, and readmissions) (15). Therefore, ERAS recovery program elements may be insufficiently different from previous standards of perioperative care to confer detectable benefits. For patients undergoing VATS lung resection, it is possible that all patients now receive sufficient beneficial components of ERAS and that this should now be regarded as ‘‘standard’’ rather than ‘‘enhanced’’ care (15). The most significant progression in cost reduction will arise from the preoperative and intraoperative management standardisation, along with the previously recognised postoperative management. The lean process saves money and decrease variables removing fault and consequently improving quality (16).
Conclusions
In an era in which both patients and hospitals benefit from decreased hospital LOS, the ERAS techniques and interventions enable the patient to return more quickly to fully functional status while minimising many of the postoperative complications associated with thoracic surgery. In today’s healthcare environment, ERAS protocols can push past traditional barriers to create innovative strategies designed to deliver the highest quality care most cost-effectively. Application of thoracic surgery ERAS protocols seems to decrease postoperative complications and hospital LOS. Useful ERAS application involves proper sustenance, multidisciplinary participation and appropriate instruction for all subjects involved. Highly standardised management is of principal importance like the quick identification of not eligible patients. Nevertheless, we need for well-designed randomised clinical trials to provide the conclusive evidence about the role of the ERAS protocols in the VATS lobectomies.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Fiore JF Jr, Bejjani J, Conrad K, et al. Systematic review of the influence of enhanced recovery pathways in elective lung resection. J Thorac Cardiovasc Surg 2016;151:708-15.e6. [Crossref] [PubMed]
- Gustafsson UO, Scott MJ, Schwenk W, et al. Guidelines for perioperative care in elective colonic surgery: Enhanced Recovery After Surgery (ERAS®) Society recommendations. World J Surg 2013;37:259-84. [Crossref] [PubMed]
- Lassen K, Coolsen MM, Slim K, et al. Guidelines for perioperative care for pancreaticoduodenectomy: Enhanced Recovery After Surgery (ERAS®) Society recommendations. World J Surg 2013;37:240-58. [Crossref] [PubMed]
- Nygren J, Thacker J, Carli F, et al. Guidelines for perioperative care in elective rectal/pelvic surgery: Enhanced Recovery After Surgery (ERAS®) Society recommendations. World J Surg 2013;37:285-305. [Crossref] [PubMed]
- Giménez-Milà M, Klein AA, Martinez G. Design and implementation of an enhanced recovery program in thoracic surgery. J Thorac Dis 2016;8:S37-45. [PubMed]
- Okita A, Yamashita M, Abe K, et al. Variance analysis of a clinical pathway of video-assisted single lobectomy for lung cancer. Surg Today 2009;39:104-9. [Crossref] [PubMed]
- Schatz C. Enhanced Recovery in a Minimally Invasive Thoracic Surgery Program. AORN J 2015;102:482-92. [Crossref] [PubMed]
- Ueda K, Sudoh M, Jinbo M, et al. Physiological rehabilitation after video-assisted lung lobectomy for cancer: a prospective study of measuring daily exercise and oxygenation capacity. Eur J Cardiothorac Surg 2006;30:533-7. [Crossref] [PubMed]
- Yie JC, Yang JT, Wu CY, et al. Patient-controlled analgesia (PCA) following video-assisted thoracoscopic lobectomy: comparison of epidural PCA and intravenous PCA. Acta Anaesthesiol Taiwan 2012;50:92-5. [Crossref] [PubMed]
- Göttgens KW, Siebenga J, Belgers EH, et al. Early removal of the chest tube after complete video-assisted thoracoscopic lobectomies. Eur J Cardiothorac Surg 2011;39:575-8. [Crossref] [PubMed]
- Bjerregaard LS, Jensen K, Petersen RH, et al. Early chest tube removal after video-assisted thoracic surgery lobectomy with serous fluid production up to 500 ml/day. Eur J Cardiothorac Surg 2014;45:241-6. [Crossref] [PubMed]
- McKenna RJ Jr, Mahtabifard A, Pickens A, et al. Fast-tracking after video-assisted thoracoscopic surgery lobectomy, segmentectomy, and pneumonectomy. Ann Thorac Surg 2007;84:1663-7; discussion 1667-8.
- Scarci M, Solli P, Bedetti B. Enhanced recovery pathway for thoracic surgery in the UK. J Thorac Dis 2016;8:S78-83. [PubMed]
- Jones NL, Edmonds L, Ghosh S, et al. A review of enhanced recovery for thoracic anaesthesia and surgery. Anaesthesia 2013;68:179-89. [Crossref] [PubMed]
- Brunelli A, Thomas C, Dinesh P, et al. Enhanced recovery pathway versus standard care in patients undergoing video-assisted thoracoscopic lobectomy. J Thorac Cardiovasc Surg 2017;154:2084-90. [PubMed]
- Cerfolio RJ. Call it “fast tracking” or “enhanced recovery pathways”—no matter the name, it ain’t nothing new to thoracic surgeons. J Thorac Cardiovasc Surg 2017;154:2091. [PubMed]


