Femoro-jugular cannulation in veno-venous extracorporeal membrane oxygenation PRO/CON
In this technique, the artificial lung is in series with the failing native lungs. Thus, the decarboxylated and oxygenated blood goes through the native lungs decreasing the pulmonary vascular resistances and allowing protective mechanical ventilation. The fundament of veno-venous (VV) extracorporeal membrane oxygenation (ECMO) is to dissociate the oxygenation and the decarboxylation functions. Carbon dioxide (CO2) removal does not depend on blood flow in the ECMO circuit, conversely on the flow of the gas mixture through the membrane. By contrast, oxygenation depends on fraction of oxygen (FiO2) in the gas mixture and on ECMO flow. Oxygenation is not influenced by sweep gas flow. Therefore this system is based on a patient adequate circulation and cardiac function and it is indicated for isolated lung failure after optimization of the ventilatory support and the medical treatment (1-3).
Technical considerations: on VV ECMO, the main limiting factor is the oxygenation. To prevent this issue, largest cannulas should be used to decrease the circuit resistances with their tips as distant as possible, to reduce recirculation. Femoro-Jugular (F>J) VV ECMO requires the insertion of two cannulas, one is for blood drainage from the venous system [superior vena cava (SVC)] to ECMO circuit, the second returns the oxygenated blood to right atrium (RA) or left internal jugular vein (LIJV) (4,5).
This is a key factor for the variability of this strategy as multiple site access can be approached [right internal jugular vein (RIJV) being always the first option].
Indeed, acute lung injury (ALI) patients might present hostile anatomic characteristics making the cannulation difficult, venous thrombosis, central venous lines already placed or they could even need the addition of a second venous cannula to optimize drainage and increase flow.
On top of that, the direction of flow can be inverted from F>J to J>F in case of short SVC-RJV dictating cannula tip position in RA. Percutaneous position of femoral ECMO cannulas can be done at bedside in the hospital, in catheterization laboratory, in the intensive care unit (ICU) or emergency room and intraoperatively (Figure 1). This procedure is best performed with two operators to well check the cannulas and wires. The F>J approach is ideal in this perspective, as large bore short multistage cannulas provide the best hydrodynamic performance and the lowest recirculation. In general, all percutaneous cannulations should be accomplished with Seldinger’s technique and, if possible, under echocardiographic or fluoroscopic control. Long guidewires are forwarded, and the access is widened step by step with always more large dilators before advancing the cannula. An ultrasound estimation of the vessel size can be helpful (6-8). In our institution F>J cannulation is performed with HLS Maquet 35 cm multistage 25 Fr cannulas in the right femoral vein (RFV) and HLS Maquet 15 cm arterial 21–23 Fr cannula in the RIJV. Transesophageal echocardiography (TEE) monitoring is focused on guidewires navigation, especially in regard of suprahepatic vein accidental cannulation, which might lead to catastrophic complications. TEE also allows for visualization of venous return anatomy, the presence of atrial septal defect (ASD) or patent foramen ovalis (PFO), the assessment of right ventricular function and pulmonary artery pressure.

Right-sided venous access is the most reliable both for the IJV and FV as it has a straight course towards the target position and, possibly, overtakes the most common anatomical challenges for cannula navigation. Our group has shown that F>J and double lumen cannulation (DLC) do not differ in terms of hemolysis as long as blood flow is in the same range (9).
F>J is the ideal setting for patients who require high flow (>5 L/min), such as those with extreme hypoxemia and/or septic shock. Sometimes, despite a correct intravascular placement of the cannulas, the target flow could be achieved only by mean of a third drainage cannula. Furthermore, the right position of the cannulas is crucial to prevent recirculation of the oxygenated blood. Recirculation is a limitation of VV ECMO and is related to the blood flow rates and pump speed, the cannula type, size and position and direction of extracorporeal blood flow, in conjunction with intracardiac, intrathoracic, and intra-abdominal pressure (2).
The tips of the cannulas should be at the level of atrio-caval junction. Every time one is too close to the other, a large quote of the oxygenated blood is directed towards the venous cannula instead of being routed to the pulmonary artery causing a short circuit phenomenon. Recirculation may also occur as a result of increased VV ECMO flow as compared to native flow or as a result of an increase in intrathoracic or intracardiac pressure impeding venous return to the heart. This allows deoxygenated blood to be removed from the IVC and oxygenated blood to be returned to the SVC or RA (11,12). Recirculation may be diagnosed clinically (flashes of arterial blood in the drainage line) and quantified biologically comparing pre- and post-membrane blood gas, and patient central venous blood gas values. A rare complication is the compression of the inferior vena cava producing an abdominal compartment syndrome and so reducing venous back-flow (13).
F>J VV ECMO is the most efficient technique for respiratory support, especially in the case of high level of oxygen delivery (DO2) requirement. Rich et al. (14) demonstrated the superiority, in terms of oxygenation efficiency, of the drainage from the inferior caval system via a femoral cannula associated with the reinjection in the right atrium via the RIJV.
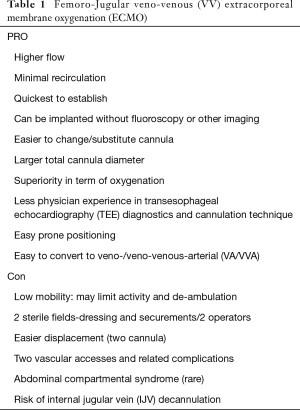
This technique is the most reliable way to quickly establish VV accesses, can be achieved quickly at the bedside also in an unstable patient and does not require radiographic imaging. Once the access is established in emergency situations in this fashion, the cannulation can be converted after 24–48 h to a double lumen cannula via the jugular vein. This allows removal of the femoral venous catheter and facilitates ambulation (1,6). Indeed, the disadvantage is that the femoral access may limit activity and ambulation (Table 1).
Full table
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Jayaraman AL, Cormican D, Shah P, et al. Cannulation strategies in adult veno-arterial and veno-venous extracorporeal membrane oxygenation: Techniques, limitations, and special considerations. Ann Card Anaesth 2017;20:S11-8. [Crossref] [PubMed]
- Montisci A, Maj G, Zangrillo A, et al. Management of refractory hypoxemia during venovenous extracorporeal membrane oxygenation for ARDS. ASAIO J 2015;61:227-36. [Crossref] [PubMed]
- Pappalardo F, Pieri M, Greco T, et al. Predicting mortality risk in patients undergoing venovenous ECMO for ARDS due to influenza A (H1N1) pneumonia: the ECMOnet score. Intensive Care Med 2013;39:275-81. [Crossref] [PubMed]
- Pavlushkov E, Berman M, Valchanov K. Cannulation techniques for extracorporeal life support. Ann Transl Med 2017;5:70. [Crossref] [PubMed]
- Sidebotham D, McGeorge A, McGuinness S, et al. Extracorporeal membrane oxygenation for treating severe cardiac and respiratory failure in adults: part 2-technical considerations. J Cardiothorac Vasc Anesth 2010;24:164-72. [Crossref] [PubMed]
- Lamb KM, Hirose H, Cavarocchi NC. Preparation and technical considerations for percutaneous cannulation for veno-arterial extracorporeal membrane oxygenation. J Card Surg 2013;28:190-2. [Crossref] [PubMed]
- Shaheen A, Tanaka D, Cavarocchi NC, et al. Veno-Venous Extracorporeal Membrane Oxygenation (V V ECMO): Indications, Preprocedural Considerations, and Technique. J Card Surg 2016;31:248-52. [Crossref] [PubMed]
- Rupprecht L, Lunz D, Philipp A, et al. Pitfalls in percutaneous ECMO cannulation. Heart Lung Vessel 2015;7:320-6. [PubMed]
- Pappalardo F, Ruggeri L, Pieri M, et al. Dual lumen catheter cannulation for venovenous ECMO. Intensive Care Med 2015;41:941-2. [Crossref] [PubMed]
- Kuhl T, Michels G, Pfister R, et al. Comparison of the Avalon Dual-Lumen Cannula with Conventional Cannulation Technique for Venovenous Extracorporeal Membrane Oxygenation. Thorac Cardiovasc Surg 2015;63:653-62. [Crossref] [PubMed]
- Broman M, Frenckner B, Bjällmark A, et al. Recirculation during veno-venous extra-corporeal membrane oxygenation--a simulation study. Int J Artif Organs 2015;38:23-30. [Crossref] [PubMed]
- Bartlett RH, Deatrick KB. Current and future status of extracorporeal life support for respiratory failure in adults. Curr Opin Crit Care 2016;22:80-5. [Crossref] [PubMed]
- Maj G, Calabrò MG, Pieri M, et al. Abdominal compartment syndrome during extracorporeal membrane oxygenation. J Cardiothorac Vasc Anesth 2012;26:890-2. [Crossref] [PubMed]
- Rich PB, Awad SS, Crotti S, et al. A prospective comparison of atrio-femoral and femoro-atrial flow in adult venovenous extracorporeal life support. J Thorac Cardiovasc Surg 1998;116:628-32. [Crossref] [PubMed]


