Three-dimensional (3D) bronchial tree model for bronchial resection with pulmonary segmentectomy
Introduction
Three-dimensional (3D) models are useful simulation tools to prepare for thoracic surgery, particularly bronchial stenting (1,2). In the last decade, there has been an increase in patients undergoing pulmonary segmentectomy because of increased numbers of small lung cancer and lung metastasis. However, it is sometimes difficult to determine the target bronchus correctly during surgery even if it is possible to use 3D computed tomography (CT) during preparation for the operation. To solve this issue, we used a 3D model as a simulation of pulmonary segmentectomy to investigate their use to simulate viewing a bronchial tree during surgery from multiple angles by mobilizing the lobes.
Case presentation
3D model
First, we used CT data to reconstruct a 3D digital model of the patient’s bronchial tree, creating a stereolithography file as the output. The model was directly printed using a 3D printer (Object260, Stratasys no.33201, Eden Prairie, MN) as previously described (3). The bronchial model was composed of a soft rather than hard material, similar to the actual bronchus. Furthermore, we made a cover for the peripheral bronchus, similar to the lung parenchyma, with a similar material to mimic the actual pulmonary lobe.
Case
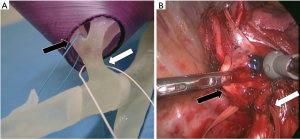
The patient was a 65-year-old woman with a partly solid tumor at segment 2 of the right upper lobe. This tumor was suspected as lung cancer, and the consolidation-tumor ratio was less than 50%. Therefore, we decided to perform a right S2 segmentectomy. The B2 bronchus can be difficult to determine for S2 segmentectomy, therefore, we made a 3D-printed model as a simulation before the operation. By using a bronchial model with a cover similar to lung parenchyma, we could mobilize the model as a simulation of the thoracoscopic surgery to see the bronchus from multiple angles from the caudal side (resembling the thoracoscopic view) (Figure 1).

Before the operation, we confirmed the view of the B2 bronchus, as well as the B1, B3, and B6 by using the 3D-printed model. We performed S2 segmentectomy via complete video-assisted thoracic surgery with one access window and three ports, and we dissected the bronchus during surgery. The camera was inserted at the port located at the 7th intercostal space on the middle axillar line, and the camera view was from caudal to cranial. After dissection of the target bronchus, we could confirm the positions of B2 and B3, which were very similar to the view using the simulation (Figures 1-3). We also confirmed the position of B2 with bronchoscopy before transection with a stapler. We also performed LN dissection, which was ND2a-1 including mediastinal lymph node. The chest tube was removed 2 days after operation. During and following surgery, the patient did not experience any complications. She stayed in hospital longer than usual because of social reasons and was discharged eight days after the operation. The pathological findings were adenocarcinoma in situ with no lymph node metastasis.
Comment
In the last few years, there has been a dramatic increase in the popularity of 3D printing and its application in many areas of medicine (1-3,6). In the simulation of surgery, 3D models offer several advantages, including the ability to visualize the situation using the patient’s specific anatomy. The model can be viewed from multiple angles from which you need to observe and touch the model, enabling the surgeon to distort organs as they would during the operation.
Pulmonary segmentectomy has become an increasingly important procedure for patients with lung cancer or metastatic lung tumors because these can be detected earlier than they could previously, and while still small and resectable (7-9). Technically, pulmonary segmentectomy is more difficult than pulmonary lobectomy because of the anatomic complexity. To expose the peripheral bronchus and vessels, we need to dissect the lung parenchyma, and we must mobilize and tense the pulmonary lobe during surgery. Furthermore, the lungs are collapsed in the chest cavity. As such, it is sometimes impossible to achieve the same view as seen in reconstructed 3D images from 3D CT scans.
We suggest that 3D-printed models may offer a practical solution to these problems. We tested the use of such a model for right S2 segmentectomy, and found it helpful because it was possible to view the bronchial location from the same angle as the thoracoscopic view (from caudal to cranial in our procedure). This is not possible with 3D CT scans. However, the usefulness of the model might depend on the specific case. Indeed, this simulation method may be more helpful for abnormal branches or sub-segmental resection, which are more complicated procedures. Nonetheless, the advantages of such a model may be great even for patients with standard branches.
Moreover, a more complicated 3D model incorporating vascular structure in addition to the bronchial tree may offer greater advantages. However, the vascular structure tends to be very similar to the images of enhanced 3D CT scans because the lung before transection of pulmonary arteries and veins is stable and relatively fixed at the same place as for CT imaging. This means that incorporating vascular anatomy may offer fewer benefits over simply modeling the structure of the bronchi.
However, some may doubt the advantages of such a model; we think that the model is not useful for all thoracic surgeons but for the relatively inexperienced surgeons because the surgeons with experience can simulate the operation by using virtual 3D imaging. The greatest advantage of this method is to be able to freely move the bronchus back and forth during a simulation as in a real-situation operation because the 3D images reconstructed using software have only a fixed bronchus. During the operation, we need to move the bronchus back and forth or to the right and left; these look different from the 3D images reconstructed by software. Therefore, 3D printing models can be useful to visualize the target bronchus when in movement during the operations. These may prove to be more useful for complicated segmentectomy although we have used it for right S2 segmentectomy in this paper.
The material from which the model is composed is also important to ensure it is useful. There are several types of material, from hard to soft, that are available depending on the 3D printing machine. In some printers, color materials are available, which could be helpful to identify different organs located nearby (10). Hard materials could make hard and stable 3D models that are longer lasting. In contrast, soft materials have the advantage of enabling modification of the shape, similar to how human tissues can be manipulated. This characteristic of the model is particularly important for use as a simulation of surgery operation. Thus, our preference is for soft materials in this preparation.
Additionally, the cost of a model is about 80–100 dollars, which includes only the cost of the material and does not include the initial cost of a 3D printer. However, the cost of the material and machine will certainly reduce with time as 3D printer are gaining popularity thus bringing down the initial cost for the machine.
We conclude that the novel use of a customized 3D-printed model based on patient specific data as a simulation can be used to confirm bronchus locations during pulmonary segmentectomy and may be helpful for surgeons, depending on the specific case. In particular, the model can increase the surgeon’s confidence that they had identified the appropriate bronchus during surgery.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this case report and any accompanying images.
References
- Matsumoto K, Yamasaki N, Tsuchiya T, et al. Double stenting with silicone and metallic stents for malignant airway stenosis. Surg Today 2017;47:1027-35. [Crossref] [PubMed]
- Miyazaki T, Yamasaki N, Tsuchiya T, et al. Airway stent insertion simulated with a three-dimensional printed airway model. Ann Thorac Surg 2015;99:e21-3. [Crossref] [PubMed]
- Baba M, Matsumoto K, Yamasaki N, et al. Development of a Tailored Thyroid Gland Phantom for Fine-Needle Aspiration Cytology by Three-Dimensional Printing. J Surg Educ 2017;74:1039-46. [Crossref] [PubMed]
- Matsumoto K, Yamasaki N, Tsuchiya T, et al. Surgical view of the right upper bronchus: dissection of the right upper bronchus and B2. Asvide 2018;5:378. Available online: http://www.asvide.com/article/view/23849
- Matsumoto K, Yamasaki N, Tsuchiya T, et al. View of the simulation using the 3D-printed model: simulation of determining the location of B2 by moving the right upper lobe using a 3D-printed model. Asvide 2018;5:379. Available online: http://www.asvide.com/article/view/23851
- Takagi K, Nanashima A, Abo T, et al. Three-dimensional printing model of liver for operative simulation in perihilar cholangiocarcinoma. Hepatogastroenterology 2014;61:2315-6. [PubMed]
- Donington JS. Current readings: sublobar resection for non-small-cell lung cancer. Semin Thorac Cardiovasc Surg 2013;25:22-9. [Crossref] [PubMed]
- Cao C, Gupta S, Chandrakumar D, et al. Meta-analysis of intentional sublobar resections versus lobectomy for early stage non-small cell lung cancer. Ann Cardiothorac Surg 2014;3:134-41. [PubMed]
- Gonzalez M, Ris HB, Krueger T, et al. Colorectal cancer and thoracic surgeons: close encounters of the third kind. Expert Rev Anticancer Ther 2012;12:495-503. [Crossref] [PubMed]
- Ventola CL. Medical Applications for 3D Printing: Current and Projected Uses. P T 2014;39:704-11. [PubMed]


